It has been suggested that schizophrenic patients are protected against cancer in general and against lung cancer in particular, despite the fact that these patients tend to be heavy smokers
(1,
2). The basis for this suggestion is a number of reports of reduced mortality from cancer
(2–
6) and more recent reports of a lower incidence of cancer among schizophrenics than in the general population
(7–
10). Various biological explanations have been proposed to explain a possible dissociation between the two diseases
(11–
13). For example, the lower cancer risk may be due to an antitumor effect of phenothiazines
(14,
15), to which schizophrenic patients are often exposed for long periods. Alternatively, the existence of a specific factor of etiological significance for both schizophrenia and tumor resistance has been proposed. One such mechanism might be apoptosis (programmed cell death), and it has been suggested that genetic predisposition to increased apoptosis due to alterations in the
P53 gene could cause schizophrenia by interfering with the normal pattern of brain development and could also explain the reduced rates of cancer in persons with schizophrenia
(13).
Method
Study Population
Since 1968, all residents of Denmark have been recorded in the Civil Registration System and assigned a unique personal registration number that contains their date of birth and sex. Individual information is kept under this identification number in all national registries, ensuring accurate linkage of information between registries. This registration system also includes identifiable information on parents and offspring as well as information on date of birth, sex, place of birth, and continuously updated information on vital status.
We extracted data for all 5,088,795 persons born on Jan. 1, 1935, or later who were living in Denmark on April 1, 1968, or born between that date and Dec. 31, 1999. Additionally, 743,151 persons born before 1935 were identified by linkage to their children born after 1935; thus, all of these were parents, yielding a database of 5,831,946 persons. We then excluded 522 persons whose vital status was unknown and 703,239 persons born outside Denmark, leaving 5,128,666 persons.
From these, we extracted 2,831,589 who were registered as parents. Furthermore, only parents whose children were over age 15 at the termination of follow-up on Dec. 31, 1997, were included based on the assumption that less than 1.5% of schizophrenia cases develop before age 15
(17). Thus, the cohort of parents consisted of 2,015,965 individuals who were all born in Denmark and were alive on April 1, 1969 (from which date information on psychiatric hospitalization is available), and who had children born after Jan. 1, 1935, and before Jan. 1, 1983.
Identification of Parents and Offspring With Schizophrenia
Members of the parent cohort and their offspring were linked to the files of the Psychiatric Case Register, which is a national database that has been computerized since April 1, 1969, and contains data on all admissions to Danish psychiatric inpatient facilities and information from outpatient contacts since 1995
(18). There is no fee for psychiatric treatment in Denmark, and no private facilities exist. The diagnostic system used during the study period was the ICD-8 up until 1993 and the ICD-10 thereafter. Persons with any hospitalization with schizophrenia were identified under ICD-8 code 295 and ICD-10 codes F20 and F25. A total of 6,676 parents (0.3%) had been admitted for schizophrenia and were excluded from the parent database, leaving a total of 2,009,289 parents. In all, 19,856 parents (1%) had one or more offspring with a diagnosis of schizophrenia.
Identification of Cancer Cases
Parents in the cohort in whom a cancer had been diagnosed were identified by linkage to the files of the Danish Cancer Registry. Since 1943, the registry has collected information on all individuals in Denmark with cancer, including benign brain tumors and urinary bladder papillomas
(19). The registration is based on notification forms that are completed by hospital departments and practicing physicians whenever a case of cancer is diagnosed or found at autopsy and whenever there are changes in an initial diagnosis. The cases recorded manually are supplemented by unrecorded cases revealed by the computerized linkages to the death certificate files and the National Registry of Patients
(20). Ambiguous or contradictory information, either within a notification form or between forms, leads to queries in approximately 10% of the notifications received. Comprehensive evaluation has shown that the registry is 95% to 99% complete and valid
(19,
21–23). The cancers are classified according to the modified Danish version of the ICD-7. A diagnosis of cancer (other than nonmelanoma skin cancer) before the birth of the parents’ oldest child led to exclusion of 10,217 parents (0.5%), leaving 1,999,072 parents for analysis.
Data Analyses
Individual follow-up of the parents was begun on the date of birth of their oldest child or April 1, 1969, whichever came last, and ended on the date on which a cancer other than nonmelanoma skin cancer was diagnosed (N=186,231, 9.3%), death occurred (N=185,312, 9.3%), the person emigrated (N=23,007, 1.2%), the person disappeared (N=355, <0.02%), or on Dec. 31, 1997 (N=1,604,167, 80.2%).
Poisson regression models were used to estimate the possible effect of schizophrenia in a child on the cancer risk of the parents. The analyses were performed with the SAS GENMOD procedure. Ratios of incidence rates were used as a measure of relative risk. The p values were based on two-tailed likelihood ratio tests, and 95% confidence intervals (CIs) were calculated from the maximum likelihood estimates.
Separate analyses were made for men and women, and adjustment was made in all analyses for age, calendar period (in 5-year categories), and number of children. The latter covariate was included both for its relevance in breast cancer analysis but also because of the increased probability of having a child diagnosed with schizophrenia with an increasing number of children. We tested the influence of having a child with schizophrenia both as an ever/never variable, with the exposure date defined as the date of the birth of the child, and as a time-dependent variable, with the exposure date defined as the date of the first diagnosis of schizophrenia in an offspring. The choice of following up from the time of birth of the oldest child was based on the hypothesis that some genetic factor might be responsible for a different cancer risk in schizophrenics and thereby also in their first-degree relatives, which would imply that the first-degree relative can be considered to be exposed throughout life. The time-dependent approach, however, reflected the cancer risk after a child has received a diagnosis of schizophrenia. Also, as most of the earlier findings of reduced risks in schizophrenic patients have been made in male patients
(7–
10), we stratified the analyses by the sex of the offspring into fathers or mothers of sons only, daughters only, or both sexes.
