Increasing evidence suggests that practice-based quality improvement programs for depressed primary care patients can improve the quality of care and a range of clinical and functional outcomes
(1–
3). Relatively little is known about the effectiveness of such programs for patients with depression and comorbid medical illnesses. In the current study we examine the effects of quality improvement programs for depression on treatment rates and outcomes for patients with depression and comorbid medical illnesses.
There are several reasons to suspect that quality improvement programs might have different effects for such patients than they do for depressed patients without comorbid medical illnesses. First, medical illnesses may complicate treatment decisions about depression. Second, treatments for depression could be less effective for patients with comorbid medical illness. There is some evidence in the literature to support both of these assumptions
(4,
5), although some studies of the elderly
(6) found no worse outcomes of depression among patients with comorbid medical illnesses.
The importance of resolving these issues is underscored by the high rates of depression
(7–
9) and high associated functional limitations and treatment costs for people with comorbid depression and medical illness
(10,
11). Uncertainty about the consequences of treatments or quality improvement programs for depression in the medically ill is attributable to several factors, including the tendency of efficacy studies to exclude patients with comorbid conditions
(12) and limited sample sizes in studies of quality improvement for separating out effects for clinically important subgroups.
The current study is based on Partners in Care, a randomized trial of two quality improvement programs for depression compared with usual care for managed primary care practices. Wells et al.
(3) reported that the two quality improvement programs resulted in higher rates of antidepressant and psychotherapy use and improved depression outcomes over a 12-month period. The incremental cost-effectiveness of the quality improvement programs was well within the range of other commonly accepted medical interventions in terms of costs per quality-adjusted life years
(13). Patients with the full range of comorbid medical conditions were included, and the number of subjects was sufficiently large to permit a comparative analysis of treatment rates and outcomes for depressed patients with and without comorbid medical illness overall as well as the impact of quality improvement programs on the rates of care and outcomes among the medically ill.
We hypothesized 1) that depressed primary care patients with comorbid medical conditions have worse outcomes than depressed patients without comorbid medical conditions; 2) that there are no differences in treatment rates for depressed patients with and without comorbid medical conditions; and 3) that a quality improvement program for depression improves treatment rates and health-related outcomes in patients with and without comorbid medical disorders.
Method
Study Design
Partners in Care, an Agency for Healthcare Research and Quality Patient Outcomes Research Team, was a group-level randomized controlled trial
(3,
14) carried out in six managed care organizations in five states. Forty-six of 48 clinics agreed to participate in the study, and 1,356 depressed patients were enrolled. Almost all primary care providers (181 of 183) agreed to participate in the study, including family practice physicians (N=96 [53%]), internists (N=60 [33%]), and nurse practitioners (N=25 [14%]).
Clinics were grouped into blocks of three clinic clusters each, matched for patient demographics, clinician specialty, and distance to mental health providers. A clinic cluster could be a single clinic, a group of small clinics, or a clinical care team within a large clinic. This created nine blocks, and within each block, clinic clusters were assigned randomly to care as usual or to one of two quality improvement programs (quality improvement with medications or quality improvement with therapy).
Patients were consecutively screened in waiting rooms of clinics between June 1996 and March 1997. Eligible patients were 18 years old or older and were determined to be depressed by a screening instrument that included the “stem” items for major depression and dysthymia from the 12-month Composite International Diagnostic Interview
(15) as well as items assessing the presence of depressive symptoms in the past month. Patients who had a medical emergency, did not speak English or Spanish, or did not have either insurance or a public-pay arrangement that covered the study treatments were excluded from the study. The institutional review boards of all participating institutions as well as the RAND Corporation approved the study. Written informed consent was obtained from all patients and clinicians.
