The prognosis for adults with chronic fatigue syndrome is poor: most patients referred to specialist settings remain disabled and symptomatic for many years
(1). In randomized controlled trials, cognitive behavior therapy has been shown to improve functional impairment and fatigue for up to 8 months after treatment
(2,
3). Little is known about its long-term efficacy. The only such study we know of followed up 19 of 32 patients with chronic fatigue syndrome 4 years after treatment with cognitive behavior therapy and antidepressants: 14 continued to show improvement
(4). Unfortunately, many patients were untraceable, and the original study was nonrandomized and uncontrolled. It is therefore difficult to draw any firm conclusions about the long-term impact of cognitive behavior therapy.
It is important to know whether gains made with cognitive behavior therapy endure over time, particularly as chronic fatigue syndrome follows a variable course of partial remission and relapse. Observed treatment gains may be transient or cyclical
(5). The present study reports the long-term outcome of 60 patients with chronic fatigue syndrome who were treated with cognitive behavior therapy or relaxation therapy in a randomized, controlled trial 5 years earlier
(3). Our main questions were the following: 1) Would the gains made with cognitive behavior therapy be maintained at the 5-year follow-up? 2) Would cognitive behavior therapy be superior to relaxation therapy at the 5-year follow-up?
Method
The patients who entered the original randomized, controlled trial all met U.K. criteria for chronic fatigue syndrome: medically unexplained, disabling physical and mental fatigue, present more than 50% of the time for least 6 months
(6). They were typical of chronic fatigue syndrome patients seen in secondary care: they had illness with long duration and substantial functional impairment. Patients were randomly assigned to 13 sessions of either cognitive behavior therapy or a control condition consisting of relaxation therapy. Cognitive behavior therapy consisted of planned activity and rest, a sleep routine, graded increases in activity, and cognitive restructuring of unhelpful beliefs and assumptions. Relaxation therapy included progressive muscle relaxation and rapid relaxation. At the 6-month follow-up, patients undergoing cognitive behavior therapy scored significantly higher than patients in relaxation therapy on measures of global improvement, functional impairment, and fatigue but not on mood measures
(3).
All 60 patients were invited to an interview with an assessor who was blind to the patients’ treatment (K.H.). The patients were given a complete description of the study, and written informed consent was obtained. The assessor gave the patients some self-rated outcome questionnaires and conducted a structured interview. The interview included a checklist to determine whether patients fulfilled U.K. criteria for chronic fatigue syndrome
(6) and were deemed ill, as per a measure of current psychiatric disorder (the Revised Clinical Interview Schedule)
(7).
Dependent Variables
Global improvement was rated on a 7-point scale from “very much better” to “very much worse.” Ratings were collapsed into dichotomous categories: “much better” and “very much better” versus “a little better,” “unchanged,” “a little worse,” “much worse,” and “very much worse.”
The Medical Outcomes Study Short-Form General Health Survey
(8), a 20-item scale of physical functioning, measures limitations caused by ill health. Scores are transformed linearly into ratings on a scale ranging from 0 (limited in all activities) to 100 (able to carry out vigorous activities). A cutoff score of 83 was used to denote good outcome, as it represents the ability to carry out moderate activities (e.g., carrying purchases, moving furniture). This cutoff was used in the original trial
(3) and is similar to the mean in the U.K. general population
(9).
On the Fatigue Questionnaire
(10), eleven fatigue symptoms are rated on a four-option continuum from “less than usual” to “much more than usual” and scored bimodally (range=0–11). This scoring system gives an empirically validated cutoff: scores of 4 or higher indicate excessive fatigue
(10).
On the 12-item General Health Questionnaire
(11), depression and anxiety items are rated on a four-item continuum (“less than usual” to “more than usual”) and scored bimodally, giving an empirically validated cutoff: scores of 4 or higher indicate psychological distress
(11).
For relapse frequency, the patients were asked how many relapses they had experienced since treatment ended. For course of symptoms over time, the patients were asked to describe the course of their symptoms since the end of treatment. Responses were collapsed into two dichotomous categories of symptom severity: “consistently absent” and “mildly or steadily improved” versus “steadily worse,” “consistently severe,” “unchanged,” or “fluctuating markedly.” A structured checklist was used to determine whether the patients met U.K. criteria for chronic fatigue syndrome
(6). For employment status, patients were asked if they were currently employed and, if so, the number of hours worked per week.
