The hippocampus and amygdala are regions known to be severely affected by the characteristic neuropathology of Alzheimer’s disease
(1–
3). Neurofibrillary tangles in these mesial temporal regions occur early in the course of the disease, and neuronal loss in these structures is apparent as the disease progresses
(1). Both neuropathological and neuroimaging studies of adults with Down’s syndrome report volume reduction of the hippocampus and amygdala
(4–
9). Although all individuals with Down’s syndrome who are over the age of 40 exhibit the neuropathology of Alzheimer’s disease (including atrophy of the hippocampus and amygdala)
(4), many do not demonstrate any of the clinical features of dementia until they are much older
(10). Previous neuroimaging studies
(11–
16) suggest that dementia in subjects with Down’s syndrome is associated with greater brain atrophy than would be expected from aging alone. It is not clear, however, whether mesial temporal structures are more severely affected than are other brain regions in demented individuals with Down’s syndrome, as is the case in individuals with Alzheimer’s disease who had previously normal intelligence. The purposes of this study were to examine the relation between age and the volume of mesial temporal structures in nondemented individuals with Down’s syndrome, to determine whether Down’s syndrome subjects with dementia demonstrate more atrophy in these regions than those without dementia, and to assess longitudinal change in these regions in demented and nondemented Down’s syndrome subjects.
METHOD
The subjects for the cross-sectional studies were 15 men and 10 women with Down’s syndrome (mean age=42.7 years, SD=10.2, range=26–59). All were Caucasian. Each of these subjects was individually matched with a healthy, cognitively normal individual on sex, race, and age (within 3 years). The subjects with Down’s syndrome lived in the community, mostly in supported accommodations. Down’s syndrome was diagnosed by physical examination documenting the presence of mental retardation and characteristic phenotypic features. Karyotypes were obtained on four individuals whose physical characteristics were not clearly congruent with the Down’s syndrome phenotype, and in all four cases Down’s syndrome was confirmed. Potential subjects were excluded if they had untreated medical conditions that might affect cognition (e.g., hypothyroidism). Subjects in the comparison group were recruited from the community and hospital staff. They had no history of psychiatric illness, head injury with loss of consciousness, or substance abuse, as assessed by a structured interview. The procedures were fully explained to all subjects and caretakers. Written informed consent was obtained from caretakers and comparison subjects; verbal assent was obtained from the subjects with Down’s syndrome before enrollment in the study.
Dementia Diagnosis
In clinical interviews with a psychiatrist experienced in the diagnosis of dementia in individuals with mental retardation (A.C.W.), caregivers were questioned regarding symptoms of cognitive and behavioral deterioration in the Down’s syndrome subjects. Evidence of decline in abilities was sought in relation to orientation, memory, language, visuospatial abilities, work performance, and activities of daily living. A diagnosis of dementia was made on the basis of a history of gradual onset and progression of deterioration in memory and in one or more other areas of cognition (e.g., language skills, praxis, gnosia, executive function) in the absence of other CNS or systemic conditions that could account for the deterioration. All subjects diagnosed with dementia met these criteria for loss of cognitive skills and had also shown functional deterioration in terms of work performance or performance of activities of daily living. No subject was taking medicines that could have caused the deterioration.
For the purposes of this study, subjects were categorized as demented if they met the diagnostic criteria at the time of the first magnetic resonance imaging (MRI) scan and if this diagnosis was confirmed by evidence of continued deterioration on 1-year follow-up. (Confirmation of continued decline was not obtained for one subject, who died before follow-up.) On the basis of these criteria, eight of the 25 subjects with Down’s syndrome (four men and four women) were diagnosed as demented. On follow-up visits, a standardized caregiver interview for the diagnosis of dementia in individuals with Down’s syndrome, the Dementia Scale for Down Syndrome
(17), was administered for six of the seven remaining demented subjects, and the diagnosis was confirmed. (A caregiver familiar with the subject’s history was not available for one of the subjects.)
The 17 Down’s syndrome subjects who met none of the dementia criteria at the time of their scans were categorized as nondemented. Only one of the nondemented subjects was diagnosed as demented at her 1-year follow-up visit. (Analyses of the nondemented group were performed both including and excluding the data of this subject.) The demented subjects with Down’s syndrome were significantly older (mean age=54.2 years, SD=2.9) than the nondemented subjects (mean age=37.2 years, SD=7.3) (t=6.29, df=23, p<0.001).