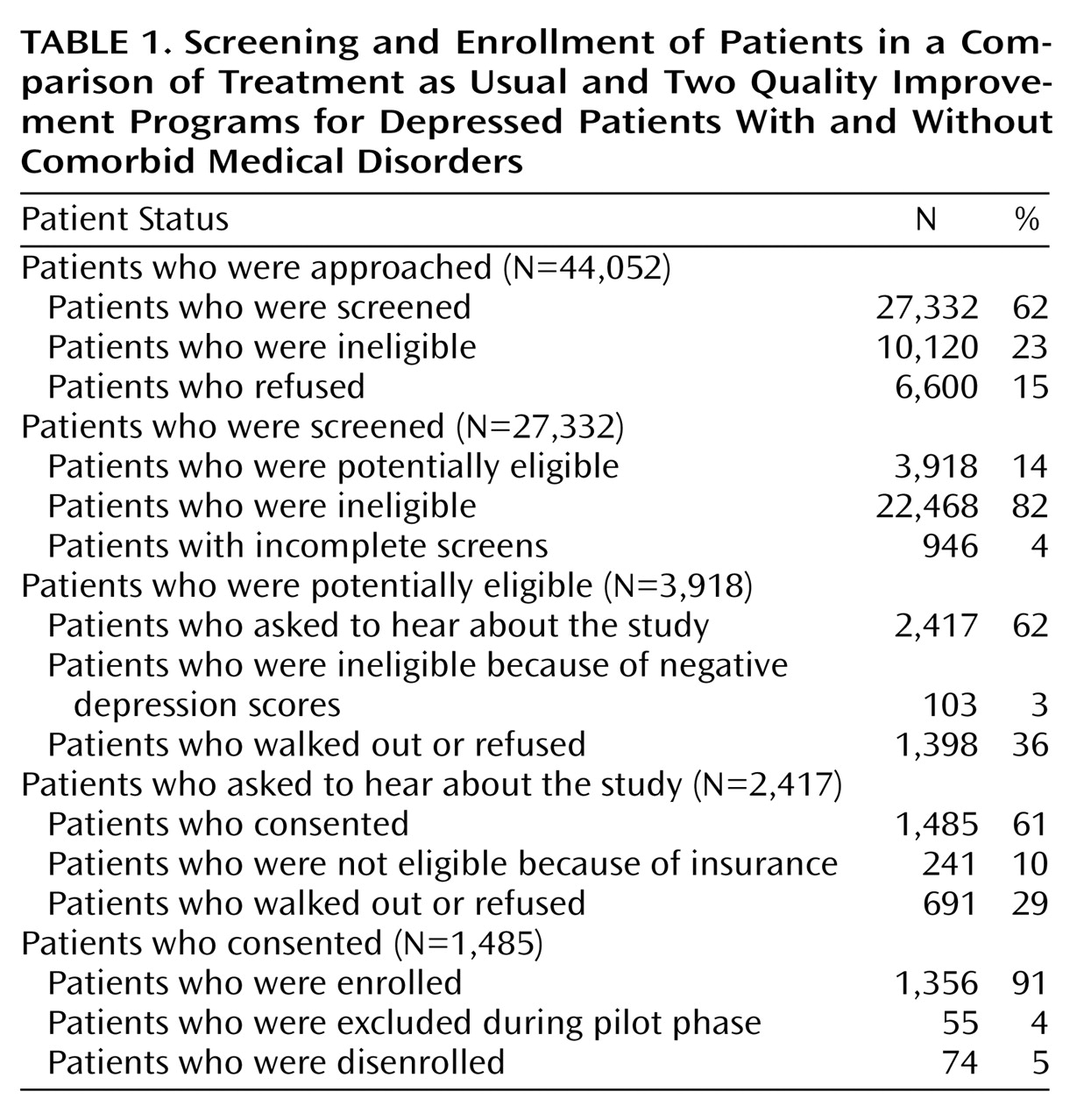
Table 1 shows the screening and enrollment process. A total of 27,332 patients completed the screening instrument, 3,918 were potentially eligible, and 1,356 enrolled. The enrolled sample included 443 patients who received care as usual, 424 who received quality improvement with medications, and 489 who received quality improvement with therapy.
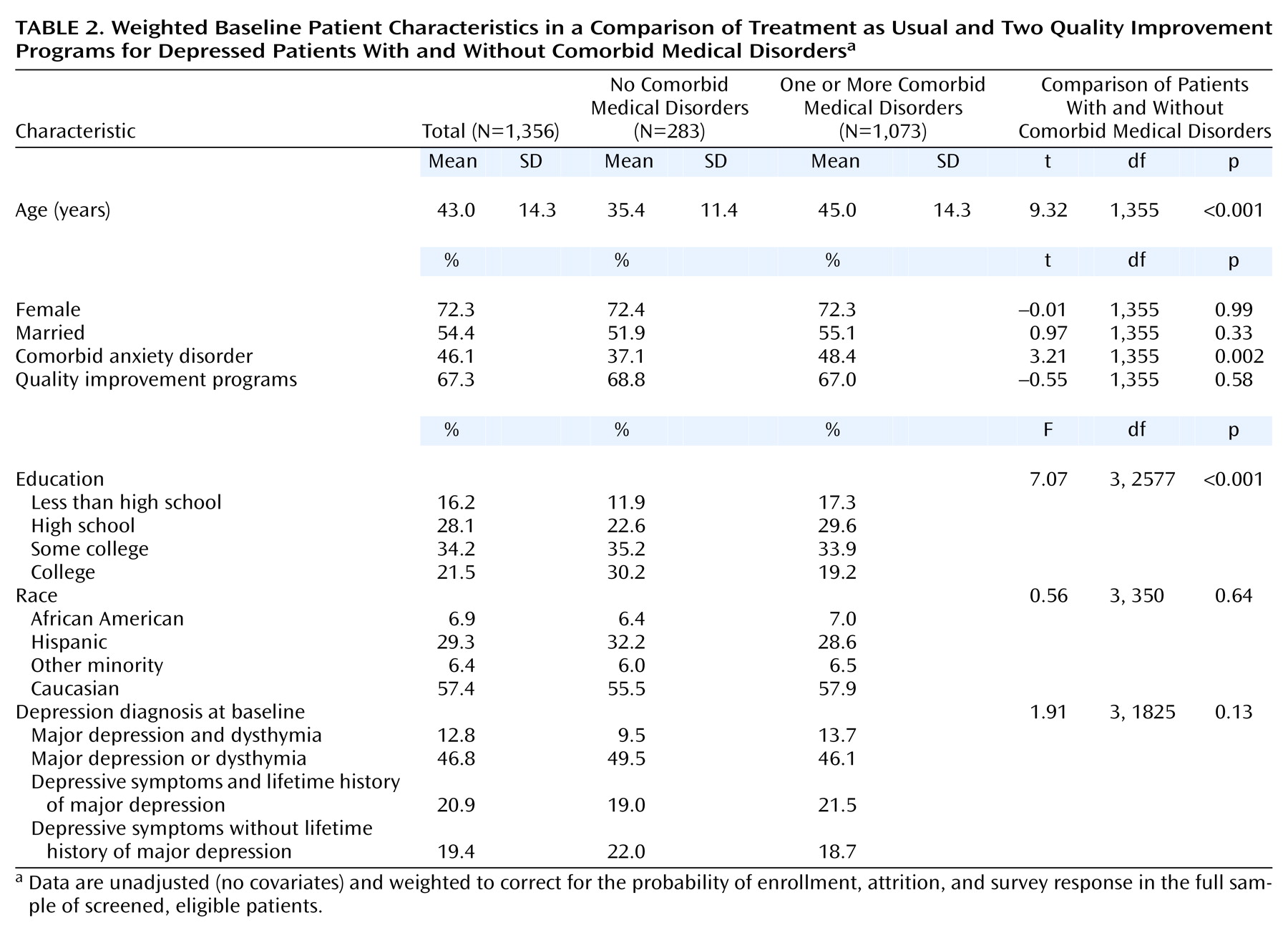
Table 2 shows characteristics of patients with and without comorbid medical illnesses; all presented data are weighted to correct for characteristics of the full screened, eligible, depressed sample. Patients with comorbid medical disorders were older, more likely to have a comorbid anxiety disorder, and less likely to be college educated. We controlled for these differences in subsequent analyses.
Quality Improvement Programs
The quality improvement programs used a combination of study expert intervention design, local managed care organization implementation, and patient and provider behavior change strategies
(16). Both quality improvement programs included screening, assessment, and patient education by a nurse depression specialist as well as education of primary care providers by local clinical teams. In addition to these core elements, quality improvement with medications provided ongoing access to the nurse depression specialist in the role of a case manager for 6 or 12 months (randomized at the patient level). Quality improvement with therapy provided trained psychotherapists who offered individual or group cognitive behavior therapy based on a manual by Miranda and Munoz
(17) at a reduced copayment rate. Patients in either quality improvement program could choose treatment with antidepressant medication, psychotherapy, or no treatment. More information on the programs can be found at the Partners in Care web site at http://www.rand.org/health/partners.care/portweb.