Predetermined criteria for “complete recovery” required that patients no longer met chronic fatigue syndrome criteria, were employed full-time, and scored less than 4 on the Fatigue Questionnaire and more than 83 on the Medical Outcomes Study Short-Form General Health Survey physical functioning scale.
Statistical Analysis
Our statistical analysis was designed to provide clinically meaningful information about the patients who achieved a good outcome on each variable. Dependent variables were collapsed into predetermined dichotomous categories. Empirically validated cutoff points were used to identify good outcomes on the Fatigue Questionnaire, General Health Questionnaire, and Medical Outcomes Survey Short-Form General Health Survey physical functioning scale. Nonparametric tests were used to examine the patients in the cognitive behavior therapy and relaxation therapy groups who achieved a good outcome on each variable. All tests were two-tailed; significance was set at 5%, with use of all available data. Between-group comparisons were made by using the Mann-Whitney U test for continuous variables and Fisher’s exact test for dichotomous variables.
Results
Recruitment
Fifty-three (88%) of the 60 patients consented to participate in the follow-up study. Five patients (three with cognitive behavior therapy and two with relaxation therapy) refused to participate, and two (both with cognitive behavior therapy) were untraceable. Nonparticipants did not differ significantly from participants on any pre- or posttreatment demographic characteristic or clinical variable.
Patient Characteristics
The 53 patients who participated in the 5-year follow-up study had a mean age of 41.4 years (SD=10.4), 36 (68%) were female, 20 (38%) were deemed to have a psychiatric disorder as per the Revised Clinical Interview Schedule (adjusted for fatigue), and 26 (49%) were unemployed. Twenty-five had originally received cognitive behavior therapy, and 28 had received relaxation therapy.
Follow-Up
