Violence in psychiatric settings is a complex workplace problem. Frequent serious incidents have been reported in both prospective (
1) and retrospective studies (
2). In one study, 60 percent of psychiatric staff who had experienced violence felt that help was not readily available, 42 percent were dissatisfied with procedures after the incident, and 43 percent felt their work environment to be unsafe (
3).
Prediction studies have focused only on factors related to patients, the environment, or the staff and have not attempted to combine multiple factors into a single model to predict violence and aggression. Research has also been confounded by imprecise definitions of violence and aggression (
4) and the use of retrospective data (
5,
6). Mild incidents of violence such as verbal threats have been overlooked despite occupational health implications (
7). Patient factors found to be related to violence include being a young male with a diagnosis of schizophrenia (
8), particularly with neurological impairment (
9); having a history of violence (
10); and being involuntarily admitted to the hospital (
6,
11). Having a diagnosis of dementia or delirium (
12), substance abuse (
13), and personality disorder and bipolar disorder (
14) have also been shown to be related to violence.
Environmental factors such as overcrowding on wards has been linked with violence (
15,
16), perhaps via increased environmental stress (
17). Violence has been known to increase around mealtimes (
5), or when patients mix freely (
4). Bed reductions and the resulting proximity of aggressive patients have been related to increased violence (
18).
Research examining staff factors found that the incidence of violence was higher on wards where staff members were uncertain of their roles (
19) or where a larger proportion of shifts were worked by substitute nursing staff (
11). A higher staff-to-patient ratio has been found to be related to increased violence (
20). Fewer incidents occurred when the staff-to-patient ratio approached 1:1 (
16). Incidents rose when staff members set limits (
21,
22). Increased violence has been found to be associated with a lower level of experience among nurses (
23), new employee status (
24), or lack of staff training in aggression control techniques (
25).
This study brings together detailed information about violent and aggressive behavior in psychiatric hospital settings and focuses on the possible complex interaction between ward staffing, patient mix, and violence.
Methods
This study was conducted in five psychiatric settings in Sydney, Australia: three acute psychiatric units for adults located in a general hospital and two units—an acute adult admission unit and a psychogeriatric unit—in a primary psychiatric hospital. These facilities served a relatively affluent population of approximately 736,000 residents that constituted 12.4 percent of the population of the state.
For this study, aggression was defined as any threatening verbal or physical behavior directed toward self or others. Violence was defined as any physical behavior that resulted in harm to self or others. Violent incidents were defined using Morrison's hierarchy (
26) of aggressive and violent behavior. The classification ranged from level 1, inflicted serious harm to self or others requiring medical care, to level 8, exhibited low-grade hostility (see
Table 1).
Assessment tools
The Violence and Aggression Checklist, Ward Activity Index, and Staff Level Index were developed by the researchers based on the input of focus groups of mental health professionals.
On the Violence and Aggression Checklist, staff members used Morrison's hierarchy to rate each violent incident they observed. A violent episode in which a patient demonstrated several violent behaviors was rated based on the most serious behavior observed. Data included the patient's identification number, the date and time of the incident, the target(s) of the assault, the severity and method of the attack, and the outcome for the patient and victim.
On the Detailed Report of Aggressive Incidents, staff members rated serious incidents—levels 1 to 4 of Morrison's hierarchy—and recorded demographic and clinical data about the aggressive patient. The incident data included a description of the behavior, the warning signs, impact, and staff response.
The Ward Activity Index comprised items reported by staff focus groups that increase activity on the ward. Items included total patient numbers, demographic and diagnostic mix, number of new admissions, and the number of patients with a history of violence. It was completed weekly by the nursing unit manager. Items were summed for a total score per week.
The Staff Level Index included items about factors that enhanced staff members' accessibility to patients; these items, such as the numbers of staff on duty, were scored positively. Some items reflected factors that hindered staff's accessibility; these items, such as staff absenteeism, were scored negatively. Items included the number of rostered staff, years of experience, demographic mix, the actual number of staff on duty, and the use of staff from a temporary agency or replacement staff. The Staff Index Level was completed weekly by the nursing unit manager.
The reliability of incident reporting was assessed by comparing the returned instruments with the standard hospital injury-incident report forms. All tools are available from the first author.
Data collection
A staff member at each site was identified as a liaison to complete the weekly Ward Activity Index and Staff Level Index and to ensure best practice in recording all aggressive and violent incidents. Incidents were recorded once at the time of the incident, either by the victim, or if the victim was incapable, by the best witness.
