Delusional thoughts are common in patients with Alzheimer’s disease and are associated with considerable morbidity. Studies indicate that delusions are present in approximately 30%–40% of patients with Alzheimer’s disease
(1–
4), fluctuate over time but often persist
(5–
7), and are associated with aggressive behaviors
(8,
9) and more rapid cognitive decline
(1). Delusions and other noncognitive symptoms in Alzheimer’s disease contribute prominently to caregiver distress
(10) and decisions to place the patient in a nursing home
(11,
12). Criteria for the syndrome of psychosis in Alzheimer’s disease have been proposed
(13), as the psychotic signs appear to represent a specific syndrome with longitudinal stability.
Emerging evidence indicates that psychosis and many other psychiatric and behavioral symptoms, in addition to the deficits in memory and other cognitive abilities, are fundamental expressions of the neurodegenerative illness. However, the specific etiologic factors and pathophysiologic mechanisms that are involved remain unclear. Neuropathological studies have revealed associations between delusional thoughts during the course of Alzheimer’s disease and density of neurofibrillary tangles, neuronal cell loss, or neurochemical abnormalities in specific cortical and subcortical regions at autopsy
(14–
17). In addition, neuroimaging assessments of regional cortical atrophy, ventricular enlargement, or white matter lesions using computed tomography or magnetic resonance imaging (MRI) suggest that focal structural abnormalities may be associated with the presence of psychosis in Alzheimer’s disease
(18–
21). More recently, neuroimaging techniques such as positron emission tomography (PET) and single photon emission computed tomography (SPECT) have been used to explore regional abnormalities of brain function associated with delusions in Alzheimer’s disease. A few studies have revealed associations between delusional thoughts in Alzheimer’s disease and function in a variety of brain regions: the temporal cortex
(22,
23), frontal regions
(24–
26), and other areas
(25,
27). Different methods among the studies probably account for the variable findings. The presence of delusions was often determined by retrospective caregiver observations over broad time spans, patients were characterized as either delusional or nondelusional, and functional activity was generally measured in relatively large cortical regions.
Discussion
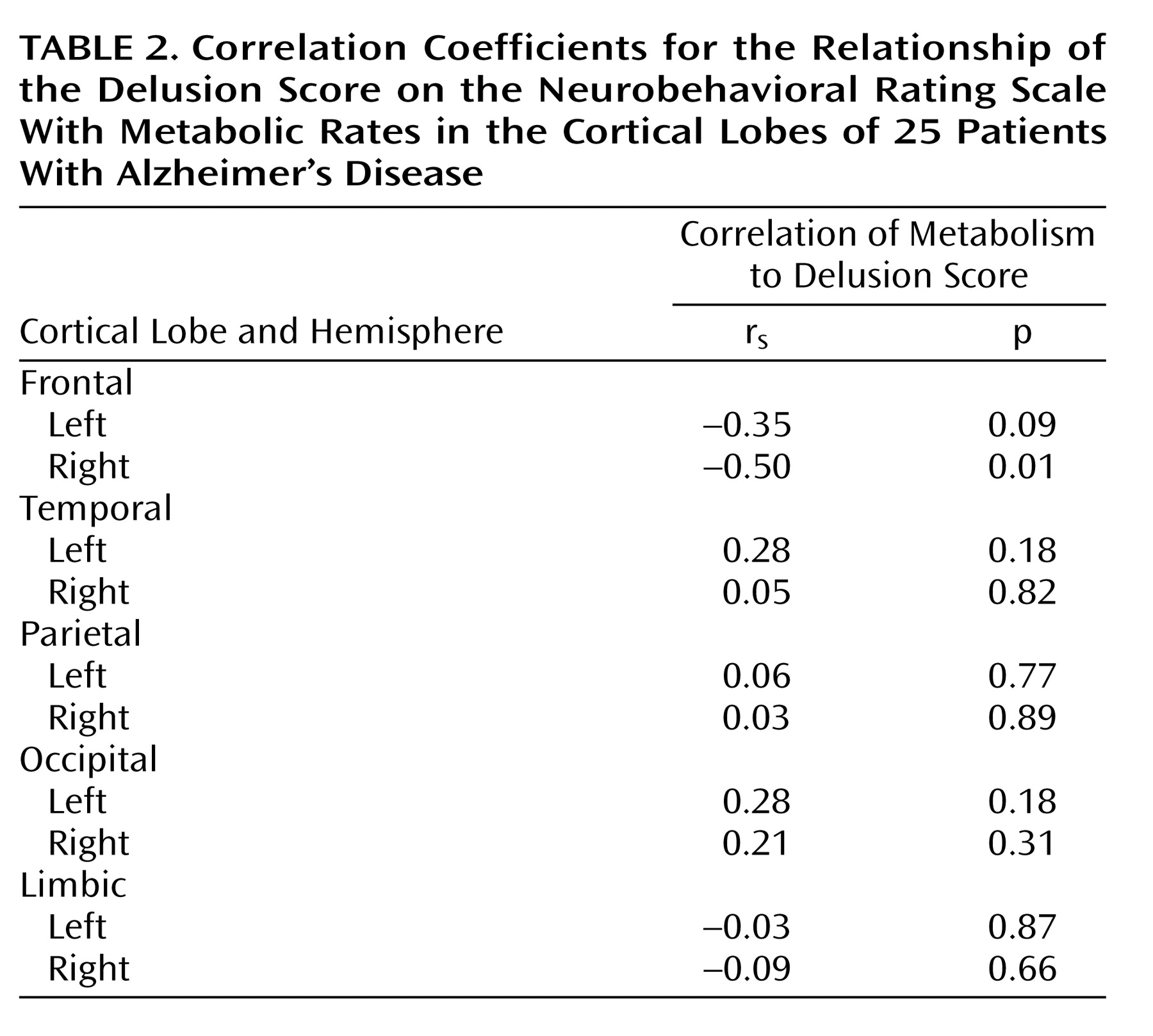
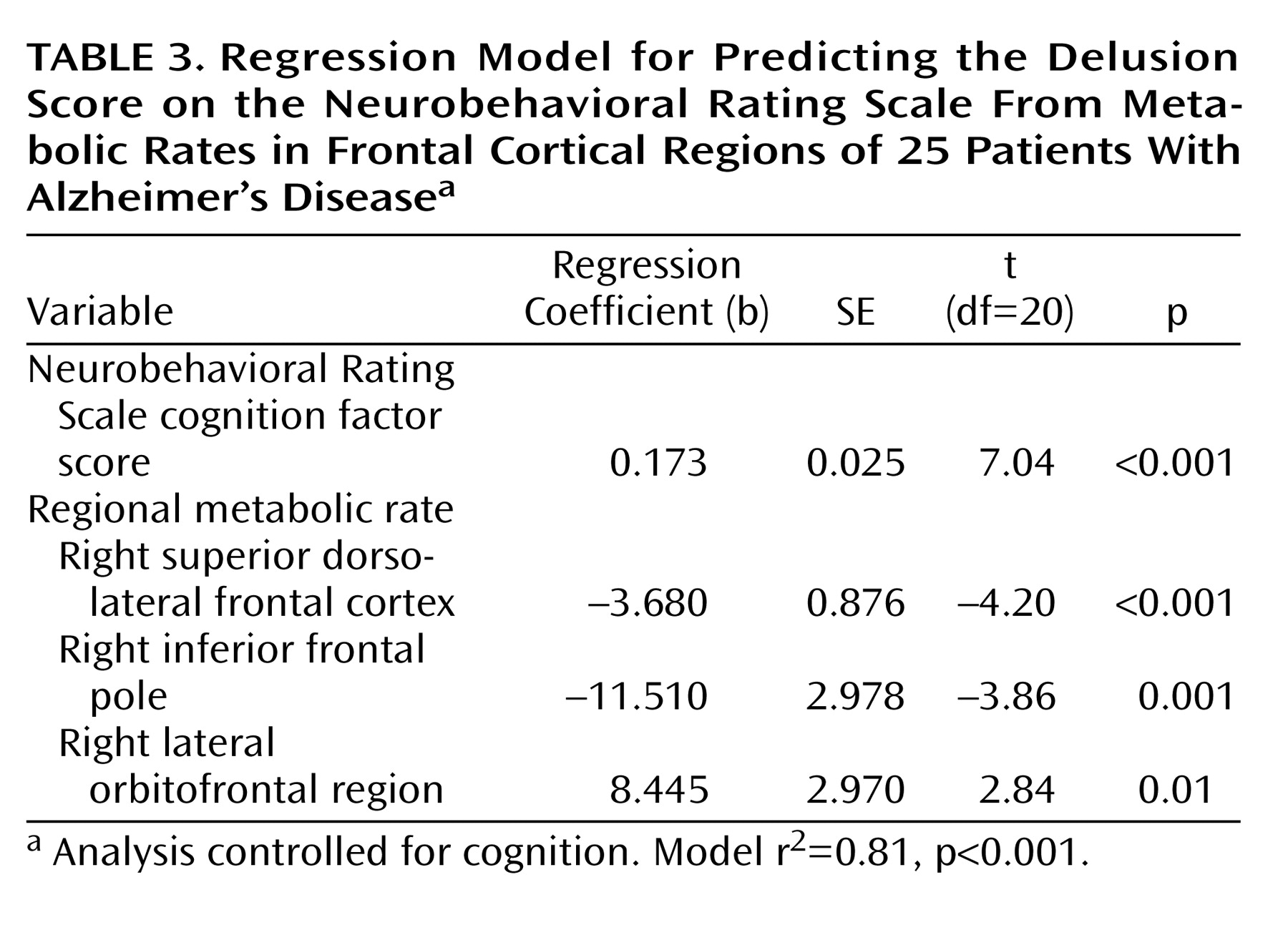
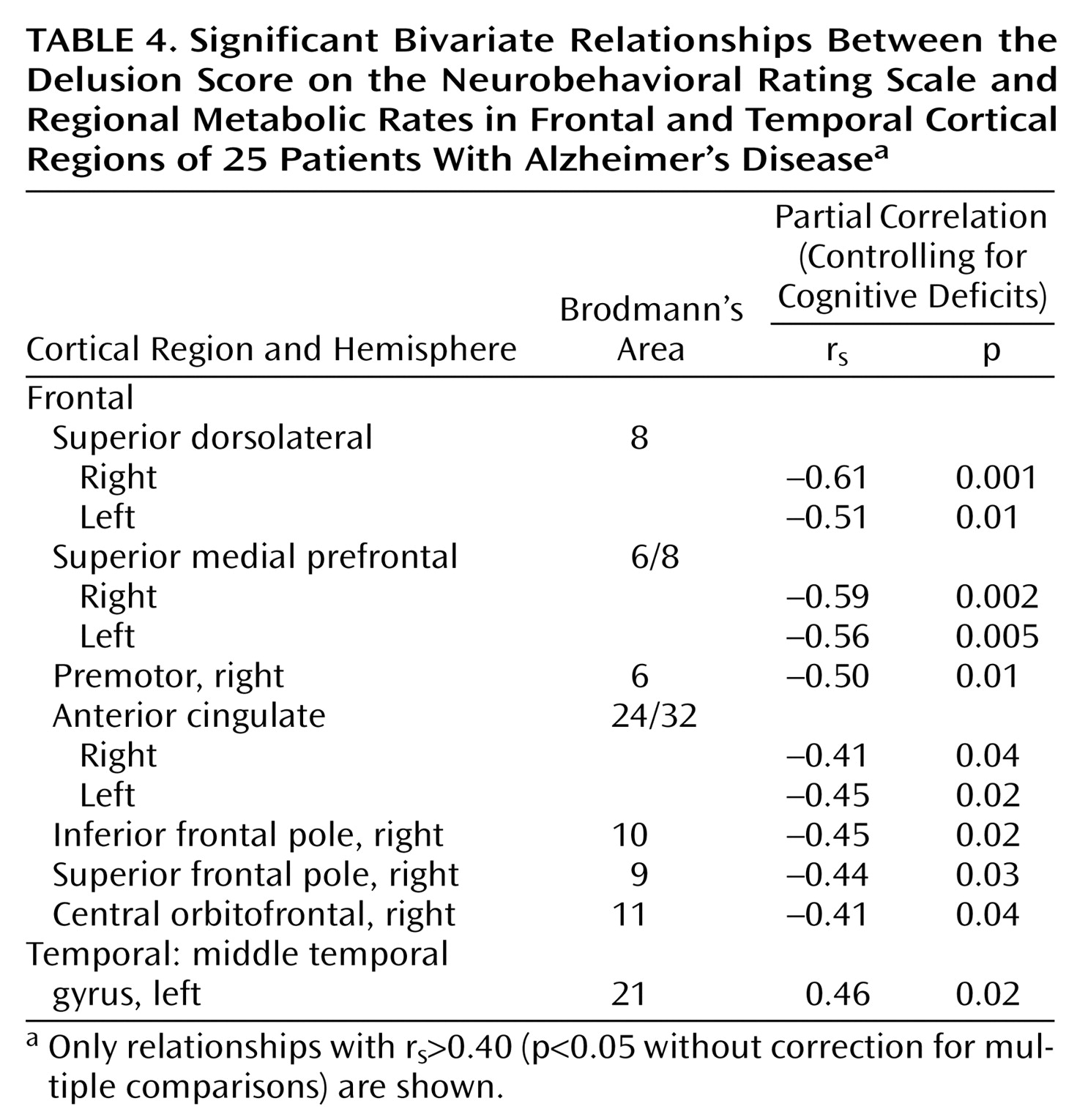
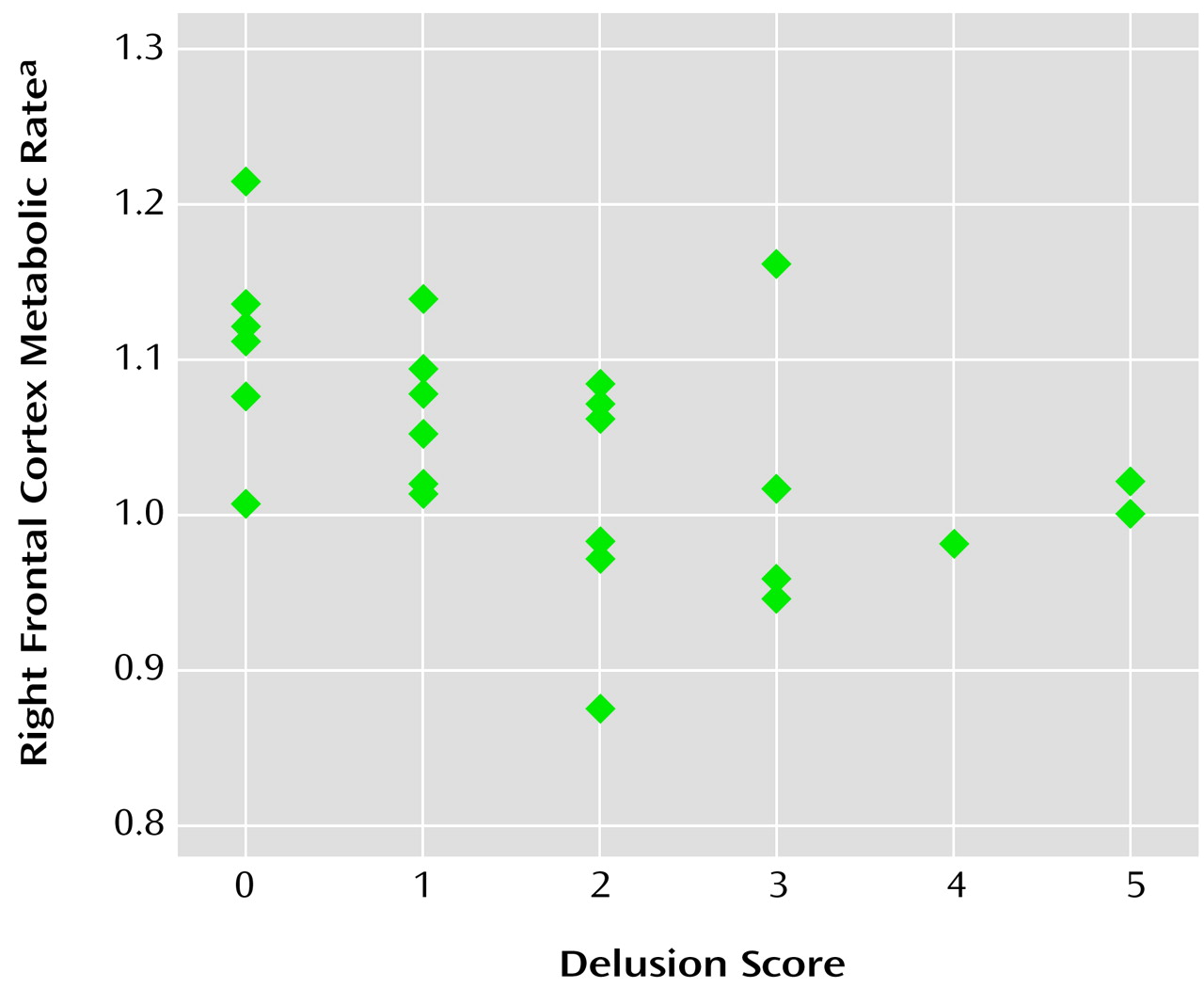
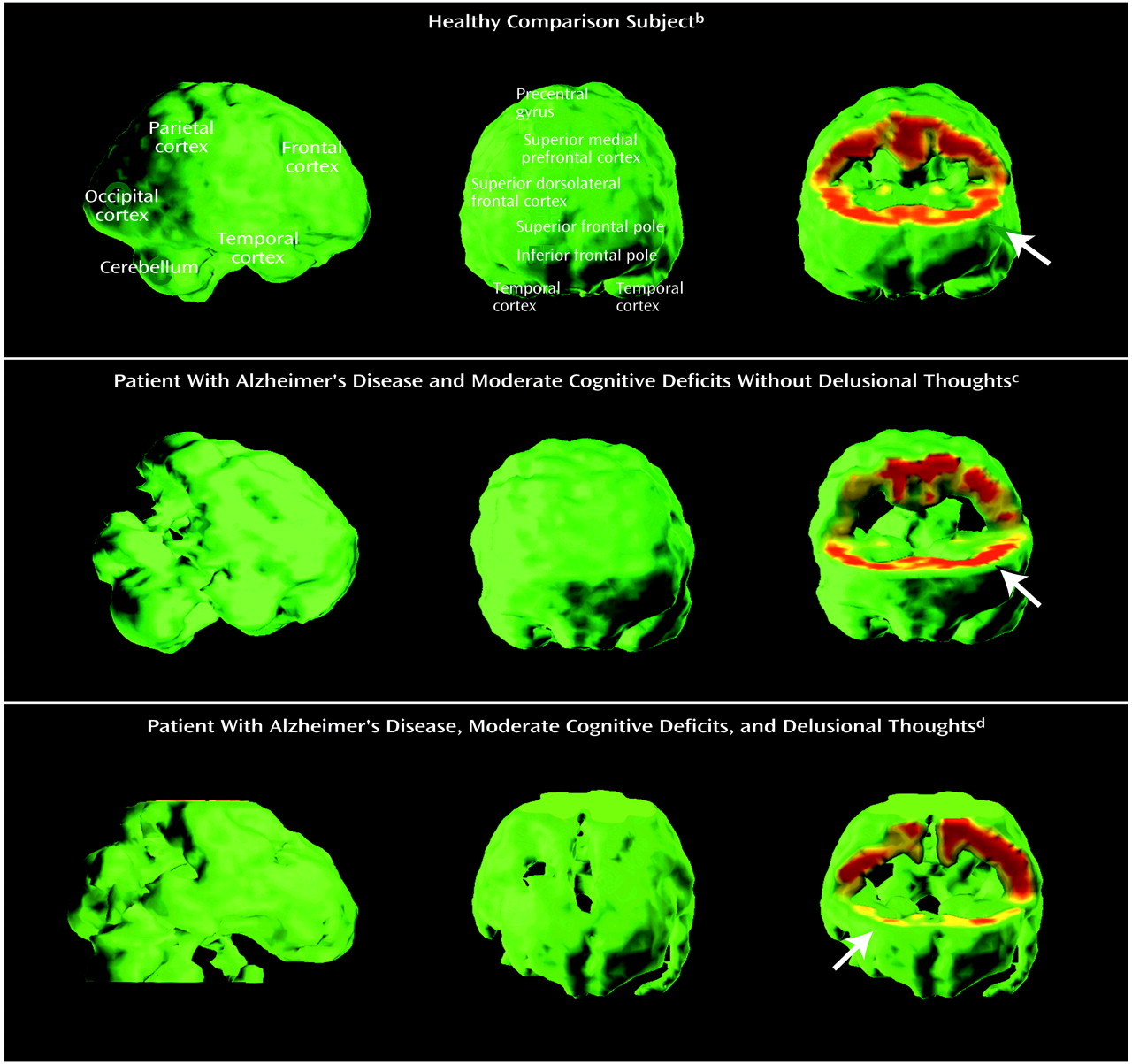
The results of this study indicate that hypometabolism in two regions of the right prefrontal cortex, the superior dorsolateral area (lateral aspect of Brodmann’s area 8) and inferior frontal pole (Brodmann’s area 10), are associated with delusional thoughts in patients with Alzheimer’s disease. The regression analysis also indicated that hypermetabolism in the lateral orbitofrontal region (Brodmann’s area 47) was independently associated with delusions, when we controlled for the metabolism in the other two regions. In bivariate correlation analyses, hypometabolism in additional right prefrontal regions, some homologous left prefrontal regions, and the bilateral anterior cingulate gyrus were also related to the severity of delusions, although this analysis was a consideration of each region individually rather than a simultaneous evaluation of all regions. Hypermetabolism in the left middle temporal gyrus was associated with delusions in the bivariate correlation analysis, but there were no other observed relationships between delusional thought and metabolic activity in the temporal lobe.
