Eighty-six participants were recruited from five temporary-employment agencies in Los Angeles.
12,15 Psychopathy was assessed using the PCL-R
1 and supplemented by five sources of collateral data
15 to evaluate 20 distinct psychopathic characteristics (i.e., glibness/superficial charm, grandiose sense of self-worth, pathological lying, conning/manipulation, lack of remorse/guilt, shallow affect, callousness/lack of empathy, failure to accept responsibility for own actions, need for stimulation/proneness to boredom, parasitic lifestyle, poor behavioral control, promiscuous sexual behavior, lack of realistic long-term goals, impulsivity, irresponsibility, juvenile delinquency, early behavior problems, revocation of conditional release, many short-term marital relationships, criminal versatility). The collateral data included 1) the Interpersonal Measure of Psychopathy; 2) self-reported crime and violence assessed using an adult extension of the National Youth Survey self-report delinquency measure; 3) criminal history transcripts obtained from the Department of Justice; 4) data derived from, and behavioral observations made during, the Structured Clinical Interview for Axis I DSM-IV Disorders and Axis II Personality Disorders; and 5) independent IM-P ratings made by two different laboratory assistants during separate phases of testing.
15 Individuals diagnosed with a DSM-IV disorder (e.g., schizophrenia) other than antisocial personality disorder were excluded. A cutoff of 23 (high) and 15 (low) on the total PCL-R score was used to define psychopathy, resulting in a total of 27 individuals with psychopathy (PCL-R range: 23–40) and 32 comparison subjects (PCL-R range: 5–14). Additional demographic, diagnostic, and cognitive characteristics were assessed, including past/current substance dependence using DSM–IV and full-scale IQ (WAIS–Revised; WAIS–R).
15 The two groups did not differ in age, gender, ethnicity, handedness, or substance dependence.
12 This cutoff was chosen to be consistent with our previous research on this sample,
9,12,15 and is similar to the optimal cutoff suggested by taxometric analyses of the PCL-R.
16 Full informed, written consent was obtained from all subjects in accordance with Institutional Review Board procedures at University of Southern California.
12For each participant, structural MRI data were collected on a 1.5T Philips S15/ACS scanner (repetition time/echo time: 34 msec/12.4 msec; voxel size: 0.9×0.9×1.7 mm) and processed using a previously detailed cortical pattern-matching analysis.
12 Response perseveration was assessed using a computerized version of the WCST,
7 and standardized scores were computed for perseverative and nonperseverative errors.
9 We conducted a partial correlation analysis, examining the group difference in the performance scores of the WCST, and findings revealed that increased total PCL–R score correlated significantly with increased WCST perseverative (r=0.2; p=0.027) but not nonperseverative error scores (r=0.12, p=0.12) across the entire sample, while controlling for age and full-scale IQ.
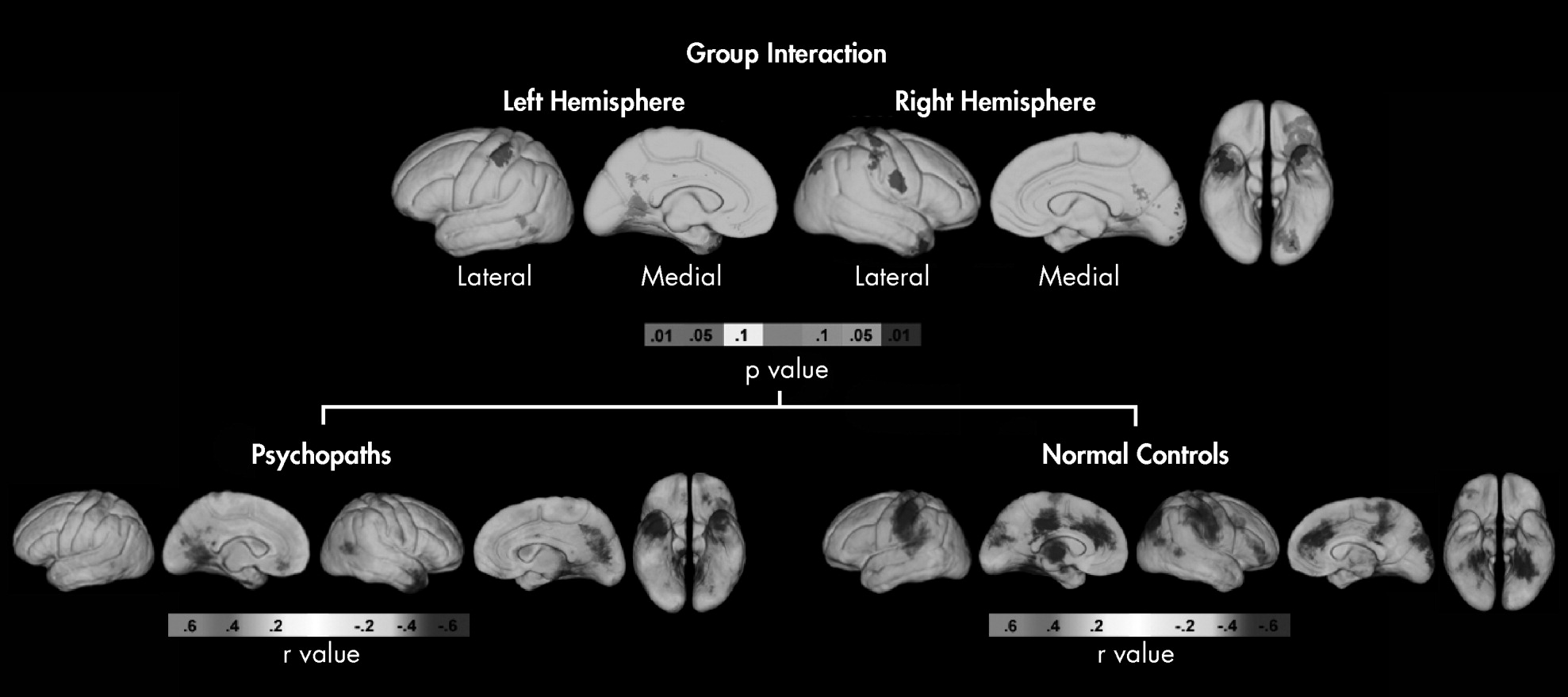
The General Linear Model, implemented with R (
http://www.r-project.org/), was used to determine whether associations between cortical thickness and WCST perseverative error scores differ between individuals with psychopathy and healthy-comparison subjects. Significant interaction effects were followed up by examining correlations between the WCST perseverative error scores and cortical thickness within groups separately while controlling for inter-individual variation in whole brain volume. Uncorrected two-tailed probability (p) or correlation (r) values obtained from statistical tests conducted for each cortical surface point were color-coded and displayed on the averaged cortical surface representations of the entire group to allow initial visualization of group differences. We performed permutation analyses, using masks of frontal and temporal regions of interest generated from an atlas
12 to control for multiple comparisons conducted on thousands of surface points, and corrected p values (two-tailed) were then reported. Given our previous hypothesis, findings outside of the prefrontal and temporal cortex were treated as exploratory.