As evidenced by several trials, there are highly effective psychological treatments for panic disorder with or without agoraphobia
(1) . However, only about 25% of the people suffering from panic disorder seek some kind of treatment
(2) . The reasons for not seeking treatment may be a shortage of skilled therapists, long waiting lists, or the high cost
(3) . People in rural areas are particularly disadvantaged because of the time it takes to travel long distances. Another problem that might arise is that people with agoraphobia may not seek treatment because of the fear of leaving their homes or traveling certain distances. Therefore, a major challenge is to increase the accessibility and affordability of evidence-based psychological treatments with the help of long-distance techniques, such as the Internet and the telephone.
Materials
All participants had access to a computer with an Internet connection and could print out training instructions, thought records, and other exercise materials. They were informed about the general risk of unauthorized people intercepting e-mail messages and were instructed to use a free online e-mail service that automatically encrypts messages (2,048 bits).
Outcome Measures
A set of valid and commonly used questionnaires were administered. Cognitions were assessed with the Agoraphobic Cognitions Questionnaire
(17) . The Body Sensations Questionnaire
(17) was used to measure physiological sensations experienced by patients with anxiety disorders. The degree of agoraphobia was measured with the Mobility Inventory
(18) . The inventory has two parts; the patient rates the degree of avoidance when alone and when accompanied by a trusted person. Generalized anxiety was assessed with the Beck Anxiety Inventory
(19) . Level of depression was measured with the Beck Depression Inventory
(20) . The patient’s quality of life was measured with the Quality of Life Inventory
(21) . To investigate if credibility could predict treatment outcome, a scale adapted from Borkovec and Nau
(22) was used. All outcome measures had adequate psychometric properties and were administered via the Internet
(23) .
Procedure
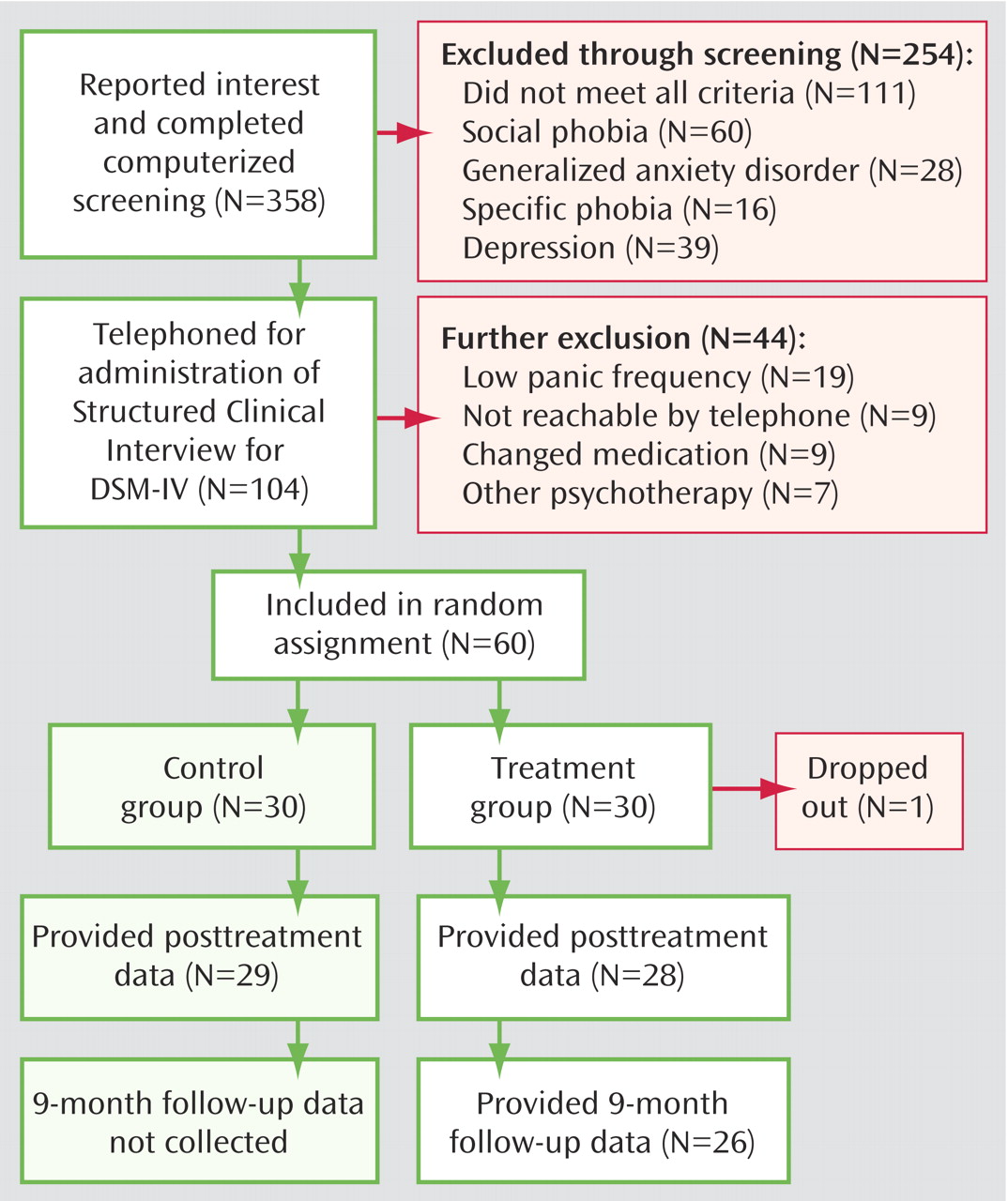
An overview of the procedure is given in
Figure 1 . There were no significant differences in demographic characteristics between the groups according to chi-square analysis. Hence, demographic data are presented for the entire study group (N=60). Sixty percent of the participants were women, with a mean age of 36.7 years (SD=10.0). The highest educational level ranged from 9 years of compulsory school (5%) to completion of college or a university (33%). Uncompleted secondary school was the educational level of 5% of the participants, 37% had completed secondary school, 2% had uncompleted vocational school, 3% had completed vocational school, and 15% had uncompleted college or university (15%). Forty-five percent of the participants were married with children, and 22% were married without children (22%). Single people with and without children were 15% and 18% of the participants, respectively. Most of the subjects were working or studying (75%), whereas a few were registered as not well full-time (18%) or part-time (7%). Fifty-four percent were taking medication.
