Bipolar disorder is a chronic psychiatric illness that often begins in adolescence. Comprehensive studies of moderate- to long-term outcome in patients with adolescent-onset bipolar disorder have only just begun to be reported
(1–
5). In a previous paper, we reported on a group of adolescents with bipolar I disorder, the large majority of whom had an overall profile of good premorbid academic functioning that deteriorated over 4 years after the onset of bipolar illness
(6). After illness onset, areas of language, art, athletics, or music were identified as academic strengths by 95% of the adolescents’ teachers, whereas mathematics was ranked the most problematic area of study by 60% of the teachers. To our knowledge this was the first and only report describing mathematical deficits in youth with bipolar disorder.
Academic difficulties in adolescents with bipolar disorder have been attributed primarily to adjustment problems, the effects of multiple hospitalizations, and difficulties with peers
(7–
10). Although a variety of psychosocial difficulties may be associated with poor school performance in this population, it is premature to conclude that academic difficulties, such as problems with language or mathematics, are a result of psychosocial factors alone. Cognitive deficits associated with psychotic illnesses have been described in schizophrenic youth with academic difficulties
(11–
13), and the academic delay previously described in adolescents with bipolar disorder
(3,
6) may result at least in part from cognitive difficulties.
As described by Geary
(14), arithmetic deficits can be due to underlying deficiencies in a number of cognitive processes, including retrieval of arithmetic facts from semantic memory, execution of arithmetical procedures, or visuospatial representation. Historically, research has demonstrated that patients with a specific brain lesion in the left parietal region have acquired acalculia, a disorder characterized by loss of calculation ability
(15).
More recent functional imaging studies have demonstrated that mathematical reasoning involves a distributed network, including the lateral and ventral lateral prefrontal cortex and the posterior parietal lobe, as well as subcortical regions such as the caudate nucleus and cerebellum
(16–
20). Specific deficits in mathematical reasoning associated with some diseases have been correlated with abnormalities in brain structure. For example, mathematics deficits in children with velocardiofacial syndrome have been related to structural abnormalities in the parietal lobe region
(21).
As part of a comprehensive study of moderate-term outcome in adolescent bipolar disorder, we compared the academic (mathematics, reading, and spelling) ability of a group of adolescents with bipolar disorder during illness remission to that of normal comparison subjects and adolescents with unipolar depression in remission. On the basis of our previous findings suggesting that mathematics is a problem area for youth with bipolar disorder
(6), we hypothesized that the bipolar disorder group would demonstrate significantly greater deficits in mathematics than the comparison group or the unipolar depression group.
Method
Forty-four adolescents with bipolar I disorder (17 male subjects, 27 female subjects; mean age=19.4 years, SD=2.9; mean grade in school=11.2, SD=1.1), 30 adolescents with major depressive disorder (nine male subjects, 21 female subjects; mean age=18.5 years, SD=2.8; mean grade=10.3, SD=1.6), and 45 comparison subjects with no psychiatric history (19 male subjects, 26 female subjects; mean age=18.2 years, SD=1.6; mean grade=11.4, SD=0.8) were included in the study. All participants gave written informed consent after the study procedures were explained. The study procedures were approved according to institutional guidelines. DSM-III-R diagnoses of bipolar I disorder or major depressive disorder were confirmed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children
(22) and the Mini Structured Clinical Interview for DSM-III-R, computerized version
(23). At the time of study participation, both mood disorder cohorts were in remission, as defined by: 1) not meeting DSM-IV criteria for a current episode of a mood disorder (including dysthymia), 2) no hospitalizations for psychiatric reasons within the preceding 6 months, 3) no history of organic brain illness or head trauma, and 4) a Beck Depression Inventory
(24) score of <13. Further details about the study and the demographic characteristics of subjects’ families have been provided in greater detail elsewhere
(25).
All subjects completed two standardized academic tests, the Wide-Range Achievement Test–Revised 2 (WRAT-R2)
(26) and the Peabody Individual Achievement Test
(27). The ratio of attempted versus not attempted items on the mathematics section of the WRAT-R2 and the ratio of correct versus incorrect responses were determined. WRAT-R2 grade lags were computed by subtracting the subject’s grade level obtained by means of the WRAT-R2 from the last grade completed by the subject (negative scores indicated that the WRAT-R2 score was below the expected grade level). WRAT-R2 and Peabody Individual Achievement Test percentile scores were compared to age norms provided with the tests. To assess functional mathematical ability, subjects completed the money and marketing subtest of the Bay Area Functional Performance Evaluation Task-Oriented Assessment
(28). Nonverbal intelligence was assessed with the standardized Test of Nonverbal Intelligence—2
(29); percentile scores were compared to age norms provided with the test. The question on mathematical achievement from the Social Adjustment Inventory for Children and Adolescents
(30) was used to determine the subjects’ subjective evaluation of their mathematical achievement during the last school year.