Follow-up scans were available for five of the demented Down’s syndrome subjects, 13 of the nondemented subjects, and the one patient whose diagnosis changed from nondemented to demented during the 2-year interscan interval. (This subject was categorized as demented in the longitudinal analyses.) Except for this subject, dementia status for all other subjects remained unchanged at the time of the follow-up scans. The demented and nondemented subjects did not differ significantly with respect to the interval between scans (mean=22.1 months, SD=12.8, for the demented subjects; mean=20.3 months, SD=8.9, for the nondemented subjects; t=0.35, df=17, p=0.73).
MRI Scans
All scans were obtained on a General Electric 1.5-T Signa scanner with the use of a standard protocol identical to that described in previous reports by our group
(18,
19). This protocol includes a 1.5-mm spoiled-gradient/recalled acquisition coronal series (TR=35 msec, TE=5 msec, number of excitations=1, flip angle=45°), which was used for all measurements reported in this study. The subjects with Down’s syndrome were sedated as necessary to minimize movement artifact. All images were transferred via the Internet and archived on CD-ROM disks.
Measurement of the Hippocampus, Amygdala, and Total Brain Volume
Measurements were made on a Gateway 2000 graphics work station with the use of locally developed custom graphics software. The rules for defining boundaries of the amygdala and hippocampus are described on our laboratory’s Internet homepage (http://pni.med.jhu.edu). Briefly, the posterior boundary of the hippocampus was set at the crus of the fornix. Boundaries of the hippocampus were traced manually, with the choroid fissure as the superior boundary, the inferior temporal horn of the lateral ventricle as the lateral boundary, and the white matter of the parahippocampal gyrus as the inferior boundary. The hippocampus forms a natural boundary around the edge of the mesial temporal lobe. Both the alveus and the subiculum were included in hippocampal measurements. When a clear demarcation between the hippocampus and amygdala was not seen on anterior coronal slices, the sagittal view was consulted to determine the border between the hippocampus and amygdala.
The amygdala was measured in axial slices (0.9375 mm thick) reconstructed from the 1.5-mm coronal series. The superior boundary of the amygdala was set at the level of the tubera where the mamillary bodies and optic nerves can be clearly viewed. A straight line was drawn from the most medial white matter protruding into the amygdaloid gray matter to the lateral fissure; gray matter medial to this line was included in the measurement. The medial boundary was set at the uncus, and the posterior boundary was set at the temporal horn of the lateral ventricle in superior slices and at the hippocampus in inferior slices. No gray matter was measured below the level of the hippocampus. After measuring in axial slices, coronal views were consulted; any measurements made in front of the anterior commissure were erased, as well as any measurements made medial to the uncal notch. The area of each structure was calculated in each slice, and areas were summed across slices and multiplied by slice thickness, resulting in approximate volumes (right and left sides combined). Interrater reliability between two raters (E.H.A., Q.L.) for the hippocampus (intraclass correlation=0.92) and amygdala (intraclass correlation=0.79) was established. Measurements were completed by the two raters (each of whom measured one-half of the scans, which were divided randomly); they were blind to group status (Down’s syndrome subject versus comparison subject, demented subject versus nondemented subject), age, and scan order (initial versus follow-up scan).
Measurement of total brain volume was performed to determine the specificity of volume reductions in the hippocampus and amygdala. A semiautomated thresholding procedure was used for segmenting brain tissue from CSF and extracerebral tissue, as described elsewhere
(20). The intraclass correlation for intrarater reliability in obtaining brain volumes with this procedure was 0.99 for 10 brains.
Statistical Analysis
Volumes of the hippocampus and amygdala from the initial scans of the nondemented Down’s syndrome subjects were compared with volumes of the matched comparison subjects by means of paired t tests. Similarly, structure volumes of the demented Down’s syndrome subjects were compared with volumes of their matched comparison subjects by means of paired t tests and with volumes from the nondemented Down’s syndrome subjects by means of nonpaired t tests. (For the analyses involving data from the initial scans, the one patient with the incident case of dementia was categorized as nondemented; however, analyses were repeated without her data.) All comparisons were redone as analyses of covariance (ANCOVA), controlling for brain volume. Pearson correlations were performed to determine the association between structure volumes and age. Partial correlations were used to assess this relationship while controlling for brain volume. Paired t tests and repeated measures analysis of variance were used to determine whether there were significant changes in structure volumes over time. All reported p values are for two-tailed tests.