The participants were divided into two groups, treatment or a waiting list, by a true random-number service. One participant dropped out during the study; shortage of time was said to be the main reason. However, in accordance with the intention-to-treat paradigm (e.g., reference 24), posttreatment data were also collected from the participant who dropped out. Two participants in the treatment condition and one on the waiting list did not return their posttreatment questionnaires. Therefore, their pretreatment scores were carried forward to the posttreatment assessment point. Hence, all 60 participants who were randomly assigned to one of the two conditions were included in the statistical analysis.
Nine-month follow-up data were collected from the treatment group only because the waiting list group was offered treatment in a different format immediately after the treatment period.
Treatment
The treatment was manualized and divided into 10 modules: modules 1–2, psychoeducation and socialization; module 3, breathing retraining and hyperventilation test; modules 4–5, cognitive restructuring; modules 6–7, interoceptive exposure; modules 8–9, exposure in vivo; and finally, module 10, relapse prevention and assertiveness training. Each module consisted of approximately 25 pages of written text.
The modules were converted into interactive web pages and were accessible via the World Wide Web. All participants accessed the program at home but some also from their offices. Each module included information and exercises and ended with three to eight essay questions. The participants were asked to explain (in their own words) the most important sections of the module they had just completed, provide thought records, and describe their experience with and results of their exposure exercises. The questions were included to promote learning and to enable the research supervisors to assess whether the participants had understood the material and completed their homework. Also included in each module was an interactive multiple-choice quiz that the participants had to provide all the right answers for in order to proceed. Otherwise, they received immediate automatic feedback and the correct answer with an extensive explanation. For each module, the participants were required to post at least one message for an online discussion group about a predetermined topic. Because fellow participants were able to read and comment on each other’s messages, a warm and supportive atmosphere developed between the participants.
