Data for this analysis were drawn from the National Comorbidity Survey, which consisted of a structured psychiatric interview of a representative national sample of 8,098 residents in the United States. Persons aged 15–54 years were selected from the noninstitutionalized civilian population in the 48 coterminous United States and a representative supplemental sample of students living in campus group housing
(5) Of all individuals contacted for participation in the survey, 82% completed the survey assessment. The survey used a two-stage design. In part II, the use of mental health services by a subsample of 5,877 respondents was assessed. These 5,877 respondents included those who had any lifetime diagnosis according to the part I assessment, all persons in the age range of 15–24 years, and a random subsample of the remaining part I respondents. Written informed consent was obtained from each participant after the survey had been fully explained. A detailed description of the National Comorbidity Survey design has been presented elsewhere
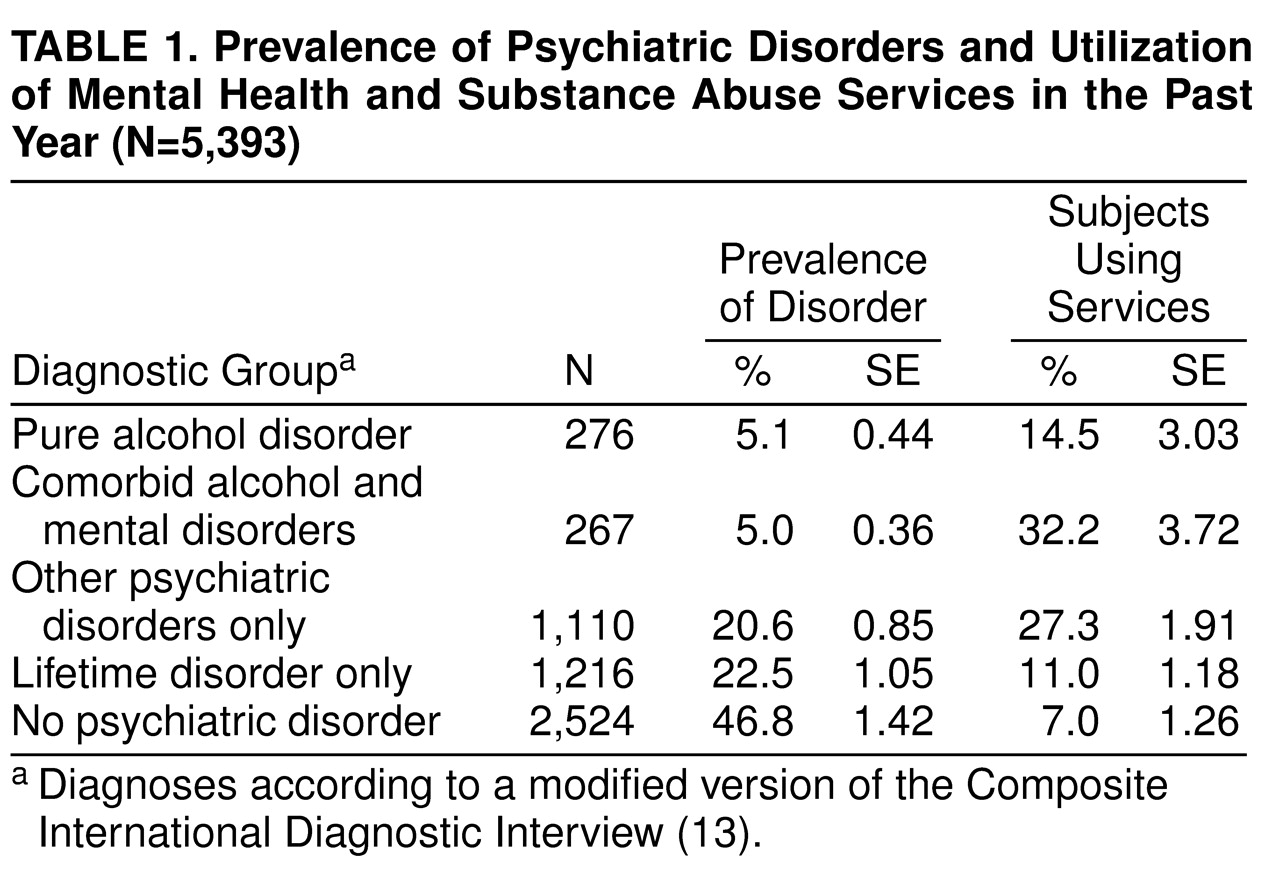
(5). For the present investigation, the statistical analysis was based on data from part II adult respondents aged 18–54 years (N=5,393); data from youths aged 15–17 years were excluded. This allowed us to examine mental health service utilization by the adult respondents in the National Comorbidity Survey.