RESULTS
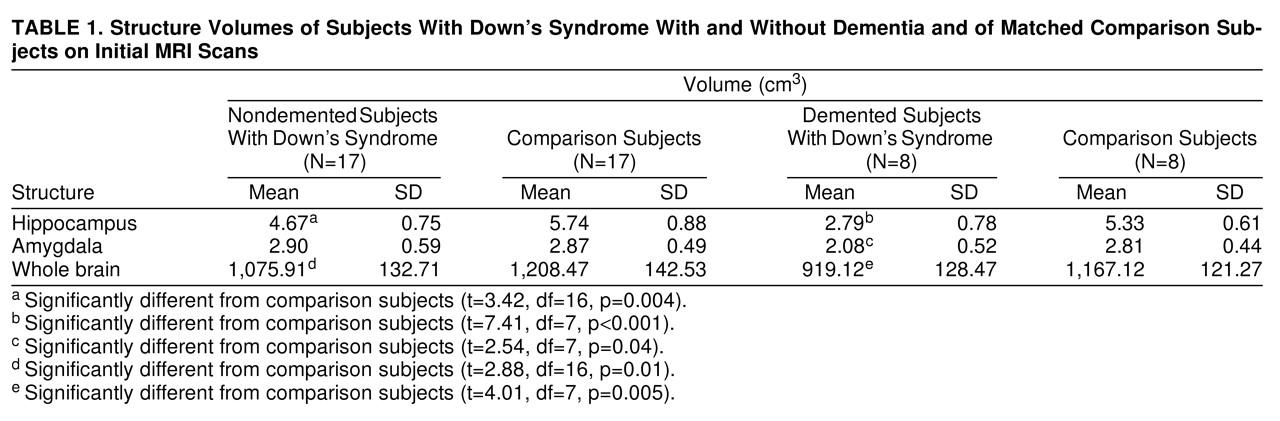
Table 1presents structure volumes of the demented and nondemented Down’s syndrome subjects (from the initial scans) and their individually matched comparison subjects. Hippocampal volumes were significantly smaller in the nondemented Down’s syndrome subjects than in their comparison subjects, but amygdala volumes were not. The mean hippocampal volume for the nondemented Down’s syndrome subjects was 19% smaller than that for the normal subjects. (Results were still significant for the hippocampus when the data of the subject with the one incident case and of her comparison subject were removed from the analysis: t=3.14, df=15, p<0.007.) Group differences in the hippocampus remained significant when we controlled for brain volume through ANCOVA (F=8.81, df=1, 33, p=0.006), even when data of the subject with the incident case and of her comparison subject were removed (F=7.21, df=1, 31, p=0.01). The eight Down’s syndrome subjects with dementia had significantly smaller volumes of the hippocampus and amygdala than their matched comparison subjects. Mean hippocampal volume was 48% smaller, and amygdala volume was 26% smaller. Group differences remained significant when we controlled for brain volume (for the hippocampus, F=18.17, df=1, 15, p=0.001; for the amygdala, F=5.26, df=1, 15, p=0.04).
Amygdala and hippocampus volumes were significantly larger in the 17 nondemented Down’s syndrome subjects than in the eight demented subjects (for the hippocampus, t=5.74, df=23, p<0.001; for the amygdala, t=3.35, df=23, p=0.003). These group differences remained significant after covarying for brain volume (for the hippocampus, F=18.57, df=1, 22, p<0.001; for the amygdala, F=9.89, df=1, 22, p=0.001). The results also remained significant after the incident case was removed from the analyses (for the hippocampus, t=5.62, df=22, p<0.001; for the amygdala, t=3.34, df=22, p=0.003). Age-adjusted difference scores (i.e., the structure volume for each Down’s syndrome subject subtracted from that of his or her matched comparison subject) for the demented Down’s syndrome subjects were significantly greater than for the nondemented subjects (for the hippocampus, t=2.85, df=23, p=0.009; for the amygdala, t=2.54, df=23, p=0.02). The volume of the hippocampus of every demented Down’s syndrome subject was reduced by more than 1 SD (based on mean and standard deviation for the nondemented subjects with Down’s syndrome).