Data were collected for three months in the two units located in the primary psychiatric hospital and for six months in the three acute psychiatric units in the general hospital. The data collection period was August 1995 to March 1996. The different data collection times reflected the high rate of patient admissions in the two units from which data were collected for three months. All reported violent incidents were included in the analysis, providing a total of 105 weeks of data.
Data analysis
The primary analysis examined violence in terms of incidents per week per occupied bed. Subscales from the Ward Activity Index and the Staff Level Index were extracted using principal components analysis and varimax rotation. Factors that explained substantial variance in the total scores of the respective index were then correlated with the number of violent incidents per unit per week per occupied bed. To examine relationships in stages, patient factors from the Ward Activity Index and staff factors from the Staff Level Index were each considered alone and then combined in a final model.
Formal analysis for the rate of violent incidents was conducted using exact methods via Poisson regression. As the dependent variable was a count, it may be assumed to follow a Poisson distribution. Because the number of violent incidents might be expected to increase with the patient population regardless of any other factor (
15), violence was examined in terms of the rate of violent incidents per bed-week, yielding a Poisson rate. Formal inference was via Poisson regression from which relative rates and 95 percent confidence intervals were obtained, in addition to p values.
Identification of statistically independent risk factors for violence used a backward stepwise selection process. Because this study explored an interactional hypothesis concerning correlates of violent behavior, statistical significance was set at p<.05 for all hypothesis tests. Consequently, our findings are suggestive rather than definitive. The secondary analysis of serious incidents used descriptive statistics, with the total number of serious incidents as the denominator, to examine the occupational health issues of violence and aggression in psychiatric units.
Results
The sample included all 855 patients who were admitted during 105 weeks of data collection. Average bed occupancy was 89 percent, with an equal number of men and women. Most patients were between the ages of 26 and 40 years. Half of the patients were involuntarily detained. More than half the patients in each study week had a diagnosis of schizophrenia or bipolar affective disorder.
Extent of violence and aggression
As shown in
Table 1, during the course of the study, 1,289 violent or aggressive incidents were perpetrated by 174 individuals. Most (752 incidents, or 58 percent) were rated in the four most serious categories, with nine life-threatening and one fatal incident. A small cohort of 20 patients caused 857 incidents (67 percent). (A separate paper in this issue addresses this group.) The mean±SD number of incidents per bed-week was .51±.67, with a range from zero to 3.33.
Most incidents occurred in the morning (424 incidents, or 33 percent) or evening (460 incidents, or 36 percent). Fewer incidents occurred at lunch (275 incidents, or 21 percent) or after midnight (130 incidents, or 10 percent). Most aggression or violence was directed toward staff members (1,029 incidents), followed by property (220 incidents), other patients (174 incidents), self (46 incidents), family (25 incidents), and visitors (14 incidents).
The response to most incidents was counseling (732 incidents). Other responses included medication (357 incidents), removal from the immediate area (272 incidents), physical restraint (242 incidents), and seclusion (74 incidents). Only a few responses involved transfer to a different facility (15 incidents). No further action was taken in 160 incidents (12 percent). (These response categories are not mutually exclusive.)
Organizational issues
Of the 1,289 incidents identified, 752 were rated as serious, and organizational issues were examined. Most of these incidents (619 incidents) were preceded by a warning sign, commonly agitation. Targets of the serious incidents included nursing staff (587 incidents), fellow patients (137 incidents), property (113 incidents), self (45 incidents), physicians (30 incidents), psychologists (15 incidents), family members (15 incidents), and domestic staff (eight incidents). (The target categories are not mutually exclusive.) On 69 occasions a weapon was used. Three staff members took time off from work, citing the incident as the reason.
Serious incidents were responded to by nursing staff (743 incidents), doctors (65 incidents), psychologists (21 incidents), police (five incidents), or others (16 incidents). (These response categories are not mutually exclusive.) The occupational health and safety officer was notified in 17 of the 752 serious incidents, and a formal incident-injury report form was completed on 173 occasions. Reports were written as often for level 1 as level 4 incidents.
Staffing level and case mix
Three subscales that accounted for 49 percent of the variance in the Staff Level Index were identified using factor analysis. Factor 1 appeared to measure nursing staffing practices. The items that loaded above .5 were the number of female nursing staff on the roster that week, nursing staff without specific psychiatric training, and the presence of nursing staff with specific training in dealing with aggression. The number of students attached to the ward loaded negatively to this factor. Factor 1 had a moderate correlation with the number of violent incidents per occupied bed (Spearman correlation coefficient= .41, p<.001).