Measures
At baseline, 6 months, and 12 months, enrolled patients were asked to complete an interview that included the affective disorders section of the Composite International Diagnostic Interview and a self-administered mail survey. All instruments were translated into Spanish, and Spanish-speaking interviewers were used when appropriate for the telephone interviews.
Chronic medical conditions
Chronic medical conditions were assessed by using a set of self-report items derived from the Medical Outcomes Study
(10). Patients were asked if they currently had one or more of 19 medical problems. The frequency and percent of patients with each chronic medical condition were as follows: back problems (including disk or spine) (N=435 [37.6%]); migraine or other chronic severe headaches (N=338 [29.2%]); arthritis or rheumatism (N=315 [27.2%]); hypertension or high blood pressure (N=233 [20.1%]); trouble seeing (N=229 [19.8%]); asthma (N=144 [12.4%]); stomach ulcer (N=143 [12.3%]); high blood sugar or diabetes (N=142 [12.3%]); chronic inflammatory bowel disease, enteritis, or colitis (N=110 [9.5%]); thyroid disease (N=87 [7.5%]); trouble breathing—for example, that caused by emphysema or chronic lung disease (N=74 [6.4%]); heart disease other than angina or coronary artery disease (N=64 [5.5%]); a physical disability such as loss of an arm or leg, loss of eyesight or hearing, or birth defect (N=62 [5.4%]); angina or coronary artery disease (N=46 [4.0%]); a neurological condition such as epilepsy, convulsions, fainting spells, or Parkinson’s disease (N=36 [3.1%]); heart failure or congestive heart failure (N=23 [2.0%]); cancer diagnosed within the last 3 years (not skin cancer) (N=22 [1.9%]); stroke or major paralysis (N=15 [1.3%]); kidney failure (N=8 [0.7%]). (Percents are not based on N=1,356 because of missing data.)