Correlations between age and structure volumes were not significant for the nondemented Down’s syndrome subjects (for the hippocampus, r=0.17, df=13, p=0.50; for the amygdala, r=–0.07, df=13, p=0.80) or for the comparison subjects (for the hippocampus, r=–0.20, df=23, p=0.33; for the amygdala, r=–0.13, df=23, p=0.54). For the eight demented subjects alone, age was significantly correlated with amygdala volume (r=–0.72, df=6, p=0.04) but not with hippocampal volume (r=–0.43, df=6, p=0.27).
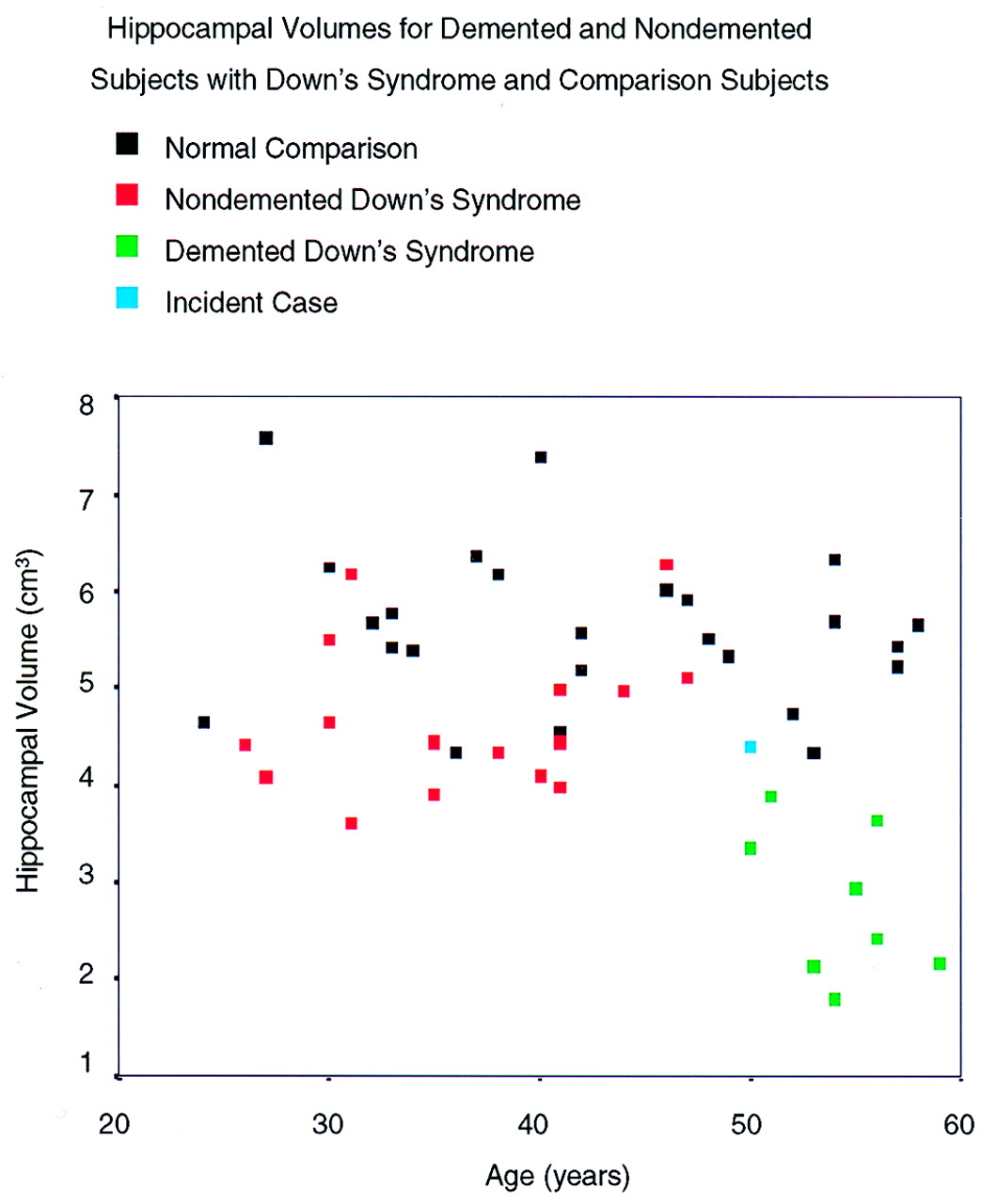
Figure 1 shows the association between age and hippocampal volume for the comparison subjects and the Down’s syndrome subjects with and without dementia.