Feedback on homework was usually given within 24 hours via e-mail. An assessment was made by a therapist of whether the participant was ready to continue or not. If he or she was ready to continue, a password to the next module was sent. If not, the participant received instructions as to what to complete before proceeding to the next module. The participants were encouraged to come up with questions, and they were free to send an unlimited number of e-mail messages. The total number of reciprocal contacts (received and sent) ranged from seven to 29 (mean=13.5, SD=4.4). Because the e-mail responses to the participants often were very similar, much text could be recycled while care was being taken not to miss the specifics of each individual client. The mean time spent on each participant per week was approximately 12 minutes, including administration and responding to e-mail.
Weekly telephone calls were made by the therapists to each participant. The purpose was to provide positive feedback and answer questions about the modules. Telephone conversations were timed and lasted an average of 11.8 minutes per week (range=9.6–15.6).
The therapists in the study were two students in their final year of studying to become psychologists (M.Sc.) and one licensed psychologist (M.Sc.) who were all given regular supervision from a clinician experienced in cognitive behavior therapy, specializing in panic disorder.
After the 10-week treatment program, posttreatment questionnaires were sent via the Internet to both the treatment and control groups. The treatment group was also asked to evaluate the program.
Statistical Analysis
Significance testing of group differences in demographic data, pretreatment measures, and clinical significance was conducted with chi-square and t tests. The participants’ pretreatment and posttreatment measures were analyzed with two-way analysis of variance (ANOVA) with repeated measures. These were followed by t tests with Bonferroni-corrected p values, which were placed at 0.0125. This limit was obtained by dividing the traditional alpha level by the maximum number of individual group comparisons (i.e., four). All analyses were made with the statistical program SPSS, version 12.0.1 (SPSS, Chicago). Effect sizes were calculated both within and between groups, and all calculations were based on the pooled standard deviation, Cohen’s d.
Results
The two groups did not differ significantly on any of the measures at pretreatment (t=0.2 to 1.7, df=58, p=0.86 to 0.09). The results will be presented in the following order: self-report inventories (including effect size), clinical re-interviews, treatment credibility, and an evaluation of the program by the participants.