The results of a few previous PET and SPECT studies have suggested a relationship between delusional thought in Alzheimer’s disease and abnormal metabolism or perfusion in the frontal cortex. Early studies of global lobar function by Grady et al.
(40), Kotrla et al.
(41), and our group
(26) suggested frontal involvement. More recently, Mega and colleagues
(25) reported that patients with Alzheimer’s disease and delusions had lower perfusion in the bilateral dorsolateral prefrontal cortex and left anterior cingulate gyrus than did patients with Alzheimer’s disease without delusions. The highest peak z score on the statistical parametric map was near Brodmann’s area 6 in the right dorsolateral frontal cortex. Staff and colleagues found that hypoperfusion in the right prefrontal cortex was associated with the presence of content-specific delusions
(42) or any persistent delusion
(24). In an FDG-PET study, Mentis et al.
(27) demonstrated hypometabolism in orbitofrontal and anterior cingulate regions in Alzheimer’s disease patients with misidentification delusions. Lopez et al.
(43) examined two patients with Alzheimer’s disease and delusions and found left dorsolateral prefrontal hypoperfusion in both, with additional right frontal hypoperfusion in one. Three of these studies demonstrating relationships between frontal metabolism and delusions in Alzheimer’s disease also indicated that metabolism or perfusion of the temporal cortex
(27,
43) or other cortical or subcortical regions
(25,
27) contributes. Moreover, in studies by Hirono et al.
(22) and Starkstein et al.
(23), abnormal metabolism or perfusion in the temporal cortex was associated with delusions in Alzheimer’s disease, without evidence of frontal lobe involvement. However, temporal dysfunction is less consistently demonstrated across the reports. Both low and high metabolism or perfusion in the temporal lobe have been seen, and different subregions, either on the left or bilaterally, have been implicated.
The substantial heterogeneity of previous findings probably reflects large differences in patient groups, clinical assessment strategies, definition of delusions, medication status, neuroimaging procedures, clinical state at the time of functional neuroimaging, and image analysis techniques. Many investigators have examined only selected regions within lobes or have summed measurements of activity across large volumes. In the current study, the patient’s thought content was assessed near the time of the neuroimaging procedure, thus helping to establish a relationship between his or her neurophysiologic state and ongoing thought. Clinical assessments were performed by trained staff using a graded measure of delusion severity. No patient was taking psychotropic medication, and metabolism was measured in regions of interest that reflect known neurobiological boundaries in frontal and temporal regions.
The specific content of delusional thoughts, as well as their presence, may reflect functional activity in particular brain regions of a distributed network. The heterogeneity of the delusional thoughts present in this study and the limited number of subjects do not allow thorough analysis, and most reports of previous studies did not describe the nature of the delusional thoughts that were present. Studies by Hirono et al.
(22), Mentis et al.
(27), and Ponton et al.
(44) included many patients with paranoid delusions or misidentification delusions (e.g., spouse is an impostor, house is not one’s home) and showed associated abnormalities in the temporal cortex or orbitofrontal cortex. In contrast, the studies by Staff et al.