Since completing treatment at our facility, 14 (56%) of the patients undergoing cognitive behavior therapy and 16 (57%) of the patients receiving relaxation therapy reported receiving further treatment for their chronic fatigue symptoms. Six (21%) of the relaxation therapy patients had received cognitive behavior therapy (all had been offered cognitive behavior therapy at the 6-month follow-up). Other treatments used were antidepressants, counseling, physiotherapy, and complementary medicine. There were no significant differences among the patients who received other types of treatment during the follow-up interval.
Three patients among those in cognitive behavior therapy (12%) had a newly diagnosed medical condition that might have accounted for their chronic fatigue at the 5-year follow-up: one had cancer and was undergoing chemotherapy and two had celiac disease.
Comparison of Treatment Groups
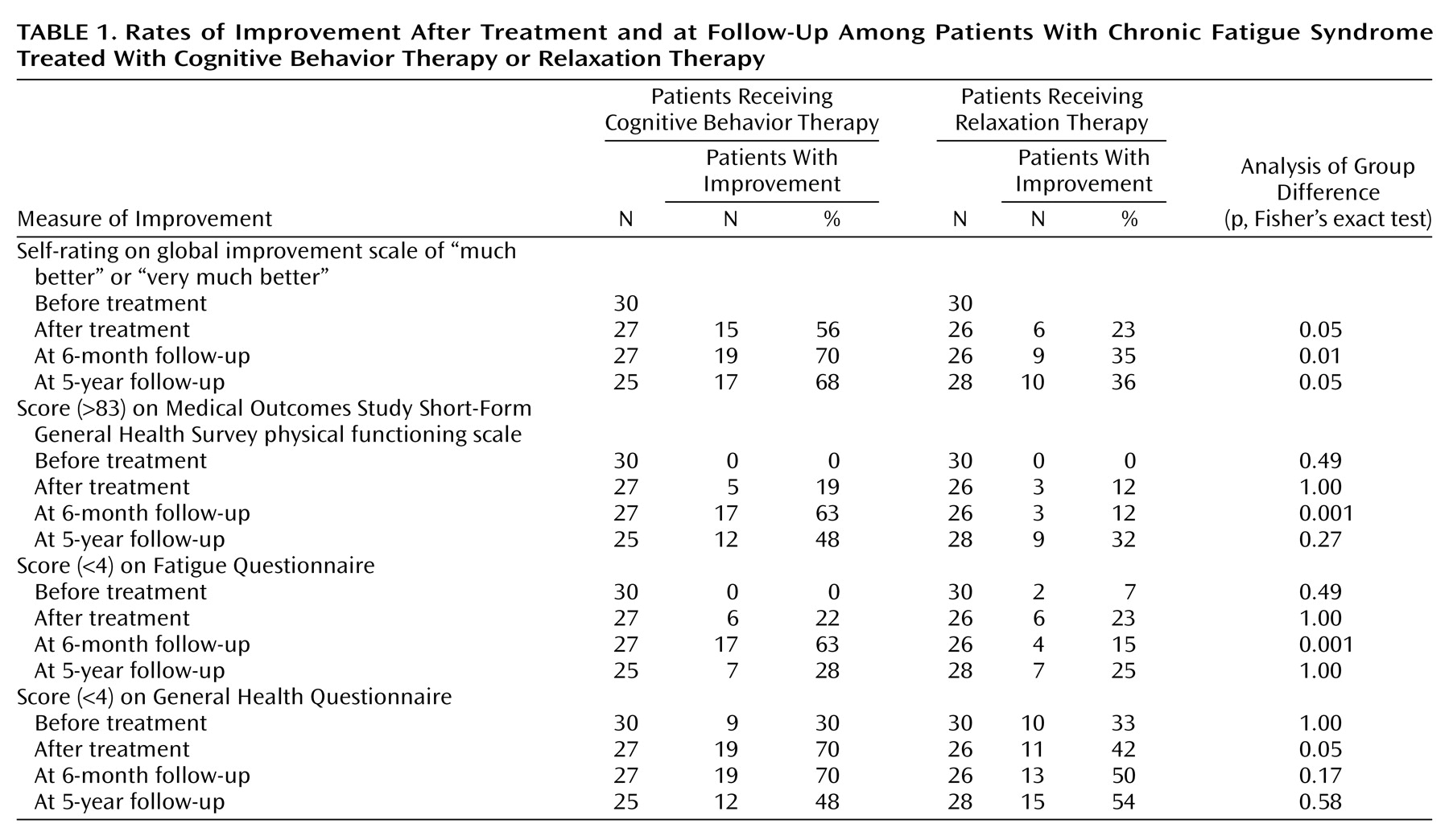
Table 1 shows outcome by original treatment group on self-rated questionnaires before and immediately after treatment and at the 6-month and 5-year follow-ups. A total of 17 (68%) of the patients who received cognitive behavior therapy and 10 (36%) who received relaxation therapy rated themselves as “much improved” or “very much improved” at the 5-year follow-up.
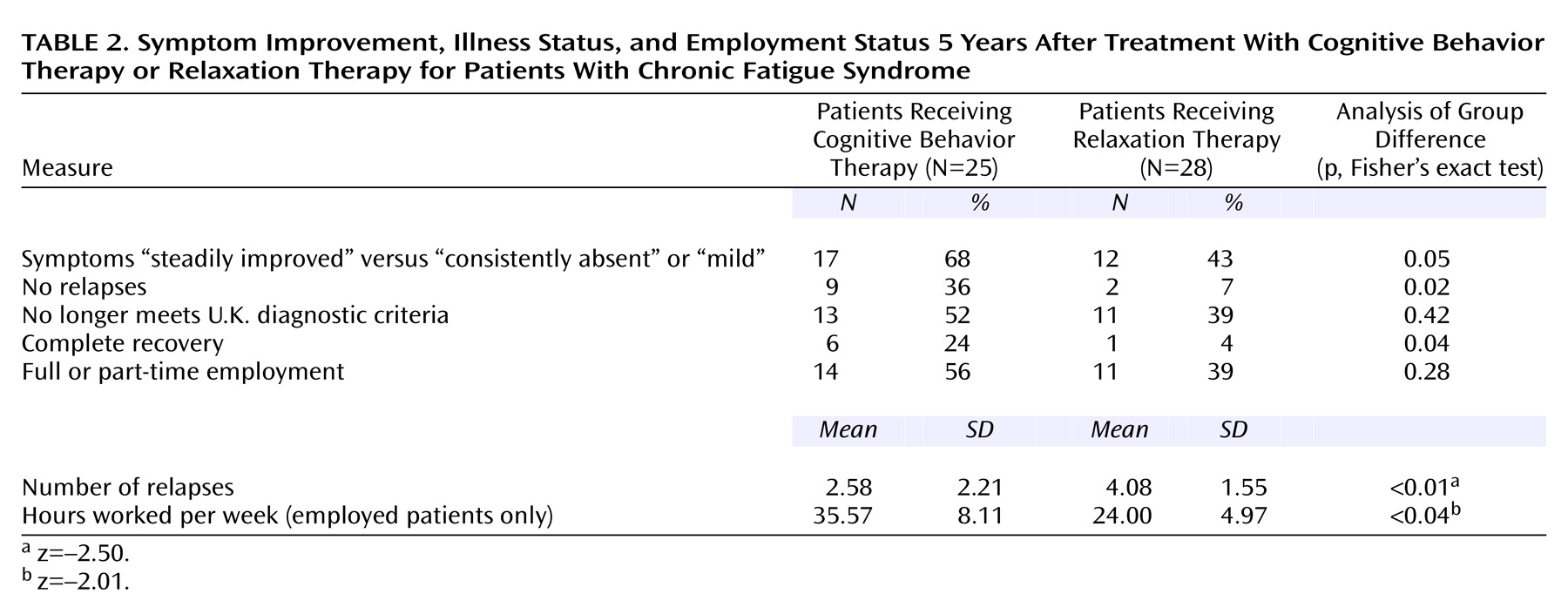
Table 2 shows improvement in symptoms and relapses since the end of treatment, current chronic fatigue syndrome and recovery status, and employment status and hours worked at 5-year follow-up, by original treatment group. Significantly more patients who received cognitive behavior therapy, in relation to those who received relaxation therapy, met criteria for complete recovery, were free of relapse, and experienced symptoms that had steadily improved or were consistently mild or absent since treatment ended. Similar proportions of patients were employed, but patients in the cognitive behavior therapy group worked significantly more mean hours per week.