For the purpose of our analyses, patients were defined as having a comorbid medical illness if they endorsed any of the 19 conditions. Wells et al.
(18) found that this type of patient self-report has reasonable validity for the more serious medical conditions. We analyzed medical comorbidity as a dichotomous variable; patients were categorized as having no comorbid chronic medical conditions or one or more comorbid chronic medical conditions.
Depression outcomes
Patients were defined as having probable depressive disorders if they had 2 weeks or more of depressed mood or loss of interest in pleasurable activities during the last year or persistent depression over the year plus at least 1 week of depression in the last 30 days. The screening instrument for probable depressive disorders was administered again at each follow-up survey.
Depressive symptoms at baseline and follow-up were assessed by using a 23-item version of the Center for Epidemiologic Studies Depression Scale (CES-D Scale)
(19) that was adapted by Dr. Daniel Ford (personal communication) to approximate the DSM-IV criteria for major depression. We report mean CES-D Scale values, scored on a scale from 0 to 100.
Patterns of care
Each survey assessed psychotropic medication use, and an indicator of whether the patient received any antidepressant medication in the past 6 months was developed.
Specialty counseling as an indicator of whether the patient had any individual, group, or family counseling by a specialist in the past 6 months was developed.
Since both antidepressant medications and psychotherapy may be considered appropriate depression treatment, we assessed whether patients reported receiving either antidepressant medications or specialty counseling during a given 6-month period.
Statistical Analyses
To test our first two hypotheses, that depressed patients with comorbid medical disorders have worse outcomes and similar rates of care as depressed patients without comorbid medical disorders, we estimated multivariate regression models with the presence or absence of a comorbid medical illness as the main independent variable. For CES-D Scale scores, we estimated linear models. For dichotomous outcomes, we performed logistic regression models. In both types of models we controlled for the following demographic and clinical factors: age (and age squared when appropriate); gender; marital status; education; household wealth ranked within age categories (using items modeled after the Health and Retirement Study
[20]); race; study “block” (matched sets of three clinic clusters within sites); comorbid anxiety disorder; mental health composite score from the 12-item Short-Form Health Survey
(21); depression diagnostic status at baseline (major depression or dysthymia, depressive symptoms and lifetime major depression, or depressive symptoms without lifetime major depression); and treatment status (quality improvement with medications, quality improvement with therapy, or care as usual). The two quality improvement programs had a common core and were both associated with improved depression care and outcomes over 12 months
(3). We combined them in our analyses to increase precision for analysis of the subgroup of patients with comorbid medical conditions and because we were most interested in the overall effect of quality improvement programs. To highlight the comparisons between groups, we generated adjusted (predicted) means and percentages using the parameters of the regression models.
To test our third hypothesis, we performed patient-level, intent-to-treat analyses for each dependent variable. To see if the treatments affected outcomes and rates of treatment for patients with comorbid medical illnesses, we tested an interaction of depression status with treatment status and conducted analyses stratified by comorbid medical illness status. We estimated multivariate regression models with combined treatment status as the main independent variable and the covariates listed above. For CES-D Scale scores, we estimated linear models, and for dichotomous outcomes we performed logistic regression models. Given the possibility that a higher rate of anxiety disorders in patients with comorbid medical illness could have contributed to their poor depression outcomes, we reran our analyses without anxiety disorders in our models. We found nearly identical results even when we did not control for anxiety in our analyses (results not shown).
We present standardized predictions of treatment effects for each outcome studied
(22). Regression parameters and each individual’s actual covariate values other than treatment status were used to drive two predicted values for each individual, first as a quality improvement program subject (quality improvement with medications or quality improvement with therapy), then as a care as usual subject. Predictions under the quality improvement with medications scenario were then averaged across the entire analytic sample to obtain an overall assessment of the treatment outcome. The procedure was then repeated for the other conditions. The procedure thus standardized the comparisons to the characteristics of the full analytic sample.