(24,
42) and the current study included some patients with predominant “factual” delusions that are less emotionally charged, e.g., delusions about current activities or fixed false beliefs regarding the environment (
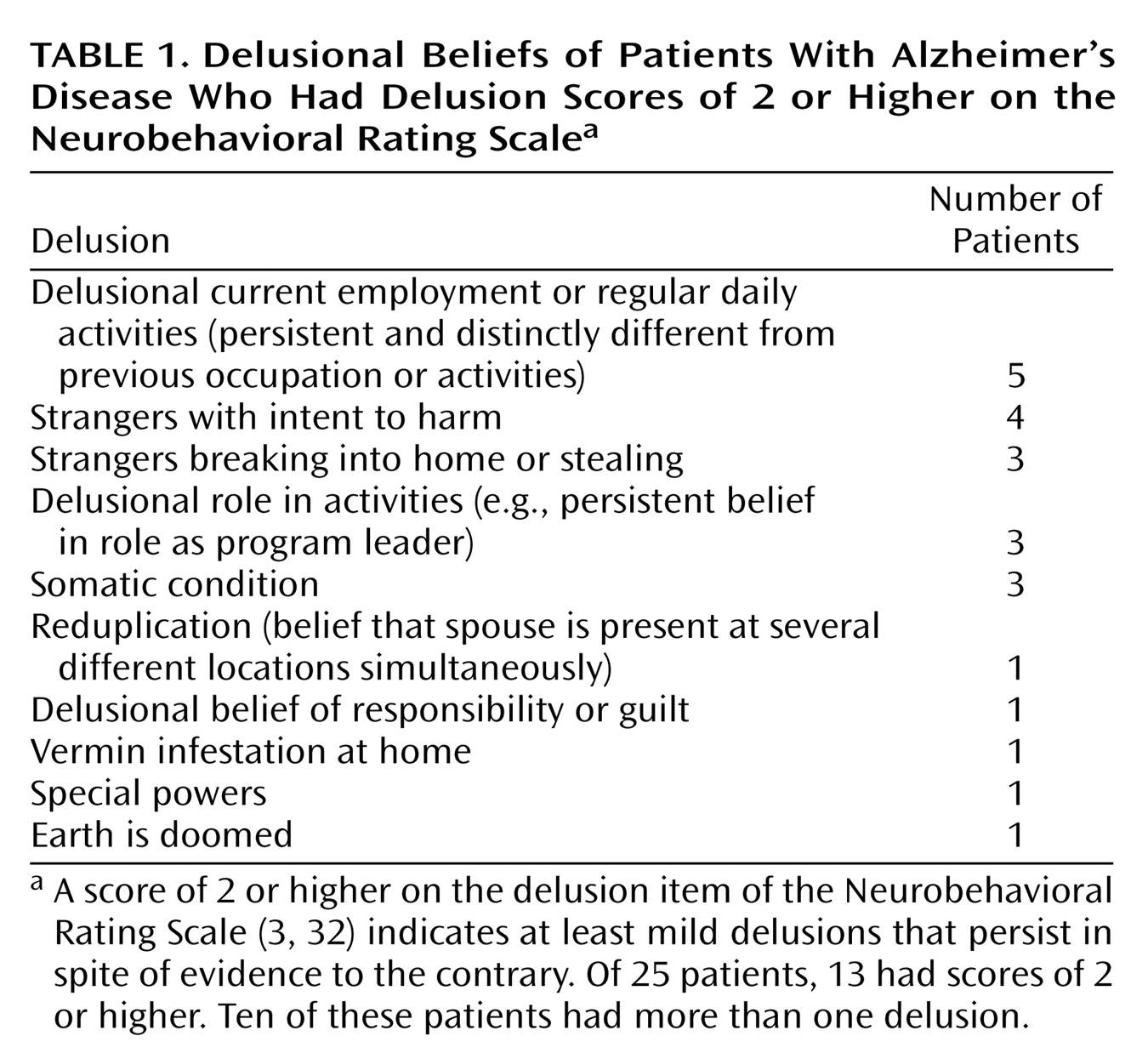
Table 1). These delusions had specific and persistent content and were firmly held in spite of information to the contrary, and thus they were considered delusions and not solely a reflection of inaccurate memory or poor insight. The relationships of delusions with frontal metabolism or perfusion were strongest in these studies. It is possible that temporal or orbitofrontal dysfunction contributes to delusions that involve fear or interpersonal relevance through limbic connections, whereas delusions of fact are linked to frontal dysfunction and errors of logic, monitoring, or mapping internal impressions to observations of the external environment.
Data from patients with psychosis due to neuropsychiatric disorders other than Alzheimer’s disease support a role for frontal dysfunction in the expression of delusional thoughts, although other brain regions may contribute. Studies of patients with frontotemporal dementia and psychosis
(45,
46) or those with schizophrenia
(28,
47,
48) have revealed abnormal frontal function, although the findings do not all agree. While a unitary neurophysiology of delusional thought is intriguing, additional data are needed, and disease-specific factors probably play an important role.