Continuous variables were examined by two-way analysis of variance and Bonferroni post hoc tests. Categorical variables were analyzed with Pearson chi-square tests. Standard linear regression techniques were used to examine linear trends of mean scores across ages. Significance level was set a priori at p<0.05.
Results
Significantly more adolescents with bipolar disorder (84.1%) had been previously hospitalized for a mood episode, compared to adolescents with major depressive disorder (30%) (χ2=22.2, df=1, p<0.001). The mean length of illness, as calculated from the first report of mood episode onset to the time of study participation, did not differentiate the clinical groups (4.5 years, SD=2.9 for the bipolar disorder group, versus 4.1 years, SD=2.0 for the major depressive disorder group). The adolescents with bipolar disorder had experienced a mean of 1.5 episodes of mania (SD=1.4) and 1.7 episodes of depression (SD=2.1). The mean number of depressive episodes for the adolescents with major depressive disorder was 1.3 (SD=0.9). The three study groups’ scores on the Test of Nonverbal Intellegence—2 were not significantly different (bipolar disorder group: mean=100.2, SD=16.6; major depressive disorder group: mean=101.2, SD=12.6; comparison group: mean=100.1, SD=14.1) (F=0.06, df=2, 116, 188, n.s.).
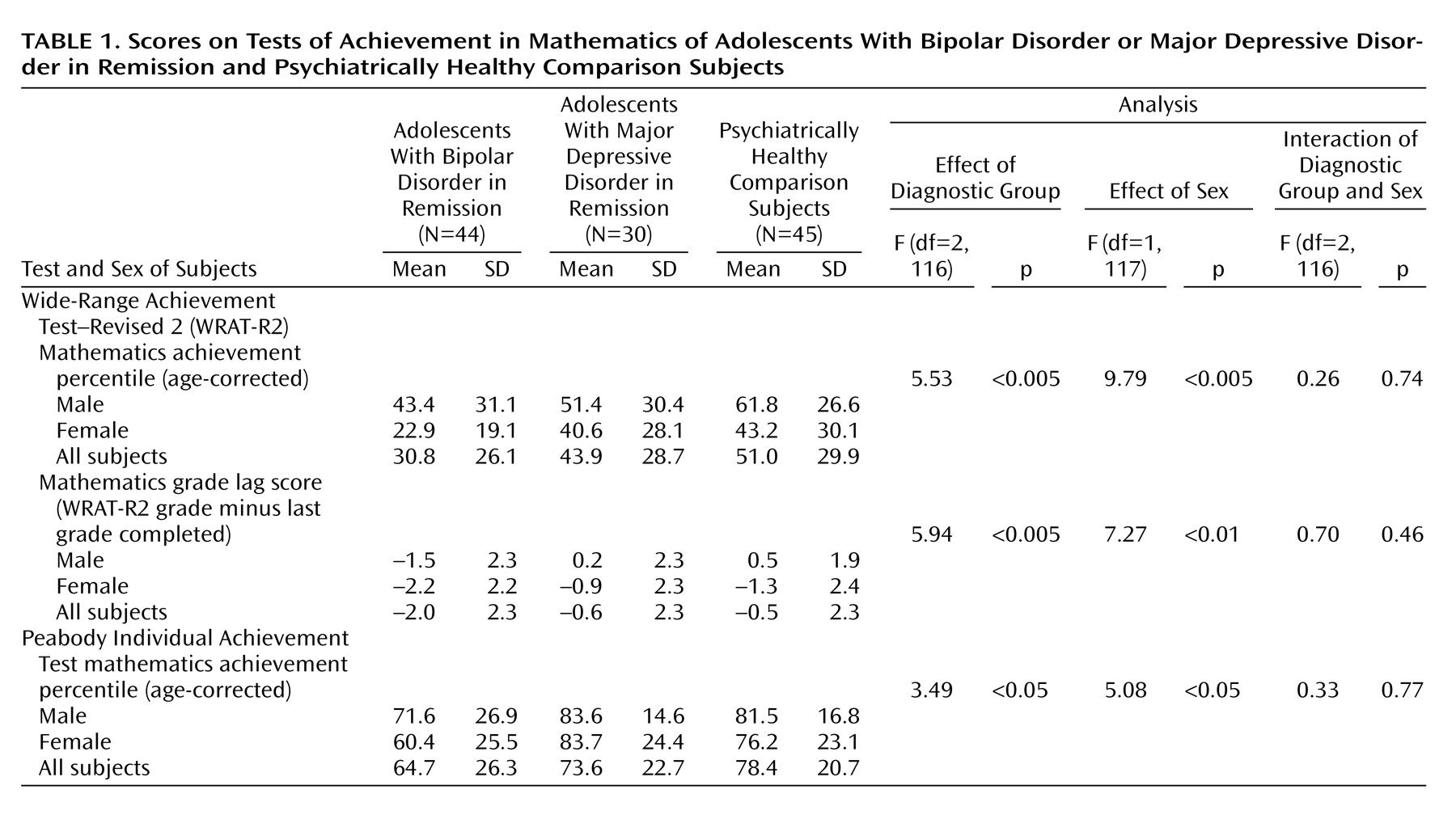
No significant between-group differences were found in the WRAT-R2 reading or spelling subtest scores. In contrast, on the WRAT-R2 mathematics subtest, the bipolar disorder group had significantly poorer scores than the comparison group (p<0.005, Bonferroni) (
Table 1). The mean for the major depressive disorder group was intermediate between the means for other two groups. The differences between the WRAT-R2-obtained grade level and the last grade completed showed a 2-year academic lag in mathematics for the bipolar disorder group, which was significantly larger than lag for the major depressive disorder group (p<0.05, Bonferroni) and the comparison group (p<0.01, Bonferroni) (
Table 1). By contrast, for grade levels in reading and spelling, no group showed an academic lag, and there were no significant between-group differences.