Self-Report Scales and Effect Sizes
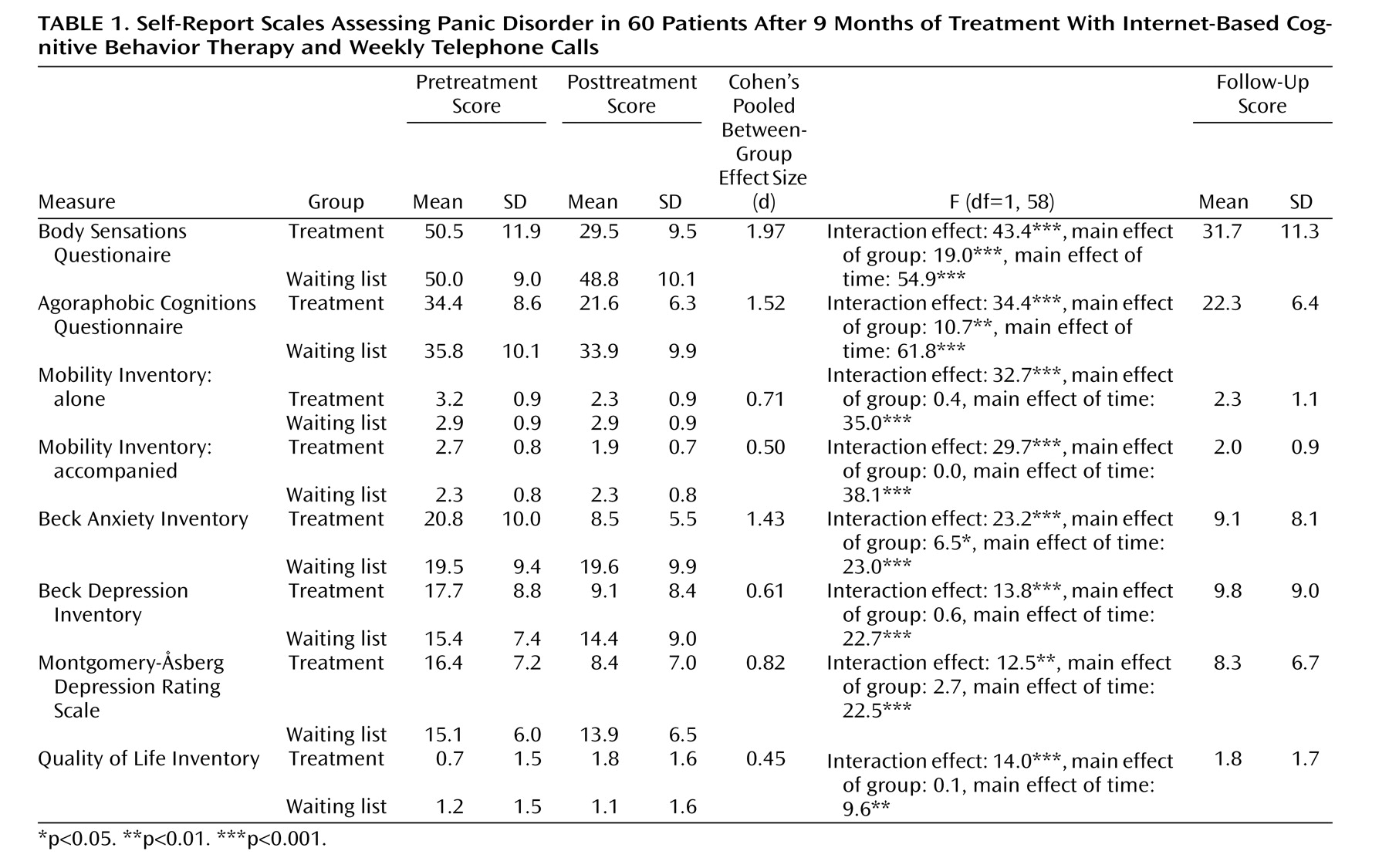
As evident from
Table 1, all ANOVAs revealed significant interaction effects with respect to group and time (all p<0.01). Post hoc t tests with Bonferroni-corrected p values suggested that the treatment group had improved significantly between pretreatment and posttreatment on all measures (t=4.4 to 8.7, df=29, all p<0.0001), whereas the control group had not (t=0.1 to 2.0, df=29, p>0.98 to 0.05). The tests also revealed that a significant posttreatment difference existed between the groups on seven of the eight measures. There were significant effects for the Body Sensations Questionnaire, the Agoraphobic Cognitions Questionnaire, the Mobility Inventory alone, the Mobility Inventory accompanied, the Beck Anxiety Inventory, the Beck Depression Inventory, and the self-report MADRS (t=2.3 to 7.6, df=58, all p<0.0125) but not the Quality of Life Inventory after Bonferroni correction (t=1.7, df=58, p<0.05).
Of the 30 people in the treatment group, 26 returned the 9-month follow-up questionnaires. The treatment effect was stable. Paired t tests showed that there were significant differences between pretreatment and follow-up scores on all measures (t=3.6 to 8.0, df=29, p<0.001) but no robust posttreatment versus follow-up changes (t=0.2 to 1.4, df=29, p=0.98 to 0.18).
The between-group effect size (pooled SD) varied markedly across the different measures. The highest value was found on the Body Sensations Questionnaire (Cohen’s d=1.97), whereas the lowest value was found for the Quality of Life Inventory (d=0.45). The mean between-group effect size across all measures was large (d=1.00). The within-group effect size for the treatment group was d=1.10 at posttreatment and d=0.95 at the follow-up. The corresponding figure for the waiting list was d=0.10 (pretreatment/postreatment).
Compliance
Of 30 participants, 24 (80%) finished all of the modules within the intended 10-week time limit. Hence, the average number of modules completed in this study was nine (mean=8.9, SD=2.6). The figure increased to mean=9.2 if the participant who dropped out in the beginning was excluded and to mean=9.3 if two participants who finished the last module just 2 weeks after the treatment ended were included. Compared to the same Internet treatment but without telephone calls
(8), the average of 8.9 modules in the present study was significantly more than the average of 7.4 modules (unrelated t test=–2.4, df=53, p<0.05) in the previous study. Hence, telephone calls seem to have made a difference regarding compliance when they were defined as the number of treatment modules finished within the time limit.
