Caregivers' experiences with their child's ADHD
Six themes underlying caregivers' experiences with their child's ADHD emerged from the data. They included caregiver strain, attribution of meaning, perception of responsibility, problem-solving approach, ADHD treatment beliefs, and response to societal influences. Multiple themes were endorsed in unique ways by each caregiver, but some themes were more predominant than others. The themes represent the breadth of experiences reported by the caregivers and could function as either catalysts or impediments to care seeking.
Caregiver strain was an expression of the distress resulting from the child's behaviors. One caregiver, noting the strain from constant calls from the school, said, “We go through this struggle every day and get these notes every day and these phone calls every day.” Others were not distressed, saying, “If you didn't come from a background with a large family you would be really stressed out .… I'm used to the boys fighting.” Changes in life circumstances, such as having additional children, affected caregivers' tolerance for their child's behaviors and symptoms.
Attribution of meaning referred to how caregivers explained the symptoms, reflecting a deeper insight into caregivers' initial receptivity to getting care for their child. Some explained the child's behavior as an innate characteristic by saying, for example, “Ms. T. recommended [clinic name] to see if he had attention deficit … but I'd always just thought that that was [child's name]!” or “I was just assuming that he was just … bad.” Some caregivers accepted the diagnosis, whereas others offered alternative explanations for behaviors by saying, for example, “I really think she just wants my attention because she is the only girl.”