Analyses of the WRAT-R2 mathematics items showed significant between-group differences in the mean number of items attempted (F=7.27, df=2, 116, p<0.001) and correctly answered (F=6.38, df=2, 116, p<0.01). The bipolar disorder group attempted and correctly answered fewer items than the major depressive disorder group (p<0.05, Bonferroni) or the comparison group (p<0.01, Bonferroni). All groups displayed a “normal” age-related developmental trend in WRAT-R2 reading and spelling test scores, with scores incrementally increasing with age (reading: r=0.38, p<0.0001, N=119; spelling: r=0.36, p<0.0001, N=119). The WRAT-R2 raw scores for mathematics did not covary significantly with age (r=0.92, p=0.32, N=119) but were associated with clinical status and sex (bipolar disorder group < major depressive disorder group < comparison group: F=4.95, df=2, 116, p=0.009 and gender (female subjects < male subjects: F=8.42, df=1, 117, p<0.004).
The data for the Peabody Individual Achievement Test showed no significant group differences in reading achievement. Paralleling the WRAT-R2 findings, in mathematical achievement, the adolescents with bipolar disorder performed at a significantly lower age-corrected percentile ranking than the comparison subjects (p<0.05, Bonferroni) (
Table 1).
On the Bay Area Functional Performance Evaluation functional mathematics test, there was a significant between-group difference in time to complete the mathematics task (F=30.28, df=2, 116, p<0.001), with the bipolar disorder group requiring more time to complete the task (mean=372 seconds, SD=114) than the major depressive disorder group (mean=247 seconds, SD=75) (p<0.001, Bonferroni) and the comparison group (mean=237 seconds, SD=77) (p<0.001, Bonferroni). No significant between-group differences in task accuracy were observed.
With respect to the question on mathematical achievement from the Social Adjustment Inventory for Children and Adolescents, 9% of the adolescents with bipolar disorder reported above-average achievement in mathematics, in contrast to 25% of the adolescents with major depressive disorder and 32% of the comparison subjects (χ2=7.82, df=2, p=0.02). Below-average achievement was reported by 27%, 25%, and 18% of the bipolar disorder, major depressive disorder, and comparison groups, respectively. Only adolescents with a mood disorder (30% of the adolescents with bipolar disorder and 29% of the adolescents with major depressive disorder) reported failing mathematics in the last academic year.