An extended hot-deck multiple-imputation technique was used to impute missing covariates at baseline. This technique modifies the predictive-mean-matching method
(23). Instead of filling in a single value for each missing value, we used Rubin’s multiple imputation strategy to create five imputed data sets
(24). Each of the five resulting data sets was then analyzed by using standard complete-data methods. The predictions across five imputed data sets were averaged, and standard errors were adjusted to reflect both within-imputation variability and between-imputation variability
(24–
26). For age, gender, comorbid anxiety disorder, depression diagnostic status at baseline, and study block, there were no missing data. For the other covariates, the percentage of imputed data ranged from 17.5% for mental health composite score to 2.1% for education.
Outcome variables were not imputed. Data were weighted to adjust for the probability of enrollment, attrition, and survey response and refer to all screened, eligible patients. Weights were developed through logistic regression equations for each step of screening, enrollment, and each survey; demographic factors, clinical indicators, site, and treatment status were used as predictors of participation, and then weights were multiplied across the different steps for each patient.
Results
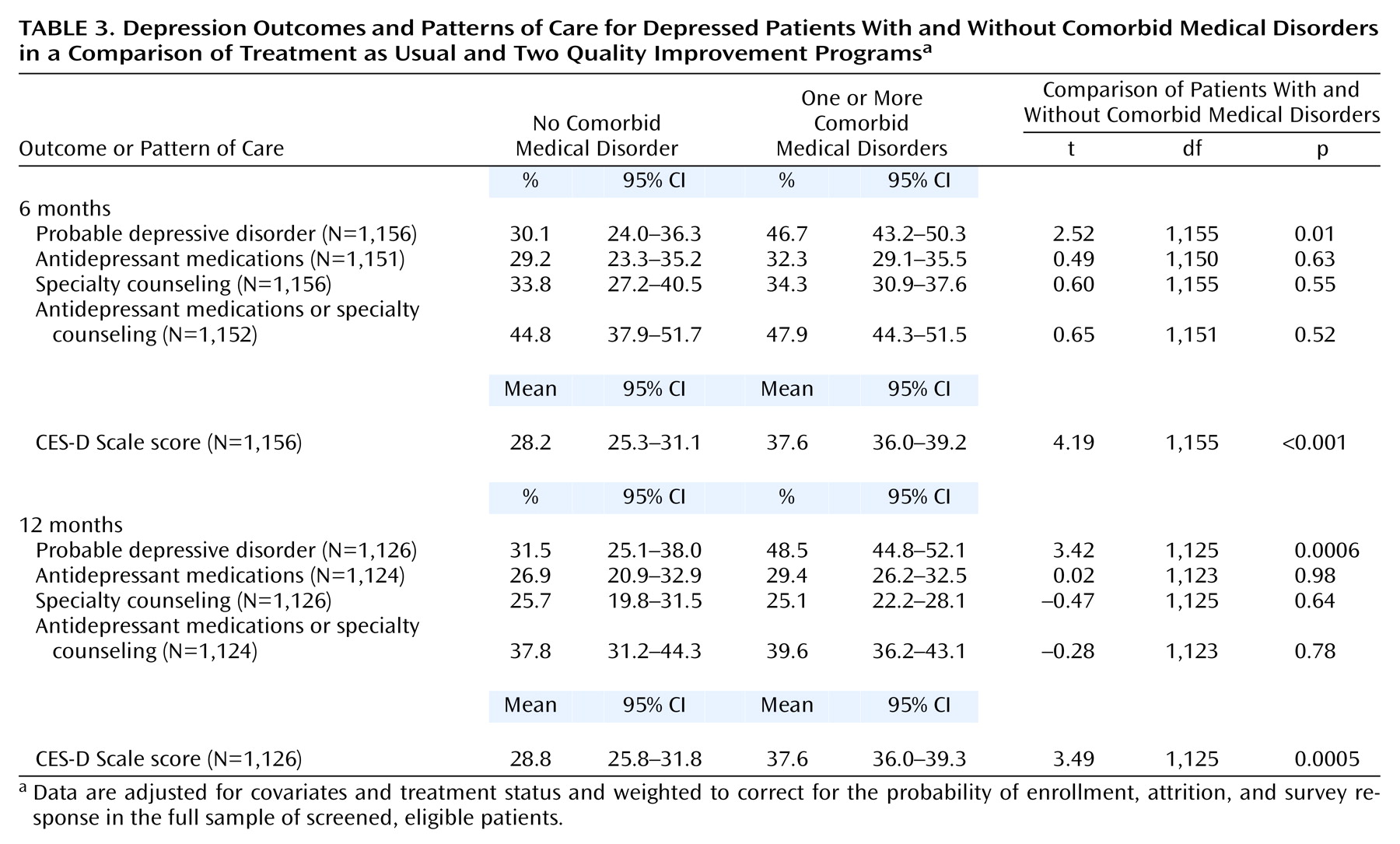
Table 3 compares depression outcomes in patients with and without comorbid medical conditions. At 6 months, probable depressive disorders were significantly more likely in patients with one or more comorbid medical condition than patients without comorbid medical conditions. Mean CES-D Scale scores were also significantly higher in patients with comorbid medical conditions than in those without. A nearly identical pattern was seen at 12 months.
