Previous studies have identified characteristics of cohorts of repetitively violent patients who perpetrate a disproportionately large number of violent and aggressive incidents. Usually the studies define recidivism as three or more incidents by one patient, and data examination is retrospective. In one study in a state mental hospital, 15 young patients who had severe symptoms that were unresponsive to treatment and who had been hospitalized for more than four years accounted for 49 percent of violent incidents (
4). Another study found that 12 patients, mainly with neurological impairment, were responsible for 68 percent of 834 violent incidents in an inpatient psychogeriatric unit (
5). Kennedy and colleagues (
2) found that 27 patients, or 8 percent of the sample, accounted for 705 violent incidents, or 72 percent of the total incidents. Noble and Rodgers (
6) described a recidivist group that was younger, more psychotic, and more seriously violent.
Other studies have characterized recidivist patients as showing warning signs (
7), having a history of violence and aggression (
2,
6,
8) and multiple psychiatric hospitalizations (
6), being younger (
2,
9), having neurological impairments such as dementia (
5,
8,
101112) and diagnoses of schizophrenia (
2,
5,
6,
13) and personality disorder (particularly among women) (
12,
13,
14), and being involuntarily admitted to the hospital (
6,
13,
15).
The nature of recidivist violence has also been examined. Incidents by recidivist patients have been found to be directed at nursing staff (
1,
3,
5,
16); to be serious, involving vital body areas (
2); to be potentially life-threatening attacks (such as strangulation) (
1,
3); and to involve deliberate self-harm or attempted suicide (
11,
12). Recidivist incidents have been found to include destruction of property (
2) and use of dangerous weapons (
1). The recidivist violence identified in general psychiatric settings resembles that seen in forensic settings and other criminal facilities (
11,
17,
18).
Methods
Data on violent and aggressive incidents were collected over a seven-month period (August 1995 to March 1996) in five psychiatric units in Sydney, Australia (
1). The data were pooled to examine recidivism. Recidivism was defined as 20 or more violent and aggressive incidents by one person. Violence and aggression was defined using Morrison's hierarchical definition of violent and aggressive behaviors among psychiatric inpatients (
21).
Morrison's hierarchy describes violence and aggression on an 8-point continuum from level 1, inflicted serious harm to self or others requiring medical care, to level 8, exhibited low-grade hostility. Aggression was defined as any threatening verbal or physical behavior directed toward self or others. Violence was defined as any physical behavior that resulted in harm to self or others. To keep the focus on serious violence and aggression, this study examined incidents reflecting the four most serious levels from Morrison's hierarchy—level 1, violence requiring medical care, to level 4, threatening touch (see
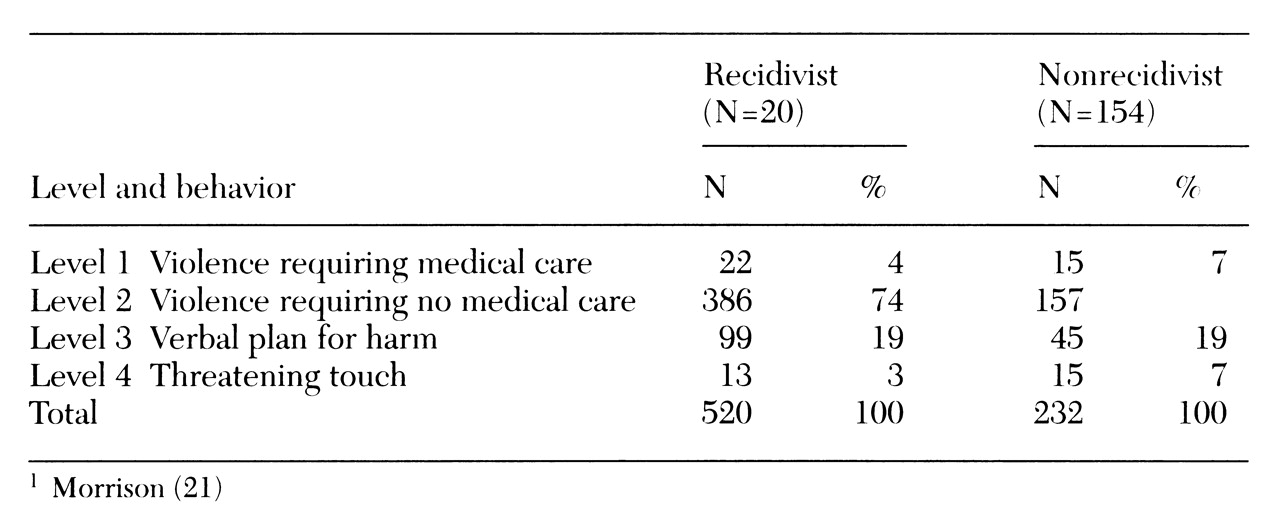
Table 1). Information about patients' demographic characteristics was recorded for each incident, and the incident was described, including the warning signs, impact, and staff response to the incident.