Factor 2 also reflected staffing matters. The three items that loaded above .5 were the number of male nurses, the number of senior nursing staff, and the number of staff members who were less than 30 years of age on the roster that week. The number of male nurses loaded negatively to this factor. Factor 2 had a negative correlation with the number of violent incidents per occupied bed (Spearman correlation coefficient= -.29, p=.003).
Factor 3 appeared to measure staff absenteeism. The number of nonnursing staff on planned leave loaded above .5, and unplanned nursing absenteeism loaded negatively. Factor 3 had a weak positive correlation with the number of violent incidents per occupied bed (Spearman correlation coefficient=.22, p=.02).
Table 2 shows staff-related factors found by the Poisson regression model to be independently and significantly associated with violent incidents. The factors were more staff on duty who lacked specific psychiatric training, students on the ward, more nursing staff on duty (either men or women), more senior nurses on duty, and the planned absence of nonnursing staff. More staff under age 30 was associated with a decrease in the relative risk of violence. Together these factors accounted for 78 percent of the variance in the Staff Level Index.
Number and mix of patients
Factor analysis found two factors within the Ward Activity Index that accounted for 46 percent of the variance in the index score. Factor 1 appeared to measure total ward load. The items that loaded above .5 were the number of occupied beds, male patients, physically sick or disoriented patients, patients with a history of violence, and patients cared for in ward areas with increased security.
Factor 2 appeared to measure the difficult caseload of the ward. The items that loaded above .5 were the number of patients between the ages of 26 and 40; patients with acute psychotic illness, personality disorder, or substance abuse problems; and the number of patients who had been involuntarily admitted. Only factor 1 had a positive correlation with the number of violent incidents per occupied bed (Spearman correlation coefficient=.58, p<.001). Factor 2 was not significantly correlated.
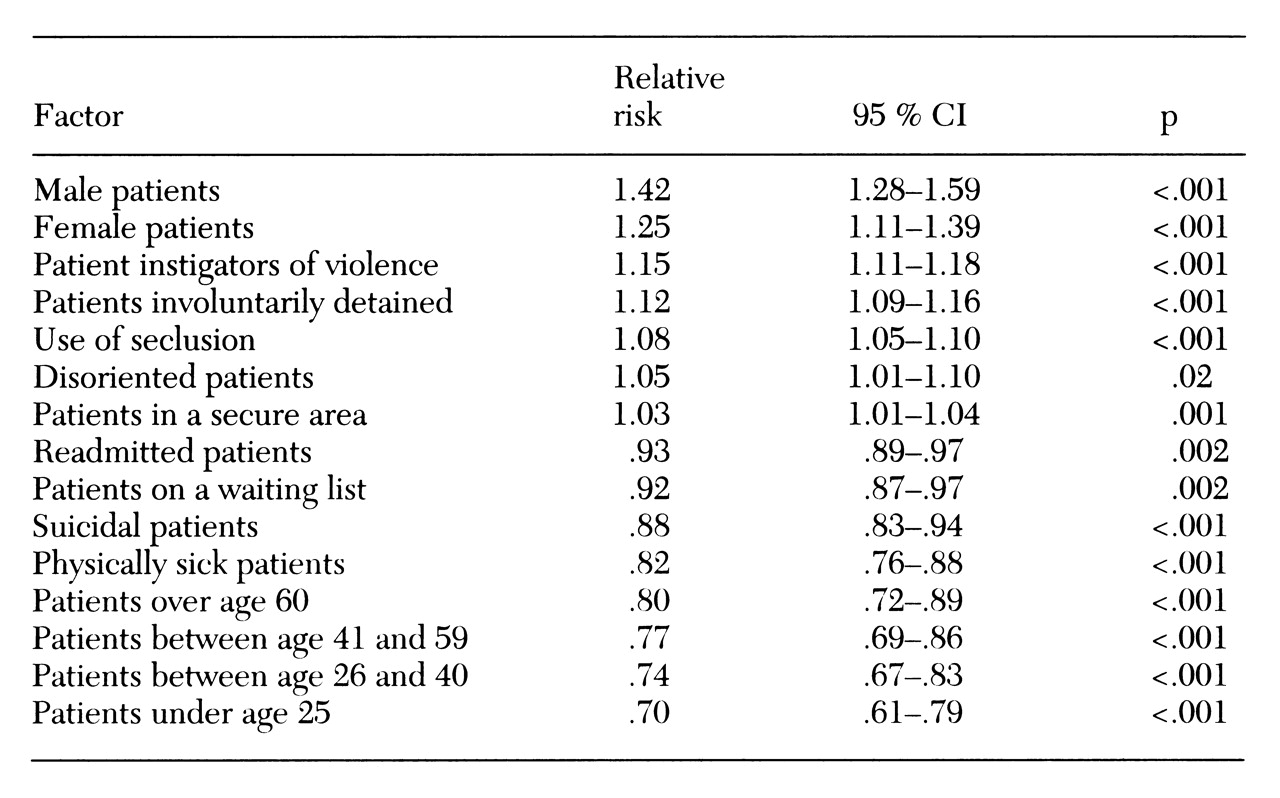
Table 3 shows factors from the Ward Activity Index found by the Poisson regression model to be independently and significantly associated with violent incidents. They were increased number of patients (both male and female), patients detained involuntarily, disoriented patients, increased use of seclusion, more patients in the secure area of the ward, and the presence of known instigators of violence. The following factors were significantly associated with a decrease in the relative risk of violent incidents: patients on the waiting list, physically sick patients, suicidal patients on the ward, and patients who had returned to the ward after being discharged within the last month. The relative risk analysis of patient age groups revealed that younger patients (less than 25 years old) had the greatest negative association with the risk of violence. Together these 15 factors were found to account for 78 percent of the variance.