While activity in discrete brain regions has value in understanding the etiology of clinical symptoms such as delusions in Alzheimer’s disease, function across distributed networks that span neuroanatomic foci is probably more pathophysiologically relevant. Several neuronal circuits have been implicated across diagnostic groups. Cummings
(49) suggested that lesions in the temporal cortex or caudate nucleus may result in delusional thoughts by disrupting limbic functions that link perception to emotional states. Richardson and Malloy
(50) proposed that right hemisphere structures and the frontal cortex influence the development of content-specific delusions by disrupting self-corrective functions, and they suggested that temporal lobe lesions may also contribute through dysregulation of the experience of familiarity. Blackwood and colleagues, in a review of persecutory delusions from the perspective of cognitive neuroscience
(51), indicated that the medial and lateral inferior prefrontal cortex, anterior cingulate, and ventral striatum, as well as the temporal cortex, are involved in several cognitive processes that contribute to delusions: attentional bias, attributional bias, and deficits in the theory of mind. These findings are consistent with the idea that the role of frontal and temporal dysfunction in the development of delusions is mediated by a collaborative network. Although the neuropathology of Alzheimer’s disease is widespread, and distant abnormalities may be important, most patients have prominent structural
(52) and metabolic
(53) abnormalities in the temporal cortex. In this study, the mean absolute metabolic rate in the temporal cortex was 20% lower than the mean frontal metabolic rate across the Alzheimer’s disease patients, which indicates lower relative temporal cortex metabolism than occurs in elderly normal subjects
(54). Patients with hypometabolism in additional critical regions of the frontal cortex may develop delusions as a result of the loss of frontal systems that facilitate the monitoring of reality, compare internal experience with reality, link new experiences with memories of the past, or prevent consolidation of inaccurate beliefs. Such a hypothesis is supported by the finding that the density of neurofibrillary tangles in neocortical regions, including the midfrontal gyrus, but not the hippocampus or entorhinal cortex, is associated with delusions in Alzheimer’s disease
(15).
There are several aspects of this study that must be considered carefully in interpreting the results. First, we focused on the metabolic rate in defined regions of the frontal and temporal lobes, on the basis of previous findings. We thus cannot exclude associations between severity of delusions and metabolic activity elsewhere in the brain, although no lobar effects were found. Also, the limited number of subjects prohibits a definitive analysis of the potential simultaneous impact of many regional metabolic rates on the Neurobehavioral Rating Scale delusion score. Moreover, the associations with specific frontal regions that emerged in the regression model are sensitive to chance fluctuations given the number of subjects, as well as potential intercorrelations among metabolic rates, and thus may not be replicable. However, the significance of associations with individual frontal regions was confirmed in the resampling model. Second, whether regional metabolic rate is a cause or an effect of delusional thoughts in Alzheimer’s disease could not be determined in this study. Third, the observed regional metabolic rates may be due to anatomically distant, rather than local, structural lesions
(55). Thus, we cannot exclude an etiologic role for distant cortical neuropathologic events that are reflected in local regional metabolic rates. In addition, the regional metabolic rates were not corrected for atrophy, and thus regional hypometabolism in this study may at least partly reflect regional brain atrophy. Fourth, it is possible that neuropsychiatric symptoms other than delusions may contribute to the observed relationships with regional metabolic rates. However, the analyses controlled for the effects of cognitive impairment, and other psychiatric symptoms, including anxiety, depression, and behavioral retardation, were not associated with severity of delusions. Delusions were associated with the extent of agitated behavior, although these two constructs are not entirely independent and strict control for behavioral consequences of delusional thoughts in the analysis needs to be considered cautiously. Nonetheless, when the Neurobehavioral Rating Scale agitation factor score was included in the regression model, the significant relationship between the delusion score and hypometabolism in the right superior dorsolateral cortex persisted, but the relationships with the other two frontal regions were not clearly independent of the effect of agitated behavior.
The results of this study indicate that hypometabolism in specific regions of the right prefrontal cortex may be involved in the expression of delusions in Alzheimer’s disease. Functional interactions across broader neuronal networks are likely to be important. These findings contribute a neurobiological framework for a specific syndrome of psychosis in Alzheimer’s disease
(13) that appears to be longitudinally consistent
(7,
56). Other factors, which may or may not be linked to regional neuroanatomic effects, also may be important. Such factors include genotype, neurochemical abnormalities, cultural background, previous personal experience, psychological state, and effects specific to particular delusional thoughts. Better understanding of the relationships between regional brain function and clinical symptoms in Alzheimer’s disease can help to refine the syndromal concept of psychosis in Alzheimer’s disease and to predict longitudinal stability of symptoms and response to therapeutic intervention.