At 6 months, antidepressant medication use for patients with one or more comorbid medical conditions was not significantly different from patients without comorbid medical conditions. Specialty counseling use was similar in patients with and without comorbid medical disorders. There were no significant differences in the rates of antidepressant use and specialty counseling between patients with and without comorbid medical conditions at 12 months.
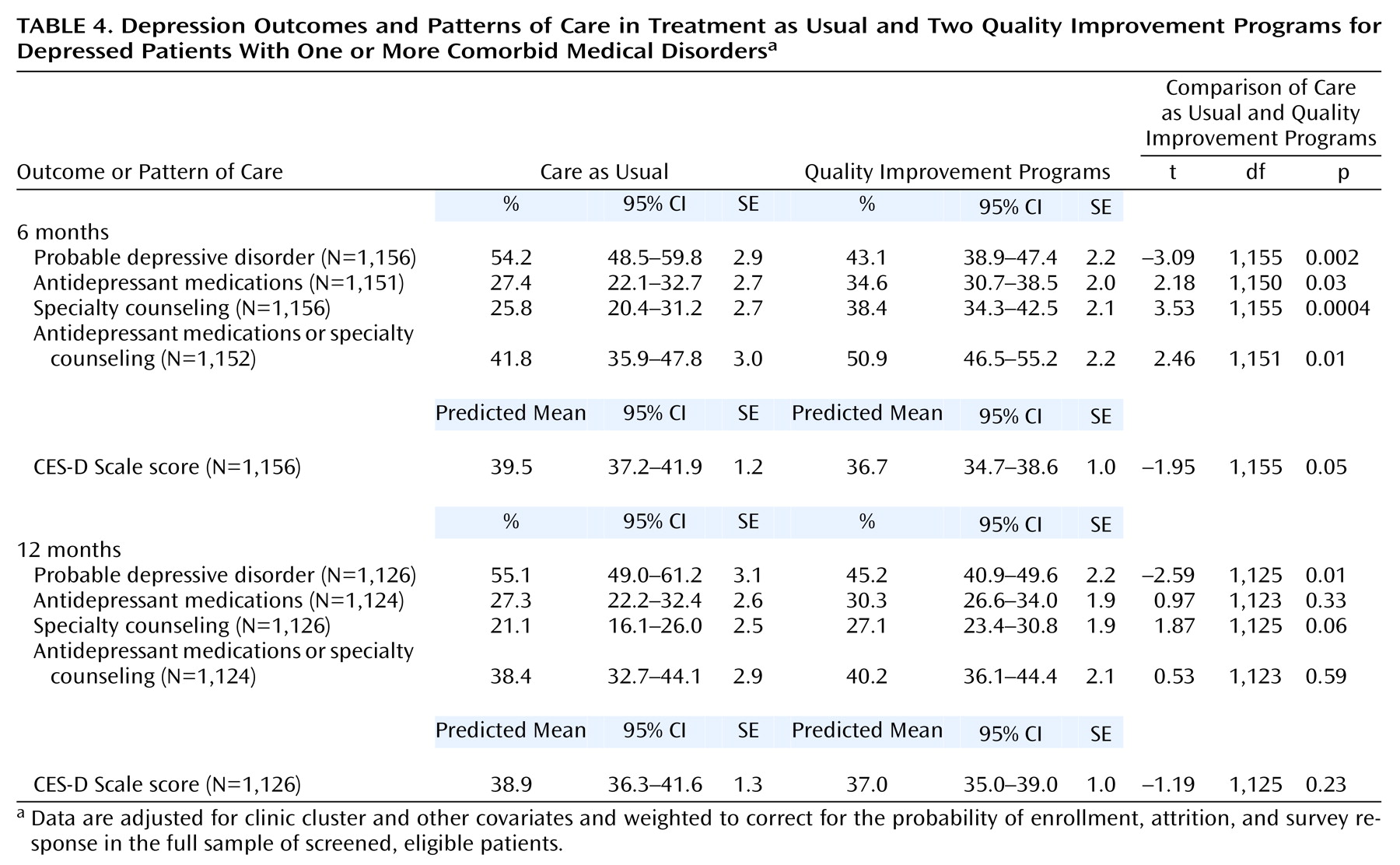
Table 4 compares the quality improvement programs with care as usual in patients with comorbid medical conditions. At 6 months significantly more patients in the quality improvement programs had probable depressive disorders than patients receiving care as usual. CES-D Scale scores were slightly lower in the quality improvement program patients than in the care as usual patients, but the difference was not statistically significant. In patients with comorbid medical conditions, antidepressant medication use for quality improvement program patients was significantly greater than for care as usual patients. Specialty counseling use was also significantly greater for quality improvement program patients than care as usual patients.