Measures
The National Comorbidity Survey used a modified version of the Composite International Diagnostic Interview
(13) to generate psychiatric diagnoses based on DSM-III-R. The modified version was developed at the University of Michigan for the survey
(14). The diagnostic criteria for alcohol abuse/dependence and other psychiatric disorders were consistent with those in a previous report from the National Comorbidity Survey
(5).
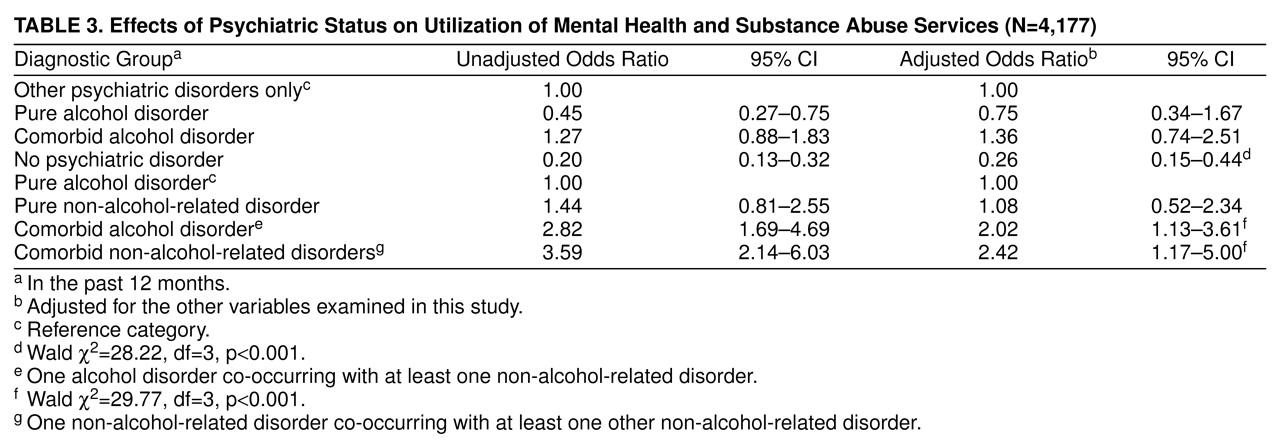
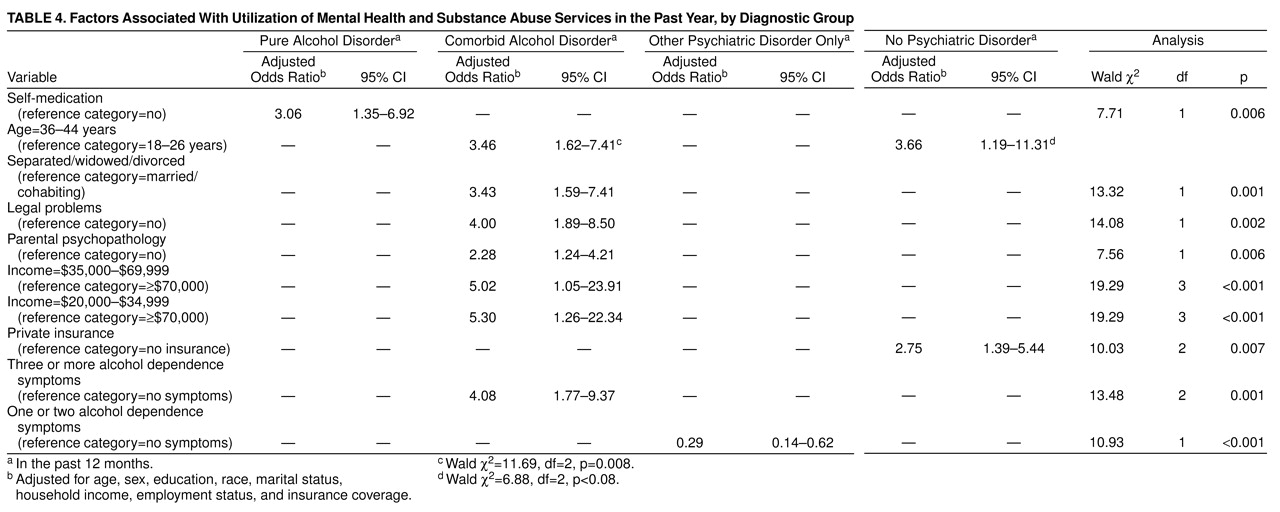
Utilization of mental health and substance abuse services was defined as any visit to mental health care providers, specialty substance abuse care providers, general medical care providers, human service agencies, or self-help groups for mental health problems, alcohol use, and/or drug use in the past year as reported by the respondents.
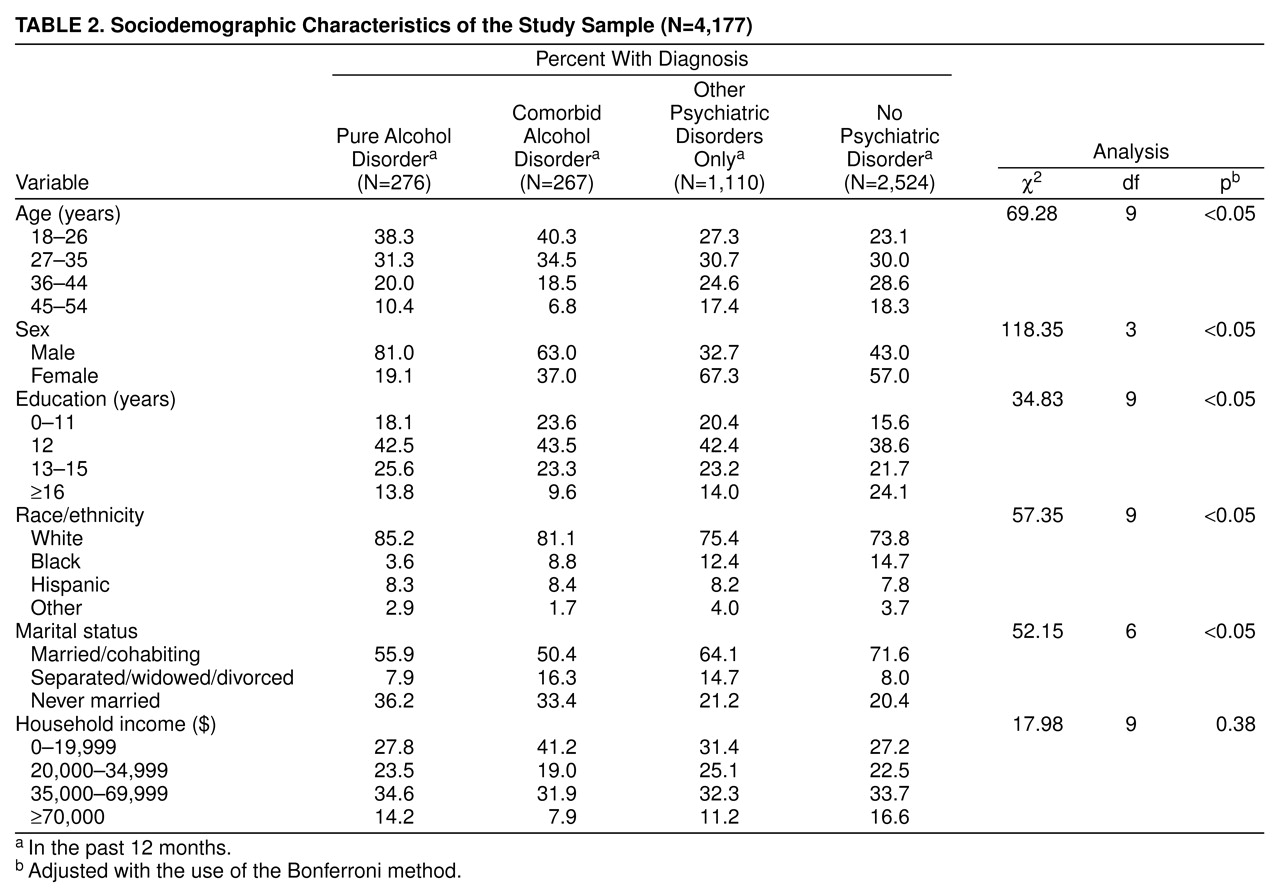
Respondents were categorized into five groups according to the nature of their psychiatric disorders. 