Perception of responsibility reflected caregivers' view of what needed to be done to help their child. One caregiver stated, “I'm going to make sure she gets the best help she might need.” Others felt their responsibility was to protect the child from being medicated (“He can't speak because he's a child, so someone had to speak for him”). Some placed responsibility with “experts” such as school officials or physicians (“I don't know because I'm not an ADHD expert. … They should get a tutor for him”).
Problem-solving approach reflected how caregivers organized themselves to get help for their child. Some observed the problem, identified a potential solution, and sought help in a timely fashion. Others were problem avoidant, saying, for example, “I kind of ignore it to be honest with you,” or “he's the age where it's harder for me to contain him like my younger children … so I send him away to get a break.”
ADHD treatment beliefs were shaped by past experiences or prior knowledge of medication appropriateness, efficacy, and side effects. These beliefs either encouraged caregivers to seek treatment or discouraged them from seeking treatment. For example, one caregiver stated, “I know a few people whose kids are on [medication] that [are] real sullen and withdrawn, and I didn't want that to be my child.” One caregiver's past experience with her own use of medication (“Before I took medication I didn't believe in ‘head medicine‘ ”) influenced her decision to use medication for her child.
Response to societal influences was also prominent. Some caregivers relied on teachers to “basically just tell [them] what was going on.” Others were confused by conflicting influences. Even as clinicians suggested medication treatment for the child, one said, “Her godmother [told me], ‘It's nothing wrong with her. … You know doctors always say something is wrong with a child and … put [them] on medicine.' ”
Patterns of caregiver theme endorsement
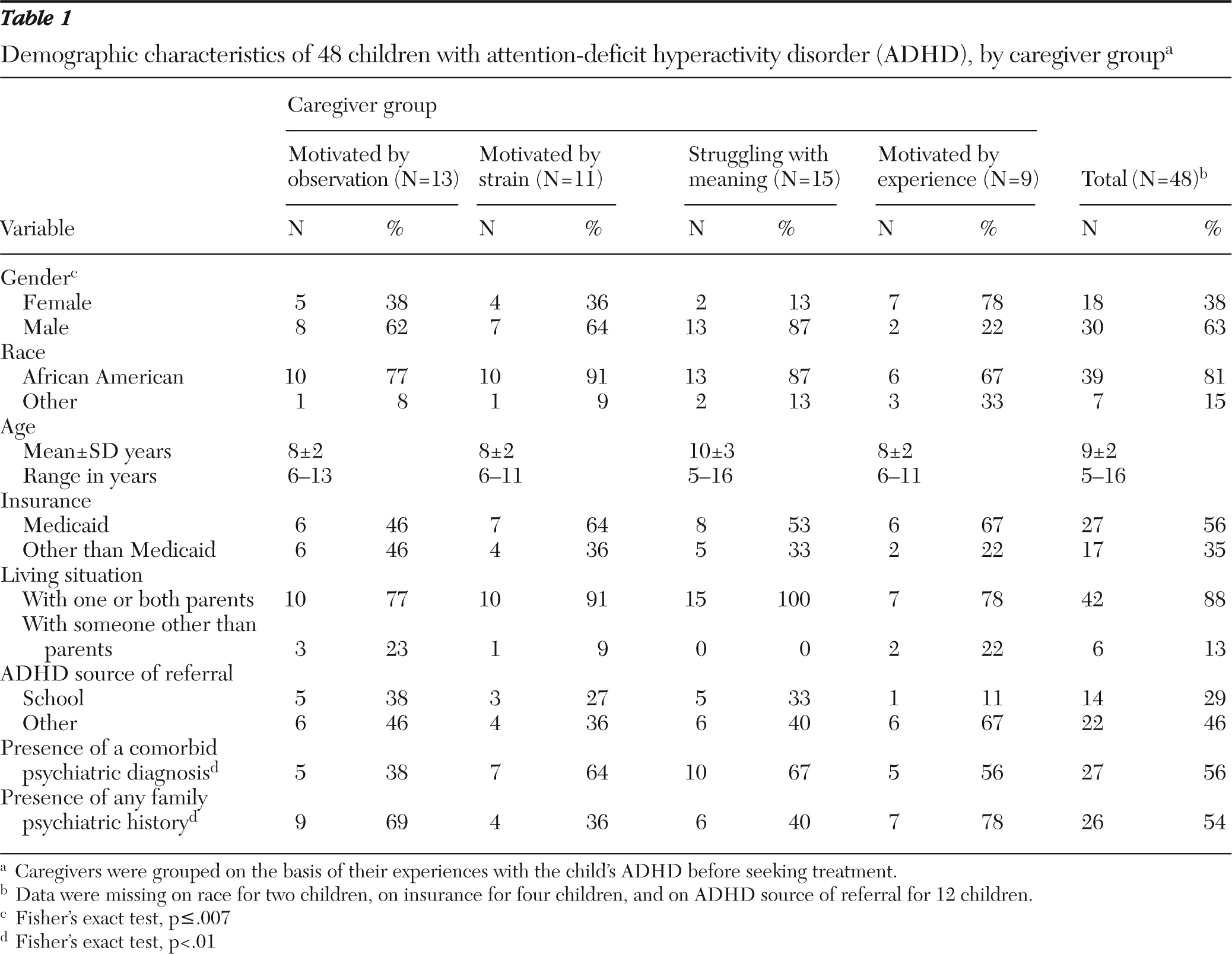
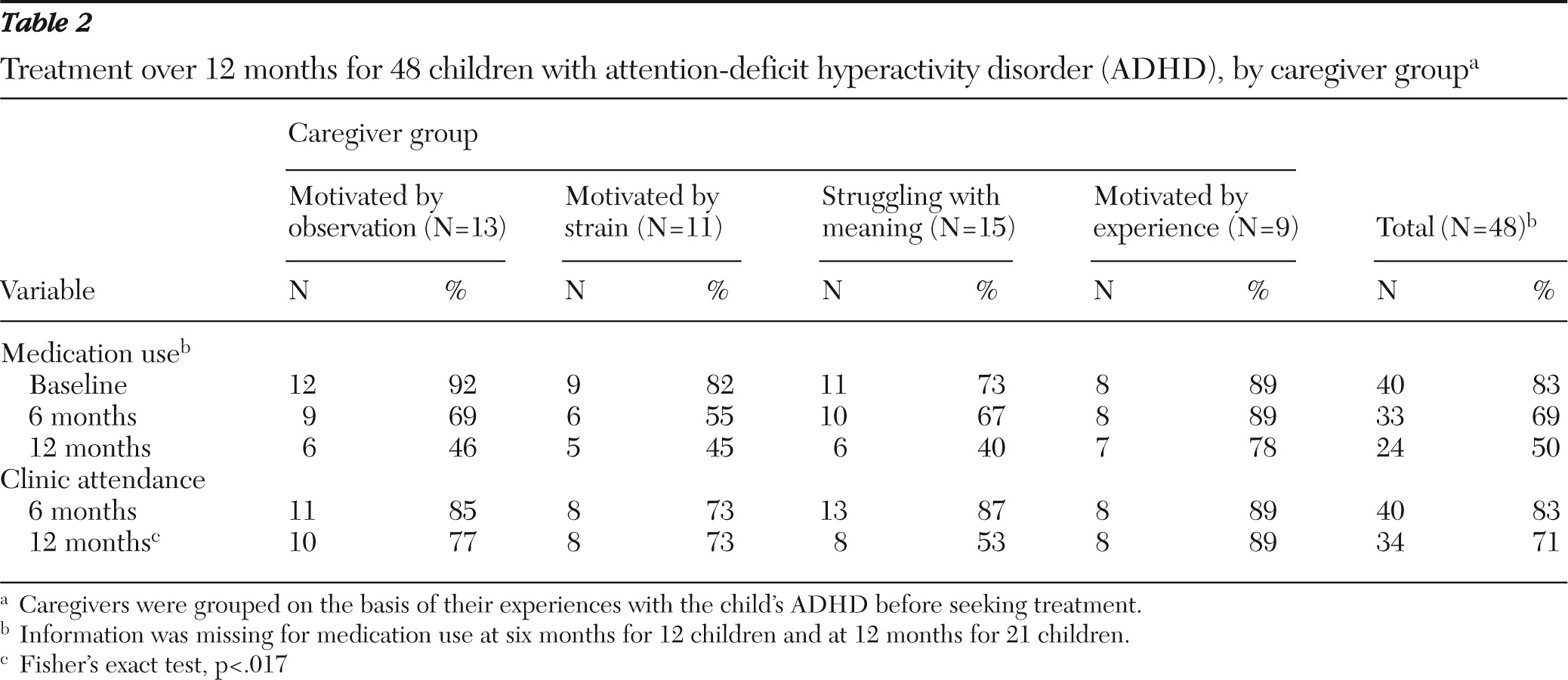