Discussion
This study demonstrated that adolescents with bipolar I disorder in remission had significantly poorer mathematics scores on standardized testing and reported significantly poorer mathematical functioning in school, compared to youth with major depressive disorder and psychiatrically healthy peers. Furthermore, female adolescents performed poorer on all mathematics tests, and an absence of expected age-related increments in mathematics skills was noted for adolescents with mood disorders. In contrast, there were no significant group diferences in language scores (reading or spelling) or in nonverbal intelligence scores. To our knowledge, these are novel findings. These results are consistent with our earlier report
(6) that identified mathematics as the most problematic area of study for adolescents with bipolar disorder, as identified by corroborative teacher reports.
Adolescents with bipolar disorder had lower mean scores (30th percentile) on the WRAT-R2 than on the Peabody Individual Achievement Test (64th percentile). One possible reason for this difference could be differences in test presentation. The WRAT-R2 is a written, timed task, and the Peabody Individual Achievement Test consists of multiple-choice items and is not timed. One hypothesis, supported by our finding that the bipolar disorder group answered fewer questions on the WRAT-R2 than the other groups, is that adolescents with bipolar disorder have a slower response time, leading to poorer performance on the WRAT-R2. This interpretation is also supported by results for the Bay Area Functional Performance Evaluation mathematics assessment; adolescents with bipolar disorder took longer to complete this assessment, compared to the adolescents with major depressive disorder and the comparison subjects. In contrast, and independent of response time, the adolescents with bipolar disorder had more incorrect answers on the WRAT-R2 questions they attempted than did the adolescents with major depressive disorder and the comparison subjects. Furthermore, on the untimed Peabody Individual Achievement Test, the adolescents with bipolar disorder performed at a lower level than the comparison subjects. These findings suggest that a slower response speed may not be the sole factor underlying the mathematics deficits found in adolescents with bipolar disorder.
Our analysis of the findings for the WRAT-R2 items suggests that youth with remitted bipolar disorder have significant mathematics difficulties that are not simply computational (basic addition, subtraction, multiplication, or division) but may also involve the organizational, spatial, and meta-cognitive aspects of mathematical performance. These findings support the hypothesis that impairments in cognitive processes may underlie the pattern of mathematical deficits observed in the subjects with bipolar disorder. Investigations examining the different cognitive components of mathematics performance in youth with other medical illnesses have identified particular cognitive deficits associated with specific mathematics deficits. For example, significant deficits in children with Turner’s syndrome have been linked to weaker visuospatial skills and poorer organizational ability in mathematics procedures
(31); in boys with ADHD specific mathematics deficits have been linked with lower problem-solving scores and slower computational performance
(32). There is also evidence that poorer mathematical ability is predicted by poor executive functioning
(33). Previous findings that adults with bipolar disorder have difficulties with executive functioning during euthymic periods
(34) suggest that mathematical deficits in youth with bipolar disorder in remission could be related to difficulties with executive functioning. In disagreement with this speculation was our finding that the adolescents with bipolar disorder in this study had age-appropriate scores on a test of executive functioning (Wisconsin Card Sorting Test). In addition, we found no significant differences in performance on this measure between bipolar disorder, major depressive disorder, and comparison groups (data not shown).
One way to try to understand the cognitive deficit that may underlie mathematics deficits in youth with bipolar disorder could be to determine the etiology within the brain. Recently presented functional magnetic resonance imaging data from our center demonstrated that adolescents with bipolar disorder who are performing mathematical calculations do not show activation of the dorsolateral prefrontal cortex to the same extent as comparison subjects (personal communication, F. McMaster, 2001). This preliminary evidence is supported by recent imaging work suggesting that the dorsolateral prefrontal cortex is involved in overall mathematical processing
(16).
The results of this study should be interpreted with caution in light of its limitations. The subjects with mood disorder in this study were attending specialized clinics within an academic health science center, and our findings may not be translatable to youth in nonacademic treatment facilities or to those with bipolar II disorder. Although we examined the relationship between mathematics performance and the effects of age and sex, future targeted investigations should be conducted to assess whether observed mathematical deficits correlate with particular characteristics of pharmacological or psychosocial treatment or with specific illness parameters or comorbid psychiatric conditions.
Conclusions
In a group of adolescents with bipolar I disorder in remission, mathematical deficits were observed in the absence of any significant mood symptoms. The relationship between these deficits and mood fluctuation should be examined. In addition to being present after remission from illness, these mathematical deficits may be present before illness onset and may worsen during the illness course. These findings suggest that remedial academic interventions in mathematics are warranted for adolescents with treated bipolar I disorder and that comprehensive treatment plans for these patients should include input from hospital educators and school authorities.