Violent incidents by recidivist patients were compared with those by nonrecidivist violent patients using the Pearson chi square test for discrete data and the Kruskal-Wallis test for continuous data.
Results
The at-risk population in the study included 855 admissions, half of whom were men. Half of the 855 patients had been compulsorily detained under mental health legislation. Over the seven-month period, 174 patients were involved in 752 incidents meeting the criteria for levels 1 to 4 of Morrison's hierarchy. Of these patients, 20 met the definition for recidivism. The recidivist patients represented 2.3 percent of the 855 admissions and 11.5 percent of all those involved in violent incidents. As
Table 1 shows, the 20 recidivist patients were responsible for 520, or 69 percent, of the 752 serious violent and aggressive incidents identified.
Comparison of patients
Patients' sex was not associated with recidivism. Compared with nonrecidivist patients involved in violent incidents, recidivist patients were significantly more likely to be widowed χ2=72.13, df=3, p<.001) and to suffer organic brain syndromes or personality disorders (χ2=36.87, df=4, p<.001). Compared with nonrecidivist men, recidivist men were significantly more likely to have an organic brain disorder (χ2=23.46, df=4, p= .001). Compared with nonrecidivist women, recidivist women were significantly more likely to have a personality disorder (χ2=70.61, df=3, p<.001).
Recidivist patients were significantly older than nonrecidivists (mean± SD age of 60.6±22 versus 50.6±22 years; t=5.84, df=750, p<.001). This finding was true for both recidivist men (61.1±22 versus 49.8±22 years; t=5.43, df=536, p<.001) and recidivist women (59.4±20 versus 52.7±20 years; t=2.27, df=212, p=.02).
Recidivism was no more common among repeat-admission patients than among first-admission patients. Recidivist patients were significantly more likely to be detained under mental health legislation (χ2=81.20, df=4, p<.001). All of the recidivist patients had a history of aggression, compared with 26 percent of the nonrecidivist patients (χ2=112.37, df=1, p<.001). Recidivist patients were significantly more likely to be highly sedated before the incident than nonrecidivist patients (χ2=77.58, df=2, p<.001).
Comparison of incidents
The rate of level 1 incidents was significantly higher among nonrecidivist patients, and the rate of level 2 incidents was significantly higher among recidivist patients (χ2=9.37, df=3, p=.02). Nonrecidivist patients were significantly more likely to assault psychologists or social workers (χ2= 5.62, df=1, p=.02), medical staff (χ2= 16.84, df=1, p<.001), and family members (χ2=7.92, df=1, p<.01) and to commit self-harm (χ2=16.27, df=1, p<.001). Nonrecidivist patients were also more likely to use a weapon (usually an object found on the unit) (χ2= 7.06, df=1, p<.01).
Warning signs
Staff members retrospectively identified significantly more warning signs for recidivist patients then nonrecidivist patients (χ2=18.83, df=1, p< .001), particularly agitation (χ2=17.56, df=1, p<.001). However, nonrecidivist patients were more likely than recidivists to make a verbal threat before a violent or aggressive incident (χ2=6.16, df=1, p=.01).
Response to incidents
Incidents by nonrecidivist patients were significantly more likely to be responded to by psychologists or social workers (χ2=9.77, df=1, p<.01), medical staff (χ2=20.07, df=1, p<.001), and psychiatric attendants (χ2=25.02, df=1, p<.001). No differences were found between groups in rates of response by nursing staff, security staff, or police.
