An outbreak of lethal infectious encephalitis killed more than 100 people in Western Malaysia during 1998–1999. The Nipah virus, a previously unknown paramyxovirus, was discovered to be the cause of the pig-borne epidemic.
1 The outbreak was first noted in late September 1998 and by mid-June 1999, more than 265 encephalitis cases, including 105 deaths, had been reported in Malaysia.
2,3 The virus appeared to be first introduced into pigs, where close contact caused by intensive farming practices led to pig-to-pig transmission, and subsequently pig-to-human transmission. In neighboring Singapore, which imports live pigs from Malaysia for slaughter, the outbreak was also limited to pig workers. Eleven workers in one of two Singaporean abattoirs developed Nipah-virus-associated encephalitis or pneumonia, resulting in one fatality.
4,5Neuroimaging studies using magnetic resonance imaging (MRI) have shown unusual multiple small lesions in the cerebral white matter in Nipah virus encephalitis, a pattern unlike other viral encephalitis.
6,7 In the study of late manifestation of Nipah virus infections, Lim et al.
8 found one case of clinical depression as well as evidence of retinal and spinal cord involvement by the virus. Furthermore, there have been reports of relapse among Nipah virus patients in Western Malaysia.
9,10 Information about this novel pathogen is still emerging. Given that Nipah virus is a new cross-species zoonotic pathogen, its natural history and long-term effects are unknown. To our knowledge, this is the first report of the long-term neuropsychiatric sequelae of Nipah virus encephalitis.
RESULTS
In Singapore, 13 patients (12 men and one woman) were affected by the Nipah virus outbreak. One patient died of his disease (mortality rate of 7.7%), and of the 12 surviving patients, three were lost to follow-up or did not present for imaging or psychological assessment. Nine patients underwent neuropsychiatric interview and eight patients underwent neuropsychological testing. Of the nine patients studied, there were eight males and one female; eight Chinese and one Indian; five Singaporeans and four Malaysians. Their ages ranged from 24 to 55 years (mean=40.8, SD=10.9). Seven patients worked in the abattoir and were involved either in the slaughtering of pigs or in the cleaning and processing of the carcasses. Two subjects were pig farmers from Malaysia.
Eight of nine patients suffered from neurological deficits, psychiatric sequelae or cognitive impairment; only one made a complete recovery.
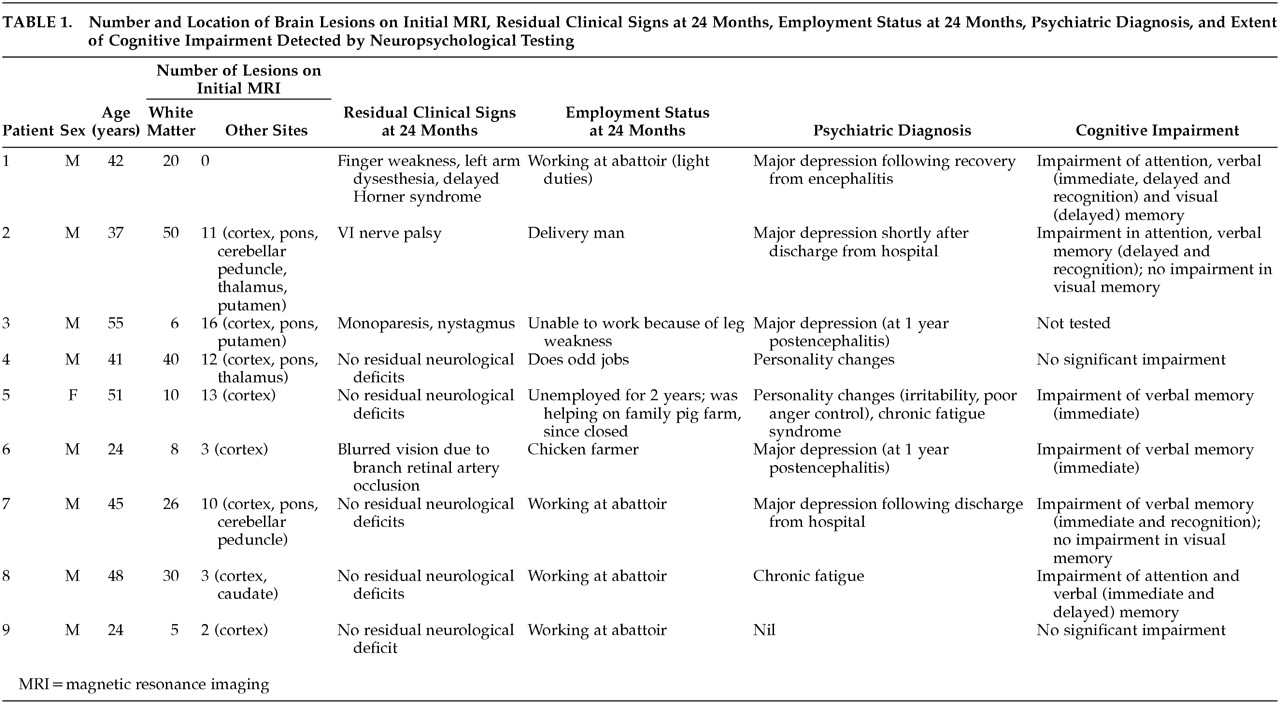
Table 1 summarizes the number and location of brain lesions on initial MR imaging, the residual clinical signs at 24 months, employment status at 24 months, psychiatric diagnosis, and extent of cognitive impairment detected by neuropsychological testing.