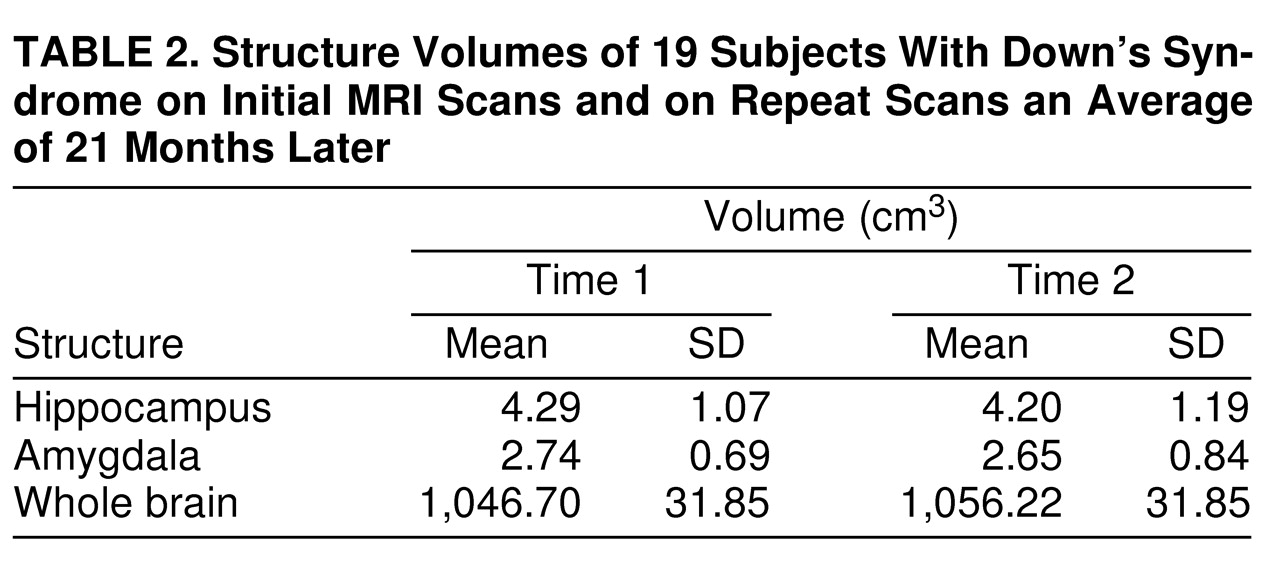
Longitudinal measures of hippocampus, amygdala, and brain volumes were available for 19 Down’s syndrome subjects (12 men and seven women; mean age=41.9 years, SD=9.2) who had follow-up scans 9–41 months after their initial MRI scans (mean interscan interval=20.9 months, SD=10.0) (
table 2). Paired t tests revealed no significant change over time in the hippocampus, amygdala, or total brain volume. Demented Down’s syndrome subjects showed a decrease of 0.13 cm
3 (SD=0.20) per year in amygdala volume and 0.10 cm
3 (SD=0.33) per year in hippocampal volume. The change per year for nondemented subjects was a decrease of 0.02 cm
3 (SD=0.25) in the amygdala and an increase of 0.01 cm
3 (SD=0.35) in the hippocampus. These differences between the demented (N=6) and nondemented (N=13) Down’s syndrome subjects in the amount of volume change over time were not great enough, however, to be statistically significant when we controlled for the interval between scans (repeated measures ANCOVA: for the hippocampus, F=0.38, df=1, 16, p=0.55; for the amygdala, F=1.49, df=1, 16, p=0.24).
DISCUSSION
In agreement with previous neuropathological
(4) and neuroimaging
(6–
8) studies, we found that hippocampal volumes are disproportionately small in individuals with Down’s syndrome, even before any signs of cognitive impairment. In nondemented individuals with Down’s syndrome, hippocampal volumes did not decrease with age, as indicated by the lack of a significant correlation between age and hippocampal volume. (In fact, the correlation was not even in the expected direction for this group.) Raz et al.