Clinical Significance
The clinical significance of the treatment was assessed in two ways: one with a statistical method, the other with clinical judgment in a reinterview administered by an independent psychologist who was blind to treatment condition.
The conservative method suggested by Jacobson and Truax (equation “C”; cf. reference
24 ), supplemented with Swedish reliability data
(23), was used to calculate the proportion of significantly clinically improved patients on the main outcome measures.
The treatment group had a significantly larger proportion of clinically improved participants on all of the main outcome measures: the Body Sensations Questionnaire (70% versus 7%; χ 2 =25.5, df=1, p<0.001), the Agoraphobic Cognitions Questionnaire (67% versus 0%; χ 2 =30.0, df=1, p<0.001), the Mobility Inventory: alone (67% versus 7%; χ 2 =23.5, df=1, p<0.001), and the Mobility Inventory: accompanied (73% versus 7%; χ 2 =27.8, df=1, p<0.001). At the 9-month follow-up, the average proportion of clinically improved individuals was 63.5% (the Body Sensations Questionnaire=60%, the Agoraphobic Cognitions Questionnaire=67%, the Mobility Inventory: alone=67%, and the Mobility Inventory: accompanied=60%).
After treatment, a clinical telephone interview, administered by two independent research assistants who were blind to treatment condition, was used to determine if each participant still fulfilled the criteria for panic disorder. One month after treatment, 23 participants (77%) in the treatment group and none on the waiting list (0%) no longer met the criteria for panic disorder (χ 2 =37.3, df=1, p<0.001). Hence, a majority of the treated subjects no longer suffered from panic disorder, whereas all of the untreated subjects did still suffer.
Treatment Credibility
The credibility of the treatment was estimated at mean=36.9 (SD=11.5) on the Borkovec and Nau Scale
(22) . In comparison with a recent study of Internet therapy targeting the same population
(8), the present credibility rating was slightly higher than pure Internet therapy (mean=33.8) but lower than standard therapy (mean=40.6).The credibility score was positively correlated with the change scores on the Body Sensations Questionnaire, the Agoraphobic Cognitions Questionnaire, both Mobility Inventory subscales, the Beck Anxiety Inventory, and the Quality of Life Inventory (all r>0.32, all p<0.05).
Participants’ Evaluation of the Treatment
Most participants were satisfied (21%) or very satisfied (76%) with the treatment they had received. Only 3% were indifferent to, or dissatisfied with, the treatment. However, most participants felt that the pace was a little too fast (46%) or much too fast (29%). Only 21% stated that 10 weeks was sufficient treatment time. On the other hand, 4% reported arguing that 10 weeks was a little too much time.
Discussion
The results suggest that Internet-administered self-help plus minimal therapist contact via e-mail, with the addition of short weekly telephone calls, can be effective in treating panic disorder. The participants improved significantly on the self-report scales used, whereas the subjects on the waiting list did not.
Specifically, bodily sensations (associated with the arousal accompanying anxiety) were reduced, as well as anticipatory and catastrophic thoughts, agoraphobic avoidance, severity of anxiety symptoms, and depression. Finally, overall life satisfaction increased. However, when disregarding the significant interactions and looking at the between-group results immediately following treatment, the quality-of-life measure showed promising results but did not survive Bonferroni correction. Apart from power issues, a reason could be that the treatment period was too short to have an effect on the quality-of-life measure with broad items such as “number of children.” Unfortunately, because people on the waiting list received treatment before the follow-up data were collected, there was no between-group comparison at 9 months.
The proportion of participants finishing the entire treatment package within the 10-week time frame was almost as high as reported for live therapy (80% versus 88%; reference 11). Additionally, when we compared the composite within-group effect size in the present study (d=1.10) with that of an earlier study using the same outcome measures and targeting the same population
(8), the effect size was more similar to that of the live treatment group (d=0.99) than that of Internet-based therapy only (d=0.78). Hence, judging from effect sizes, adding telephone contact might at least boost the effect of regular Internet-based self-help. However, when we looked at the proportion of participants no longer meeting criteria for panic disorder, the percentage was approximately the same. Hence, direct comparisons with live therapy are imperative in evaluating the specific value of adding short weekly telephone support. Should the two forms of treatment be equivalent, the cost of the Internet-based treatment is approximately 40% of that of 10-session in-person panic disorder treatment.