Staffing level and patient mix
Finally, items from both the Staff Level Index and the Ward Activity Index were entered into a Poisson regression model to examine the impact of both staffing and patients on the relative risk of violence. As
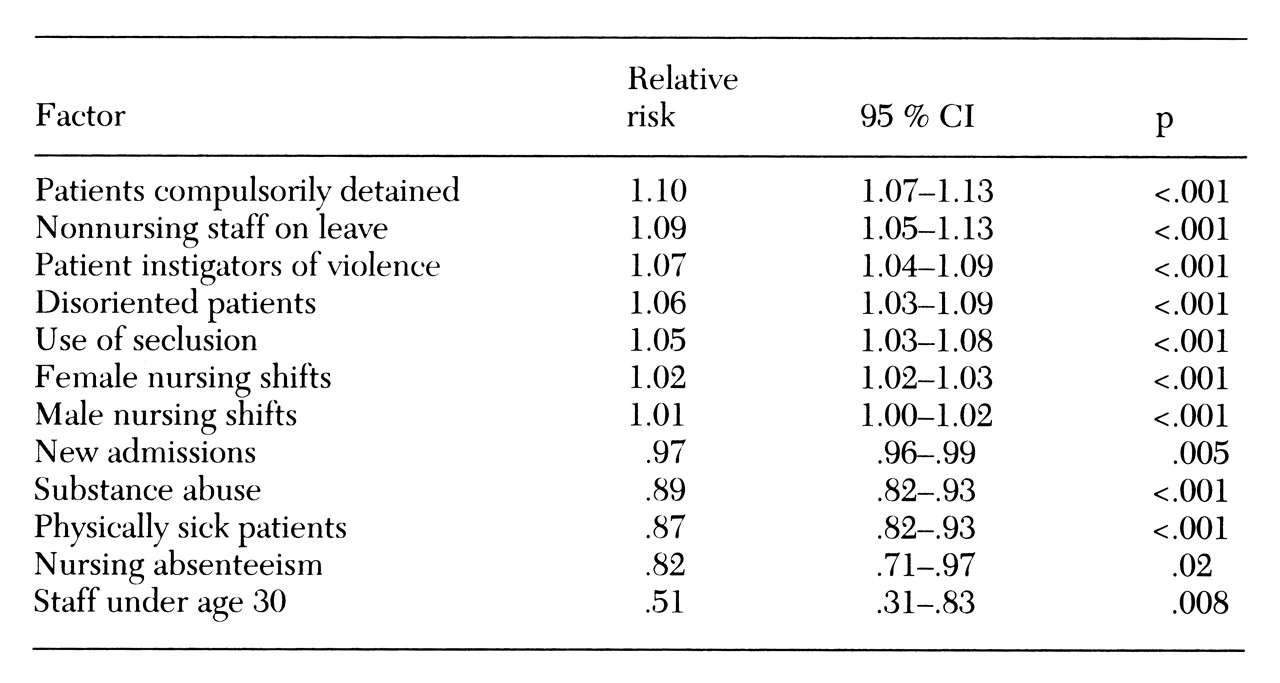
Table 4 shows, relative risk increased with more nursing staff (of either sex), more nonnursing staff on planned leave, more patients known to instigate violence, a greater number of disoriented patients, more patients detained involuntarily, and more use of seclusion. The relative risk decreased with more young staff (under 30 years old), more nursing staff with unplanned absenteeism, more new admissions, and more patients with substance abuse or physical illness. In total these factors accounted for 62 percent of the variance in violence.