(7) also failed to find a significant correlation between age and hippocampal volume in 13 nondemented Down’s syndrome subjects ranging in age from 22 to 50 years. These findings are consistent with earlier computed tomography (CT) findings that generalized cerebral atrophy in nondemented subjects with Down’s syndrome is not accelerated, at least in individuals under 50 years of age
(13). Our finding is contrary, however, to the results of Kesslak et al.
(8), who found a highly negative (r=–0.67) correlation between age and hippocampal volume in a group of 13 nondemented individuals with Down’s syndrome (age range=23–51 years). However, in the study by Kesslak et al., cognitive decline suggesting dementia was determined by “individual neurologic examinations for pathologic reflexes suggestive of neurodegeneration,” which are signs generally seen only in the latest stages of dementia. Thus, some of the older individuals in their study might have been considered demented according to the criteria used in our study (where the dementia diagnosis was based on a history of decline in cognitive and functional abilities, as reported by caregivers and observed during clinic visits.) In addition, eight of the 13 subjects in the study by Kesslak et al. were less than 30 years of age, whereas only two individuals in our group of 25 subjects were under age 30. It is possible that the volume of the hippocampus decreases significantly before age 30, remains stable, and then declines again in later life as individuals become demented.
Figure 1 suggests that hippocampal volume, while somewhat smaller in subjects with Down’s syndrome than in comparison subjects, remains fairly stable with age in nondemented individuals, at least through the fifth decade. It cannot be determined whether the precipitous drop in hippocampal volume after age 50 is associated with older age or dementia, as all subjects in this study who were over age 50 had diagnoses of dementia.
Amygdala volumes of the demented Down’s syndrome subjects were significantly smaller than those of the matched comparison subjects, even when brain volume was controlled for. Amygdala volumes of the nondemented Down’s syndrome subjects did not differ from those of the comparison subjects. As with the hippocampus, amygdala volumes did not decrease with age among the nondemented Down’s syndrome subjects. These findings suggest that the amygdala is proportionate to total brain volume during development, but that specific atrophy of the amygdala, like that of the hippocampus, is involved in the dementia experienced by elderly persons with Down’s syndrome.
Subjects with Down’s syndrome who were diagnosed as demented had significantly smaller volumes of the hippocampus and amygdala than those who were not demented. This difference was not the result of normal aging, since individual Down’s syndrome subjects with dementia differed more from their matched comparison subjects in hippocampal and amygdala volumes than did the Down’s syndrome subjects without dementia. These findings corroborate those of a qualitative analysis of two MRI scans from demented individuals with Down’s syndrome
(8), where hippocampal atrophy was similar to that observed in the moderate to severe stages of Alzheimer’s disease. Using a CT measure of mesial temporal atrophy, the suprasellar cistern ratio, Pearlson et al.
(11) also found evidence of more atrophy in Down’s syndrome subjects with dementia than in those without.
Longitudinal change over a mean interval of 21 months in volumes of the amygdala and hippocampus was not significant for either the demented or the nondemented group. The small size of the demented group, however, prevents us from concluding that volumes of the amygdala and hippocampus remain constant after the onset of dementia. In 20 nonretarded individuals with histopathologically confirmed Alzheimer’s disease, Jobst et al.
(21) found an average rate of atrophy of the medial temporal lobe of 15.1% per year, compared with 1.5% in 47 healthy elderly individuals (although the subjects with Alzheimer’s disease were, on average, 8 years older than the comparison subjects).
The strengths of this study include its relatively large, well-characterized group of adults with Down’s syndrome who were individually matched to cognitively normal comparison subjects. The dementia status of both the demented and the nondemented Down’s syndrome subjects was confirmed by evidence of continued cognitive decline or stability on follow-up examination 1 year after the MRI scans were obtained. Study weaknesses include the absence of nondemented Down’s syndrome subjects over the age of 50, which prevented us from testing the hypothesis that volume reductions in mesial temporal structures are specifically associated with dementia and not simply a reflection of aging in this population. A larger study group or one containing more incident cases, as well as greater interscan intervals, might have yielded evidence of significant longitudinal change with the onset of dementia.
In summary, we conclude that hippocampal volume, while disproportionately small for brain size in individuals with Down’s syndrome, remains fairly constant through the fifth decade of life. We observed volume reduction in the hippocampus and amygdala, as well as clinical signs of dementia, in all of our subjects over the age of 50.