Apart from cost-effectiveness, one of the advantages of Internet-based self-help therapy is the possibility of treating people who would not otherwise seek treatment, for example, because of the fear of leaving their homes or traveling certain distances. By asking participants to come to a clinical selection interview, self-selection bias may be induced for people with less severe problems. This study was designed to target anyone suffering from panic disorder, whether he or she was able to travel or not. Therefore, we decided to administer the clinical interview over the telephone, which might compromise diagnostic reliability but has the advantage of bridging distances.
Because we did not include a comparison treatment, the specificity of the findings cannot be ensured. However, present knowledge would not support the role of alternative self-help treatments because cognitive behavior therapy has been found to be superior to other treatments for panic disorder
(25) . However, future studies ought to investigate the issue of the specificity of Internet-based self-help interventions, the role of community online support, and the nonspecific aspects of therapist contact that are likely to be present in both telephone and Internet consultations.
Because the research supervisors never met the participants in person, there was a risk of including those with too extreme suicidal tendencies. To minimize this risk, we excluded people who, according to the depression inventory self-report MADRS
(10), were suicidal. Hypothetically, this might have led to a group of people who were less depressed compared to participants in other studies. To our knowledge, there are three published bibliotherapy studies that have used the Beck Depression Inventory as a measure of depression. The average pretreatment depression scores in those studies were 14, 15, and 18 points, respectively
(2,
26, and
27 ). The treatment group in this study had an average Beck Depression Inventory score of 18 points, but it is still uncertain how the treatment would affect a more severely depressed group.
Another potential caveat from this study is that the educational level of the subjects was high compared to the general population. One in three Swedish adults ages 25 to 64 has some form of postsecondary education
(28) . That is considerably lower than in the present study, which raises the question of how well the treatment would work with individuals with lower levels of education. Also, because the subject group was selected from individuals who had expressed an interest in an Internet-administered self-help program for panic disorder or been on a waiting list and had been diagnosed over the telephone, it is possible that selection biases yield a more effective result for this treatment compared to standard live treatment. However, earlier studies in the same field have also used waiting lists (e.g., references
6,
7) .
There have been two recent studies testing Internet-guided self-help in the United Kingdom
(29,
30) . However, comparing results is difficult because there have been critical differences in inclusion criteria, follow-up times, and outcome measures. Moreover, the results of those studies have been questioned because the data were not analyzed in the same conservative way as in the present study (e.g., reference 31). However, it seems as if the U.K. program can be effective. The difference between the U.K. program and the present Swedish program is that the latter strongly encouraged interaction between the participants by means of discussion groups. Other unique features are the interactive quizzes and the compulsory and therapeutic e-mail correspondence between therapist and patient. Finally, the U.K. program has a primary focus on exposure alone, whereas the Swedish program emphasizes cognitive techniques as well as exposure.
The outcomes of this trial and previous Internet trials raise questions about how to implement these methods in clinical practice. Haaga
(32) suggested that not all patients need the same type and intensity of intervention. Some may be helped greatly by reading a self-help book, watching an instructional video, or using a computer program. Others could benefit from a brief psychoeducational group conducted by a paraprofessional, and still others may require long-term individual treatment from a highly trained professional therapist with specialized expertise. There already exists a stepped-care model for depression, including a self-administered treatment component
(33) . A similar model for panic disorder, backed up by empirical findings, would be welcome because psychiatric care has limited resources
(34,
35) . A step in that direction has been taken by Baillie and Rapee
(36), who have developed a prognostic scale that can be used to guide the choice of psychoeducation, self-help, or face-to-face therapy as the first step in stepped care. Hence, one should provide the time, expertise, and individual attention a patient needs but no more
(32) . The present study suggests that treatment credibility can be used as a predictor of treatment outcome, although correlations are small.
In sum, adding telephone contact to self-help treatment programs on the Internet is encouraged to reach clients in rural areas. Dismantling studies are strongly encouraged in order to evaluate the cost and benefit of briefer (no contact and shorter programs) or more intensive combined treatments (e.g., Internet plus live therapist sessions for severe cases).