Psychiatric Complications
Five of the nine cases developed major depressive disorder following the encephalitis. These five cases all had cognitive and emotional symptoms of depression, like hopelessness, feelings of worthlessness and suicidal thoughts. Of the five, three became depressed shortly after their discharge from the hospital while two became depressed about 1 year after the outbreak. Four cases responded favorably to antidepressants therapy and supportive psychotherapy, while one patient refused psychiatric interventions and remained chronically depressed. There were two patients who developed personality changes, and two suffered chronic fatigue syndrome. Only one patient had no psychiatric diagnosis. Also, in this study, we found that four patients needed help coping with uncertainty. Although they had survived the initial critical period of viral encephalitis, many of them had complications arising from the illness, both physical and mental. Furthermore, recovering patients faced uncertainty and anxiety over reports of relapsed patients in Western Malaysia, although to date no such cases had been reported in the Singapore cohort.
Neuropsychological Testing
Eight patients were studied by neuropsychological testing. Of the eight subjects, four were estimated to have average premorbid functioning, two of low average functioning and two to be functioning within the borderline range. This estimation was based on their education and occupational background. Intellectually, five of the subjects were assessed to be functioning within their estimated premorbid level while the remaining three subjects were functioning at below the expected level.
Three subjects had impairment of attention. Five subjects had impaired immediate verbal memory. Three subjects had problems with delayed verbal memory and three of them had recognition memory problems. Of the eight subjects, two had verbal memory problems across the three domains, namely, immediate, delayed and recognition memories.
All of the eight subjects had no difficulty with immediate visual memory and performed within or well within their expected level. Only one subject was impaired on delayed visual memory. Contrasting verbal memory with visual memory, it appears that the subjects had more problems in verbal memory functions than with visual memory functions.
Occupational Status
Of the seven who were gainfully employed at 2 years postencephalitis, four resumed their work at the pig farms or abattoirs. Of the two patients who remained unemployed, one was unable to work because of leg weakness, while the other was severely affected by his fatigue and impaired memory.
Neuroimaging Findings
During the viral outbreak, all patients had multiple small lesions less than 1 cm in maximum diameter within the cerebral white matter. Although lesions were also found in the cortex, brainstem, cerebellum and deep nuclei, most patients had more lesions in the white matter than gray matter. Comparison between psychiatric and cognitive impairment and total number of brain lesions showed no discernible trends.
DISCUSSION
In Nipah virus encephalitis, the diversity and multifocality of neurological manifestations are particularly striking.
5 Histologically, widespread vascular endothelial infection and microinfarction have been demonstrated in Nipah virus infection,
2 and Lim et al.
7 have proposed that the lesions seen on MRI may represent vasculitic small vessel cerebral infarction. Our series of cases would be representative of the population of post-Nipah virus encephalitis patients. There are no selection biases that may have influenced the findings in this case series.
Psychiatric sequelae, especially depression, are common and constitute a major cause of disability following recovery from viral encephalitis caused by other viruses.
16 Depression, cognitive deficits, personality changes and chronic fatigue have been noted months after recovery. In our study, we found patients suffering from depressive symptoms, personality change, and chronic fatigue syndrome. None of our cases had mania, obsessive-compulsive disorder, or psychosis: these have been reported in other postencephalitis syndromes.
17,18We find that depression following Nipah virus encephalitis is phenomenologically indistinguishable from an idiopathic depressive disorder. Sadness, anhedonia, loss of energy, weight loss, insomnia, psychomotor agitation or retardation, feelings of worthlessness or hopelessness, diminished ability to concentrate, and thoughts of death or suicide are the characteristic features. In DSM-IV symptoms that are attributable to physical causes are not counted towards a diagnosis of major depression. Our five cases of major depression all had cognitive and emotional symptoms of depression, like hopelessness, feelings of worthlessness and suicidal thoughts. The origins of the mood changes are likely to be multifactorial, including brain dysfunction, functional incapacity, and role changes in society and in the family. The patient’s premorbid personality and adequacy of family support and social resources further condition the behavioral response to the brain disorder.
Two of our patients suffered from chronic fatigue. It seems probable that infection involving the central nervous system has a greater propensity to cause fatigue. Viruses are thought to cause organic brain syndromes in two ways—one is direct action of the virus within the CNS, the other is secondary to an autoimmune or hypersensitivity reaction to the virus either within or outside the CNS.
17We found neuropsychological testing helpful in fully delineating the extent of cognitive damage. Formal testing is extremely useful in assessing the patient’s cognitive limitations, in following the progress of the disease and in treatment planning. Despite their clinical subtlety, these deficits have significant practical implications for patients’ ability to return to their normal lifestyle.
18 It appears that the subjects in our study had more problems in verbal memory functions than with visual memory functions, and this pattern of verbal memory deficits may be a result of Nipah virus infection. However, an alternative explanation is that it could be easier for the subjects to compensate for visual memory loss than verbal memory loss and consequently, they had more problems in verbal memory functions.
The anatomical location of brain lesions in other organic brain diseases has been shown to be an important factor in determining which patients become depressed. Depression occurs most frequently in patients with lesions affecting the frontal and temporal lobes and the basal ganglia, particularly the caudate nuclei.
16 Additionally, the number and location of MRI lesions did not correlate with the severity of clinical findings in this study.
4 Therefore, the method of measuring lesion burden by counting the number of abnormalities visible on MRI may not be clinically useful in this new disease.