The types of staff called in to respond to incidents were compared. After incidents by nonrecidivist patients, two types of staff were significantly more likely to be called in—psychiatric attendants (χ2=38.1, df=1, p<.001) and security staff (χ2=6.38, df=1, p=.01). No differences were found in the rates at which nursing staff, medical staff, or police were called.
According to hospital rules, occupational health and safety officers should be notified after every violent incident. These officers were notified significantly less often after incidents by recidivist patients (χ2=9.34, df=1, p<.01), and the required incident forms were significantly less likely to be completed (χ2=8.59, df=1, p<.01). Victims of recidivist patients were significantly less likely to receive debriefing (χ2=24.36, df=1, p<.001) or to report the incident to police (χ2=7.33, df=1, p<.01).
Outcomes for patients responsible for incidents were examined. Compared with recidivist patients, nonrecidivists were significantly more likely to be secluded after an incident (χ2=9.60, df=1, p<.01), to receive extra medication (χ2=24.66, df=1, p< .001), to be transferred to another hospital (χ2=5.62, df=1, p=.02), and to receive extra supervision (χ2=9.78, df=1, p<.01).
Discussion
Even though this study focused on serious violence and aggression and used a much higher cutoff point to define a patient's violent recidivism (20 incidents of aggression or violence) than in previous research, several previously reported characteristics of recidivist patients were confirmed. Recidivist patients represented 2 percent of the total at-risk population, but were involved in 69 percent of the violent incidents. Nonrecidivist patients engaged in more serious violence and aggression, but the recidivist patients were involved in a large number of incidents that were by no means trivial. The impact of such a small group has been noted in other studies (
2,
4).
As found in other studies (
10,
12), the recidivist patients formed two groups—men with an organic brain syndrome and women with a nonpsychotic psychiatric disorder, such as a personality disorder. In the study reported here, recidivists were older than nonrecidivists due to the higher mean age of men in the study and the fact that there were more men recidivists than women recidivists. Other studies have also found a higher mean age for recidivist patients (
5). As found in previous research (
2,
8), all recidivist patients in this study had a history of violence or aggression.
The new findings in this study were in relation to staff members' responses to the violent incidents. Despite the frequency and serious nature of the incidents examined, several significant differences in response to incidents by recidivists and nonrecidivists were identified. When a recidivist patient was violent, the response was significantly less likely to include the institutional mechanisms for dealing with violence, such as contact of occupational health and safety officers, completion of injury notification forms, and notification of police. The relative lack of response suggests that staff were not surprised by violence perpetrated by recidivist patients and may have been demoralized by the repetitive nature of such violence. This finding further suggests that staff may have become accustomed to the behavior (
12), which may explain the underreporting of violent incidents evident in this and other studies (
19,
20).
Even when victims needed medical care after an incident, the victims of recidivists were significantly less likely to be debriefed than the victims of nonrecidivists. Incidents by recidivist patients were significantly less likely to result in more staff being called in, such as security or psychiatric attendants. Violence occurred among recidivist patients despite the fact that they gave more warning signs and caused more injuries. (It may be that the warning signs were noticed only retrospectively by staff members.) These differences are all the more disturbing because other studies have also shown that staff underreport violence and aggression.
There are several possible explanations for the difference between staff members' responses to incidents by recidivist and nonrecidivist patients. Recidivist patients were significantly less likely to target physicians, and physicians were less likely to respond to incidents by recidivists. Perhaps the repeat incidents were seen as less significant because of the targets and were therefore not responded to with the usual vigor. In addition, the repetitive nature of such incidents may have reduced staff morale, leading staff members to regard violent incidents as part of the regular work environment rather than as unusual or undesirable events in the workplace. The differences in response may be due to staff members' perceived level of personal threat. Perhaps the repetitively violent patient was less personally threatening than the patient who unexpectedly became violent. The notion of perceived personal threat is an area for further study.
The small cohort of recidivist patients identified raises the issue of selective care for the recidivist group within a secure unit established for each geographic region. This group would comprise a disparate patient population, with a mix of younger patients with functional psychosis and older patients with dementia. However, pooling recidivist patients would substantially reduce the number of serious incidents of violence and aggression in mainstream psychiatric units. Such a plan would help caregivers and others conceptualize these patients as having a dual diagnosis—a psychiatric disorder and aggressive behavior—which would help improve patient management.