At 12 months, fewer quality improvement program patients than care as usual patients had probable depressive disorders. CES-D Scale scores were slightly lower in the quality improvement program patients than in care as usual patients, but this difference was not statistically significant. Antidepressant medication and specialty counseling use were slightly higher in the quality improvement program groups than in the care as usual patients, but this difference was also not statistically significant.
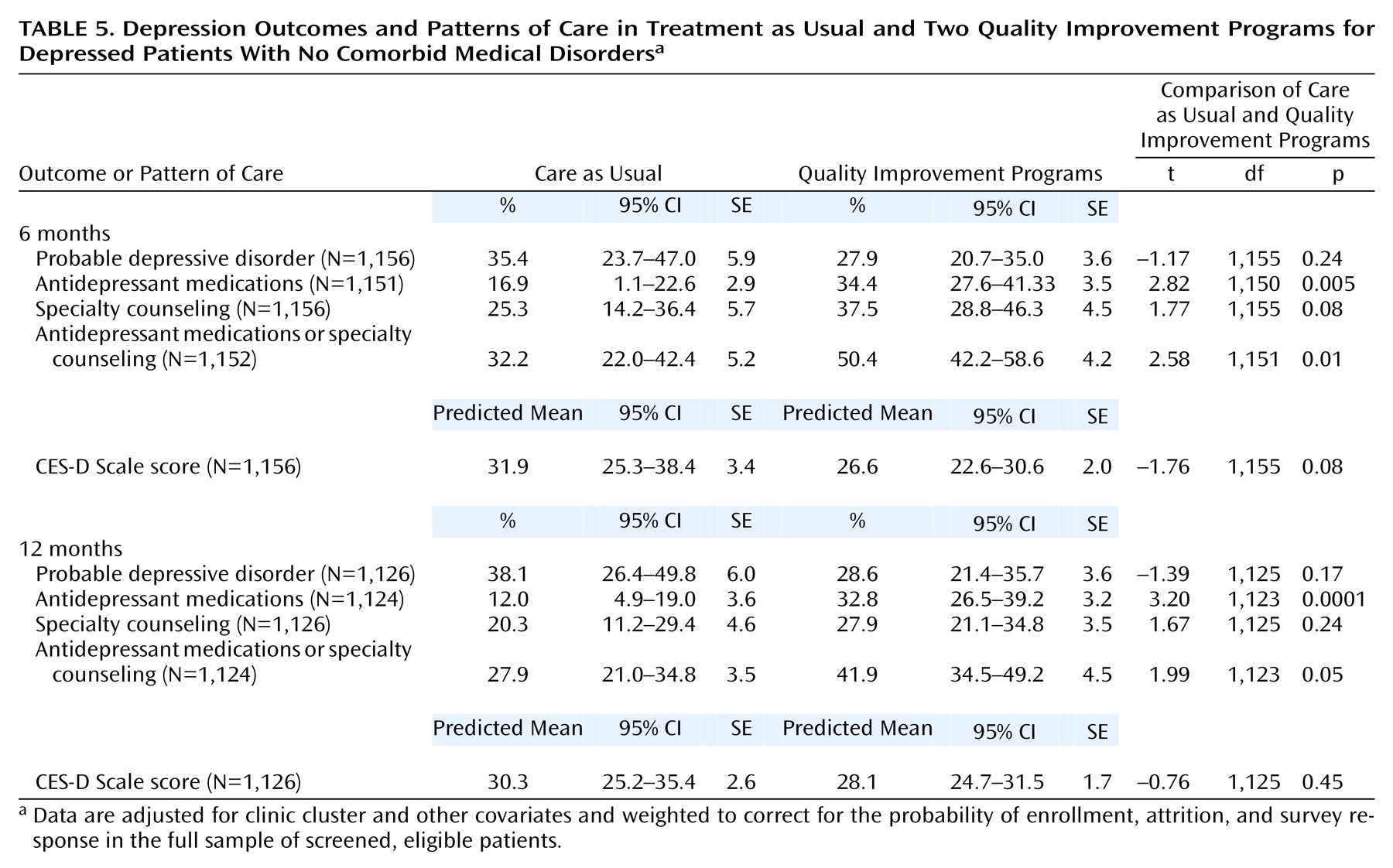
Table 5 compares the quality improvement programs with care as usual in patients without comorbid medical conditions. At 6 months, antidepressant medication use for quality improvement program patients was significantly greater than for care as usual patients. A nearly identical pattern was seen at 12 months. At both 6 and 12 months, quality improvement program patients had less probable depressive disorders and lower CES-D Scale scores than care as usual patients, but these differences were not statistically significant.