Discussion
Some of the methodological difficulties of earlier work about violence are overcome in this study by the use of a prospective design, a standard definition of violence, a rating system that distinguished between physical incidents and verbal threats (the latter are often neglected in research studies), and specified targets of incidents (such as property as well as persons). The interplay of patient and staff factors in relationship to violence was examined.
Violent incidents were found to be frequent, averaging .5 incidents per week per occupied bed, and ranging from no incidents to 3.3 incidents. Other investigators reported one incident per bed every five days (
27). In our study, most incidents (58 percent) were serious, and some involved a weapon. Our finding that 174 patients were involved in 1,289 incidents is similar to results of other work (
1) in which a few patients cause a large number of incidents (
2,
5,
28).
Violence and aggression are a substantial occupational health issue. In this study, nursing staff were the most common target of assaults. Nursing staff members almost always responded to an incident of aggression or violence, which may be due to their expertise, greater proportion on the staff, and availability. However, this finding may suggest that other back-up resources, such as security staff, or other health professionals, such as medical staff, were unavailable, untrained, or unwilling to respond.
Substantial morbidity was documented for victims of violence and aggression, with harm occurring in 45 percent of incidents. However, rarely were the appropriate occupational health and safety personnel notified, and a formal report of the incident was made to hospital administration in less than a quarter of the incidents. More serious incidents were reported with no more frequency than less serious ones, which suggests that official data about violence and aggression very likely understate the true incidence, and that staff in some way tolerate a large number of incidents without reporting the details to the administration. This disparity in reporting was at odds with previous studies that found the documentation of episodes of violence to increase with the severity of the act (
25).
Three-quarters of the serious incidents in our study were preceded by some warning sign, particularly agitation. A previous study reported that 85 percent of incidents were considered spontaneous (
1). Our finding suggests that warning signs may often exist but may be difficult to identify and interpret—and perhaps are seen only in hindsight.
Two models were used to examine the relative risk of violence and aggression in psychiatric units—ward activity and staff level. A significant positive relationship was found between violence and a factor reflecting total ward load identified in the ward activity measure. In this study as in other work (
2,
13), a larger number of patients on the ward (particularly male patients) and patients with a past history of violence increased the risk of violence. Unlike earlier work, this study found that younger patients (under age 25) reduced the risk of violence. Suicidal or physically sick patients also reduced the risk, perhaps reflecting that these patients' concerns were more self-focused.
The relationship between staffing and violence was not clear. Three factors—more female staff, more staff without psychiatric training or aggression training, and more staff absenteeism—had a positive relationship with violence, whereas two additional factors—younger staff and staff with higher levels of psychiatric expertise—had a negative relationship with violence. A larger number of staff members have been linked to increased violence in other studies (
20), perhaps because of increased stimulation and limit setting. Other investigators have found that higher staffing levels are a response to violence (
23,
24). The greater number of staff may simply have allowed staff members to notice and record more violent incidents.
Staff absenteeism has been linked with increased violence and may be a cause or effect of increased violence and aggression (
29,
30). Students on the ward were associated with an increase in the risk of violence, perhaps because students made more contacts with patients or because staff members' time was occupied in training students. This finding suggests that having extra staff to provide adequate supervision for students on placement is an important issue.
This study combined staff and patient factors in a final model to examine the prediction of violence and aggression. The factors that increased the relative risk of violence included some recognized in earlier univariate research—a history of violence, involuntary admission, increased nursing staff, and planned absences by nonnursing staff (
10,
20,
31). Factors associated in our study with a decrease in the relative risk included several new findings—younger staff, increased absenteeism among nursing staff, patients' substance abuse, and patients' physical illness.
Based on these findings, several strategies for managing violent behavior in psychiatric settings could be developed. Given that warning signs preceded most incidents, staff training programs could target early recognition of warning signs of violence and aim to institute early verbal de-escalation procedures (
32). Few patient factors remained significant in the prediction model when both patient and staff factors were considered. A history of violence continues to be a factor that can aid in the early identification at admission of those at risk of violence and aggression. In other work (
33), incidents against staff were reduced by 92 percent by identifying patients with a history of violence, making staff members immediately aware of this information, and planning appropriate treatment.
The seriousness of the incident did not guarantee that it was reported according to occupational health and safety guidelines. Substantially more incidents were identified with the study tools than were reported to the administration. It may be that having to complete the reports for the study caused staff not to complete the "official" violence reports. However, the rates of violence according to official data at these institutions did not vary before or after the study period. This finding suggests a real deficit in institutional data. To improve accuracy, occupational health data collection may need to be simplified and to be seen by staff as a real tool in the development of interventions in each work setting.