Twenty (80%) of the patients in cognitive behavior therapy and 14 (50%) of the relaxation therapy patients rated treatment as “very useful” or “moderately useful” to them (p=0.04, Fisher’s exact test). Twenty-two (88%) of the cognitive behavior therapy patients and 17 (61%) of the relaxation therapy patients reported that they still used specific techniques learned during treatment (p=0.03, Fisher’s exact test).
Analyses were repeated to compare patients who received cognitive behavior therapy during or after the trial (N=31) with those who received relaxation therapy (N=22). Twenty-three (74%) of the cognitive behavior therapy patients and four (18%) of the relaxation therapy patients rated themselves as “much better” or “very much better” on our global improvement scale (p=0.001, Fisher’s exact test). On the physical functioning scale of the Medical Outcomes Study Short-Form General Health Survey, 16 (52%) of the cognitive behavior therapy patients and five (23%) of the relaxation therapy patients scored 83 or more (p=0.05, Fisher’s exact test). Twenty-three (74%) of the cognitive behavior therapy patients and seven (32%) of the relaxation therapy patients described their symptoms as “steadily improved” versus “consistently absent” or “mild” since treatment ended (p=0.01, Fisher’s exact test). Eleven (35%) of the cognitive behavior therapy patients and none of the relaxation therapy patients were free of relapse (p=0.01, Fisher’s exact test). Seven (23%) of the cognitive behavior therapy patients and none of the relaxation therapy patients were deemed completely recovered (p=0.03, Fisher’s exact test). Eighteen (58%) of the cognitive behavior therapy patients and seven (32%) of the relaxation therapy patients were employed (p=0.05, Fisher’s exact test).
There were no significant differences between the groups on cutoff scores on the Fatigue Questionnaire or the General Health Questionnaire. More patients treated with cognitive behavior therapy, than patients treated with relaxation therapy, tended to no longer meet the criteria for chronic fatigue syndrome; this finding approached significance: 17 of 31 (55%) cognitive behavior therapy patients and seven of 22 (32%) relaxation therapy patients (p=0.07, Fisher’s exact test).