1) The group with pure alcohol disorder (N=276) included adults who had met the criteria for alcohol abuse or dependence, but not other psychiatric disorders, in the past year. 2) The group with comorbid alcohol and mental disorders (N=267) included adults who had met the criteria for both alcohol abuse/dependence and at least one other psychiatric disorder in the past year. These disorders included major depression, dysthymia, mania, bipolar disorder, generalized anxiety disorder, panic disorder, simple phobia, social phobia, agoraphobia, posttraumatic stress disorder, drug abuse/dependence, and nonaffective psychosis. 3) Respondents who met the criteria for at least one of the other psychiatric diagnoses and who did not meet criteria for alcohol abuse or dependence in the past year constituted the group with other psychiatric disorders (N=1,110). 4) Respondents who met the criteria for any psychiatric disorder in their lifetime but not in the past year were included in the lifetime group (N=1,216). 5) The group with no psychiatric disorder (N=2,524) included adults who had never met the criteria for any DSM-III-R diagnosis in their lifetime.
Alcohol-related symptoms
Alcohol-related symptoms were assessed and defined by items from the Alcohol section of the modified Composite International Diagnostic Interview, which elicited information on the respondent’s use of alcohol, with a focus on the amount, frequency, and consequences of alcohol use. These symptoms included the amount of alcohol drinking, alcohol-related social or occupational impairments, alcohol-related health or psychological problems, and the number of alcohol dependence symptoms. Alcohol drinking was assessed by asking respondents about the number of alcoholic drinks consumed in a single day in the past year. Alcohol-related social or occupational impairments were assessed by five items. Alcohol-related health or psychological problems were assessed by asking the respondent whether alcohol use caused health, emotional, or psychological problems (two items). The number of alcohol dependence symptoms was measured by 10 items.
Sociodemographic variables
These variables included age (in years), sex, education (in years), race/ethnicity, marital status, household income (in dollars), employment status (currently working for pay versus not working for pay), and insurance coverage (none, Medicaid, private insurance).