Despite the caregivers' unique situations, the themes endorsed by individuals were classified into four distinct patterns that reflected individuals' experiences leading up to their decision to seek care. They were motivated by observation (N=13, 27%), motivated by strain (N=11, 23%), motivated by experience (N=9, 19%), and struggling with meaning (N=15; 31%).
The group described as motivated by observation clearly perceived their child's behavior as a problem requiring professional attention. The distinguishing characteristics of this group were their systematic problem-solving approaches, their strong sense of responsibility, and their relatively low strain. These caregivers took primary responsibility for the child's success and partnered with professionals to obtain the care the child needed.
The group described as motivated by strain was characterized by disruption, exhaustion, uncertainty, and frustration attributed to their child's behavior. They had a strong sense of responsibility for the child but were uncertain of how to get help and often received mixed advice from others. This situation was a major source of stress. When the diagnosis of ADHD was made, it was generally accepted and received with relief.
The group labeled “struggling with meaning” reflected caregivers who offered alternative explanations for the behaviors that were diagnosed as characteristic of ADHD. Although some had agreed to treatment, their alternative explanation for the child's behavior and adversarial interactions with schools and clinicians were prominent. In contrast to those motivated by strain, these families were strained by the pressure from teachers and doctors to use ADHD medication.
The group considered motivated by experience were those who had greater knowledge of ADHD and were more comfortable with medication and management of their child's symptoms. These families' knowledge allowed them to identify the behavior problems as secondary to the ADHD. Consequently they did not reach a point of strain or distress with the ADHD behaviors.