Discussion
This study found that at the end of a randomized controlled trial, significantly more patients with chronic fatigue syndrome who were treated with cognitive behavior therapy had good outcomes at the 5-year follow-up than patients who received relaxation therapy. When original treatment groups were compared, significantly more cognitive behavior therapy patients rated themselves as “much better” or “very much better.” Significantly more cognitive behavior therapy patients met predetermined, stringent criteria for complete recovery, were free of relapse, and described their symptoms as “steadily improved” versus “consistently absent” or “mild” since treatment ended. The relaxation therapy group had significantly more relapses and more severe or unpredictable symptoms. Similar proportions in each group were employed, but mean hours worked per week were significantly greater in the cognitive behavior therapy group. Cognitive behavior therapy was evaluated positively, and most patients still used the treatment techniques 5 years later.
There were no significant differences between the groups on cutoff scores on the physical functioning scale of the Medical Outcomes Study Short-Form General Health Survey, the Fatigue Questionnaire, and the General Health Questionnaire, on chronic fatigue syndrome diagnostic criteria, and on employment status. The study may have had insufficient power to detect a true difference between groups. Of note, more relaxation therapy patients than cognitive behavior therapy patients participated in the follow-up study; three cognitive behavior therapy patients had a newly diagnosed medical condition that might have contributed to chronic fatigue, and six relaxation therapy patients received cognitive behavior therapy for chronic fatigue syndrome after the end of the original trial. It is noteworthy that a significantly greater proportion of the patients who received cognitive behavior therapy during or after the trial achieved a good outcome on more variables (including score on the physical functioning scale of the Medical Outcomes Study Short-Form General Health Survey and employment status) than the patients who received relaxation therapy only.
Relatively few patients crossed the threshold denoting “normal” levels of fatigue, despite achieving good outcomes on other measures. This may not be uncommon. People who recover from chronic fatigue syndrome often continue to score higher on the Fatigue Questionnaire than normal comparison subjects
(12). The results of the present study suggest that although many cognitive behavior therapy patients still experienced “excessive” fatigue at the end of 5 years, it had relatively little impact on their daily lives and was more predictable and controllable than before treatment. If so, this finding is largely in keeping with the intervention delivered: The main goal of cognitive behavior therapy was to help patients improve activity levels and quality of life, rather than overcome symptoms of the illness.
In the original trial, the proportion of patients in cognitive behavior therapy who achieved a good outcome on the Medical Outcomes Study Short-Form General Health Survey physical functioning scale, the Fatigue Questionnaire, and the General Health Questionnaire increased in the interval between the end of treatment and the 6-month follow-up. This proportion had decreased by the 6-month follow-up. This is not entirely surprising, since the patients had met with their therapists 1 month and 6 months after treatment. During this time they were encouraged to maintain a self-directed treatment program. It seems that once therapist contact ended at 6 months after treatment, some patients had difficulty making further progress unaided and may have become vulnerable to relapse. In the future, more attention could be paid to ensuring that gains are better maintained over time. It may be useful to extend the duration of treatment to include more attention to relapse prevention and to core beliefs and schema that could leave patients vulnerable to relapse. Regular follow-up sessions at widely spaced intervals for several years after treatment could also help patients make a successful phased return to work and achieve lasting lifestyle changes.
A recent longitudinal follow-up study
(13) showed that 91% of patients with chronic fatigue syndrome who received standard medical care continued to fulfill diagnostic criteria for chronic fatigue syndrome 4 years after their first assessment and that only 4% completely recovered. Other studies
(14–
16) have reported a comparable rate of recovery over a similar interval. A greater proportion of cognitive behavior therapy patients in the present study (including substantially fewer patients meeting chronic fatigue syndrome diagnostic criteria and patients with a higher recovery rate) appeared to have enjoyed more favorable long-term outcomes than comparable groups seen in secondary care.
Some caution should be exercised in interpreting the results of this study. First, there was no information from third parties, such as relatives or general practitioners. Second, the findings may not be applicable to chronic fatigue syndrome patients seen in primary care settings. Third, it is difficult to draw firm conclusions about the effect of cognitive behavior therapy, given that many of the patients received further treatment during follow-up. Finally, only 26% of the patients who received cognitive behavior therapy were judged completely recovered after 5 years, and almost one-half still fulfilled the criteria for chronic fatigue syndrome. This study demonstrates that while cognitive behavior therapy is not a “cure” for chronic fatigue syndrome, it can produce beneficial long-term effects on global, occupational, and physical functioning and symptom management. There is scope for refining treatment and improving the long-term maintenance of treatment gains.