Discussion
We found that in depressed patients with comorbid medical disorders, quality improvement programs significantly reduced the likelihood of probable depressive disorders at 6- and 12-month follow-up. We also found that patients with comorbid medical conditions in these programs had higher rates of depression treatment than those in care as usual at 6 and 12 months (although the difference was not statistically significant at 12 months). Our results suggest that quality improvement programs implemented in real-world managed primary care settings can improve depression treatment and outcomes in patients with chronic medical conditions.
Even in the quality improvement program patients, however, more than 43% of those with comorbid medical conditions still had a probable depressive disorder at 6 months, and rates of treatment in quality improvement program patients with medical disorders were low despite the greater severity of depression in this group. The improvement in CES-D Scale scores for quality improvement program patients was modest and not statistically significant. The relatively modest effect of quality improvement programs on treatment rates is typical of effective quality improvement programs, which focus not on treating every patient but on fostering conditions that increase the likelihood of treatment for a pool of at-risk patients. We also found that the desirable effect of the quality improvement programs on treatment appeared to be wearing off and the favorable depression outcomes were less prominent at 12 months. Further interventions may be needed to sustain quality improvement effects on both patient and provider behavior
(2,
27).
It should be pointed out that this was an effectiveness study in which regular primary care providers in nonacademic primary care practices delivered the treatments rather than a research team, increasing the generalizability of findings. Under such circumstances, it may be particularly challenging to implement and sustain the improvements or to reach the majority of depressed patients not already identified by the practice as depressed.
This study also found that patients with comorbid medical conditions had significantly more continued depression than patients without comorbid medical conditions at both 6 and 12 months. These results are consistent with our first hypothesis and the general belief that comorbid medical disorders are associated with poor outcomes for depressed patients. Some studies suggest that medical clinicians fail to detect depression or to institute appropriate treatment when comorbid medical conditions are present
(5,
10,
28,
29). However, we found that patients with chronic medical conditions were actually more likely to receive appropriate antidepressant medications and specialty counseling than those without, although these differences were not statistically significant. At this point the etiologic mechanisms underlying the relationship of depression and physical illness are still uncertain.
Our results are consistent with our second hypothesis that despite having worse depression, patients with comorbid medical disorders do not have higher rates of depression treatment than patients without comorbid medical disorders. These results are of concern, especially considering that patients with medical conditions are more likely to see their primary care physicians and thus have more opportunities to have their depression treated. These results suggest a need for greater recognition and treatment of depressed patients with comorbid medical disorders, perhaps in the form of care management programs that integrate the management of medical illnesses and depression.
We also looked at rates and outcomes of treatment in the group of subjects without comorbid medical disorders. We found a similar effect of quality improvement on rates of depression treatment and outcomes, but differences between the quality improvement program groups and the usual care patients were not always significant.
There are several limitations to our study. There are a number of diagnostic problems involved in measuring depression in chronically medically ill patients. Symptoms that we might attribute to depression, such as weight changes, fatigue, sleep difficulties, and appetite disturbance, may be attributable to medical conditions. Thus patients with medical illness may have artificially inflated scores on the CES-D Scale and appear more depressed than patients without comorbid medical illnesses. We measured chronic medical illness by patient self-report and not from their medical records. We also used a simple count of chronic medical conditions rather than weighting these conditions by severity or impact. There was substantial sample loss during enrollment, but only somewhat more than in an observational study
(3). Finally, the study took place in managed primary care settings, thus limiting the generalizability of our results in non-managed-care settings.
Conclusions
The treatment of patients with depression and comorbid medical disorders is an important challenge for primary care. The results of our study suggest that patients with comorbid medical disorders have worse depression outcomes but not significantly higher rates of treatment than those without chronic medical illnesses, calling for increased efforts to recognize and treat depression in patients with comorbid medical illness. The encouraging news is that primary care patients with comorbid medical disorders can benefit from quality improvement programs for depression. This has implications for both practice and research. Given these results, greater efforts should be made to include the medically ill when implementing quality improvement programs for depression, and there is no real justification for excluding them from either studies of depression treatments or opportunities for depression treatment in practice.