Social and psychological factors
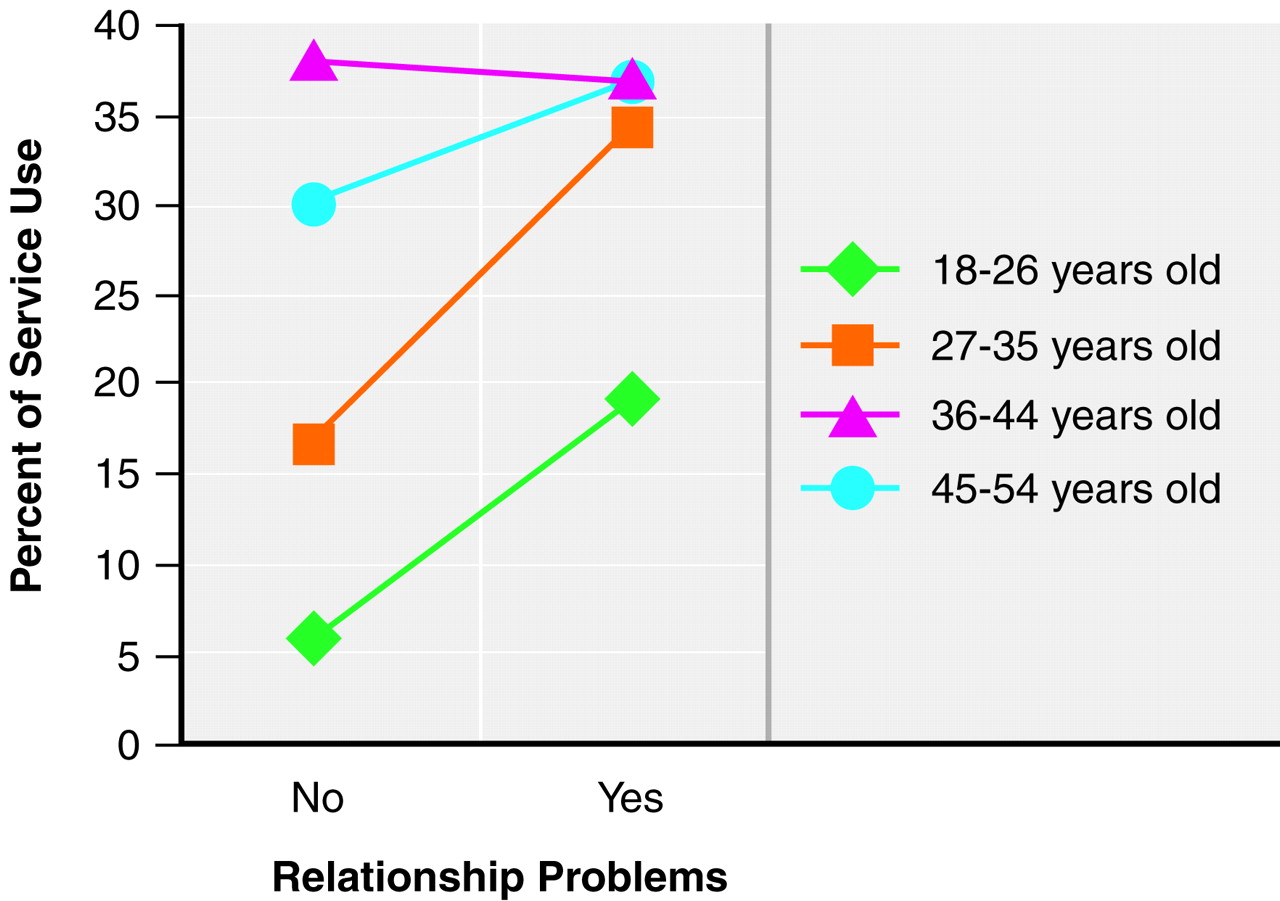
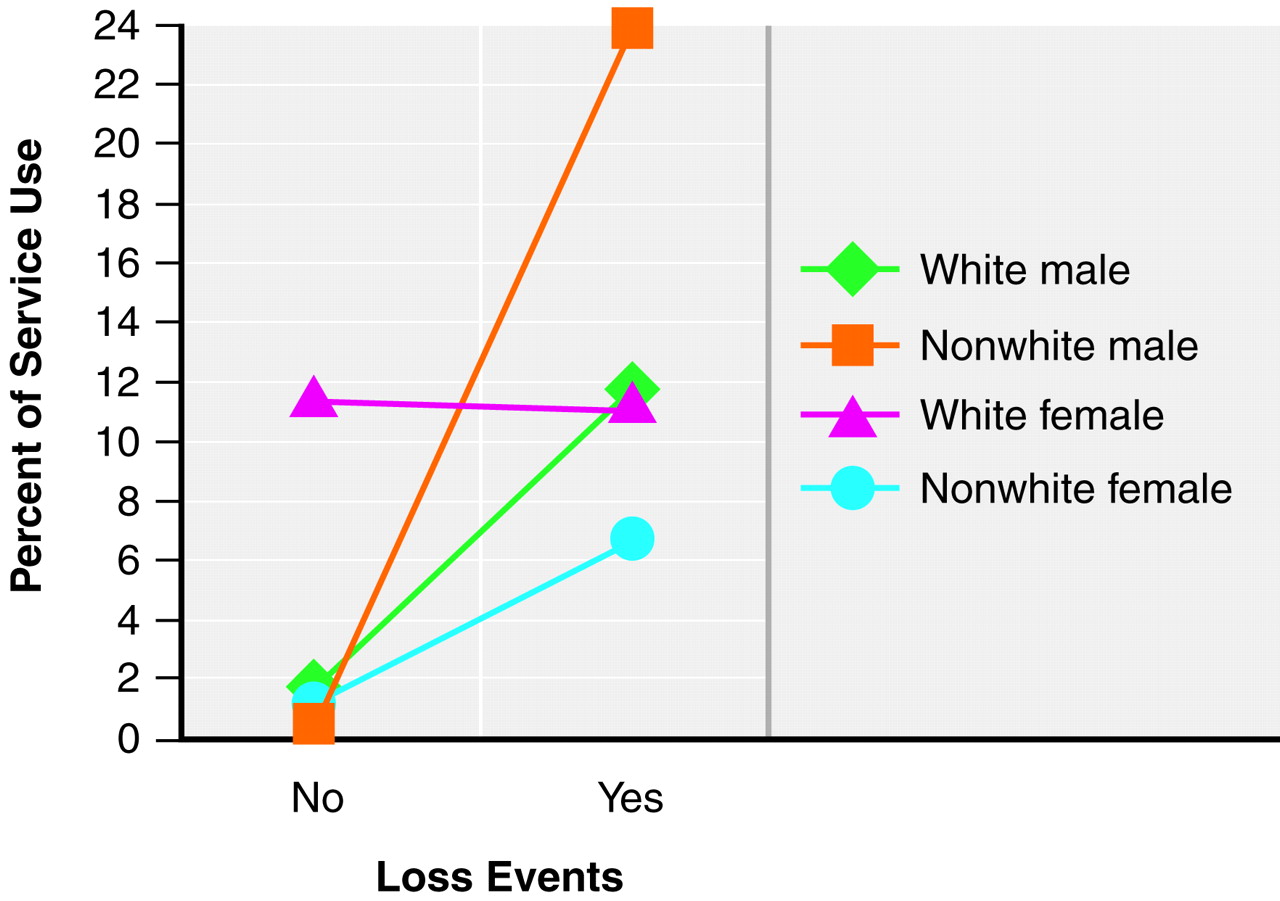
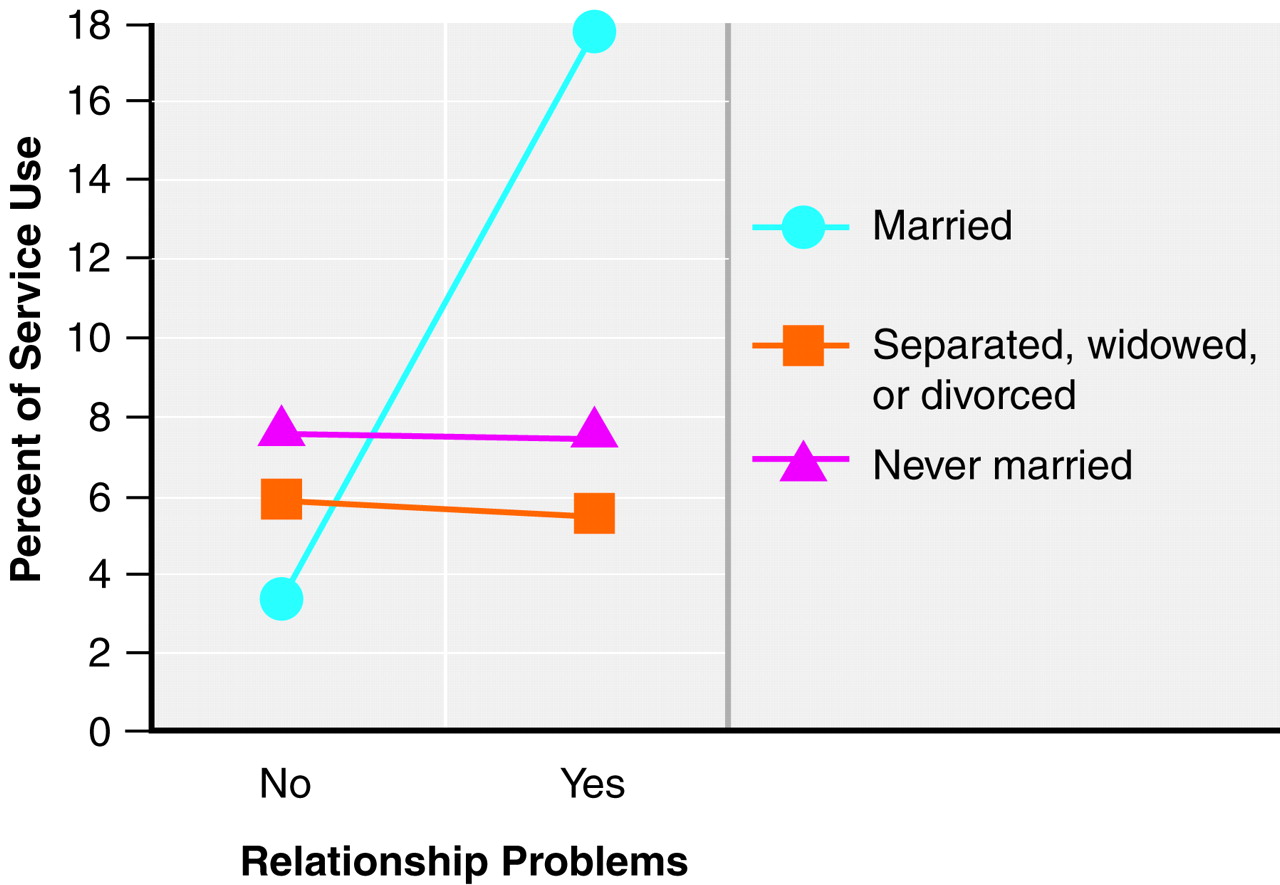
Social support, conflicted support networks, self-medication, recent stressful life events, and parental history of psychopathology were included. Social support was assessed by asking the respondents about positive characteristics of their social support network (spouse, relatives, or friends) (20 items). Conflicted support networks were measured by asking respondents about negative aspects of the support network (18 items). Self-medication was defined as ever having drunk more than usual or having used drugs not prescribed by a physician (or in greater amounts than prescribed by a physician) to help reduce psychiatric symptoms (e.g., fears, anxiety, sadness, manic feeling, or panic attacks). Recent stressful life events included legal problems, loss events, and relationship problems that had occurred in the year before assessment. Legal problems were defined as having been sued by someone, ever having sued someone, or ever having had trouble with the law enforcement system. Loss events were defined as recently experiencing the death of a close friend or a relative. Relationship problems were defined as having a broken close relationship, a long separation from a loved one, or tension or conflicts with friends or family members. Information on whether the respondent’s natural father or mother had ever been hospitalized or treated for depression, anxiety, or alcohol/drug problems was also collected.