Relative risks were calculated for all types of cancer combined, for tobacco-related cancers combined (cancer of the buccal cavity, esophagus, pancreas, larynx, lung, kidney, and urinary bladder
[24]), and for a number of site-specific cancers. For all categorical variables, the category with the largest number of cases was chosen as the reference.
Results
Follow-up of the cohort of 1,999,072 parents yielded a total of 48,343,430 person-years at risk.
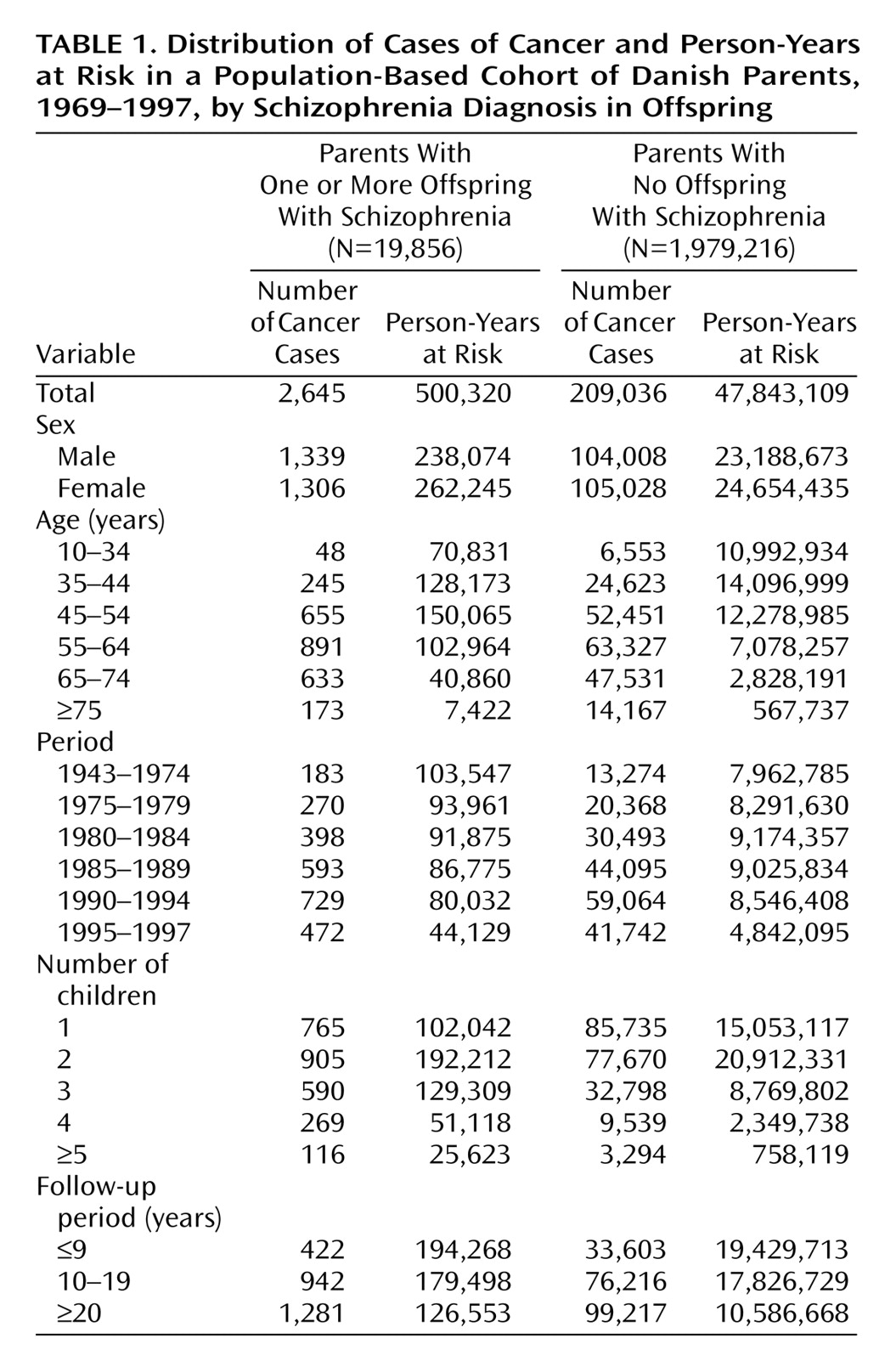
Table 1 shows the distribution of person-years at risk by selected descriptive variables for the group of 19,856 parents with schizophrenic offspring (exposed) and the 1,979,216 parents with no schizophrenic offspring (unexposed). The mean follow-up was 25.3 years (SD=5.6) for the women with one or more schizophrenic children and 24.1 years (SD=5.6) for the women with no schizophrenic offspring. The corresponding mean follow-up time for men was 24.0 years (SD=6.5) and 23.2 years (SD=6.1), respectively. The mean age at the time of the first birth was no different in the two groups of mothers—24.7 years (SD=5.6) for the women with schizophrenic offspring and 24.7 years (SD=5.4) for the women with no schizophrenic offspring—whereas the fathers of schizophrenic offspring were slightly older at the time of the birth of their first child compared to the fathers with no schizophrenic offspring (mean age=28.3 years, SD=6.8, versus mean age=27.9, SD=6.4, respectively). Among the parents with schizophrenic offspring, 18% had one child, 37% had two children, and 45% had three or more children, whereas the corresponding proportions were 26%, 44%, and 30% among the parents with no schizophrenic offspring.
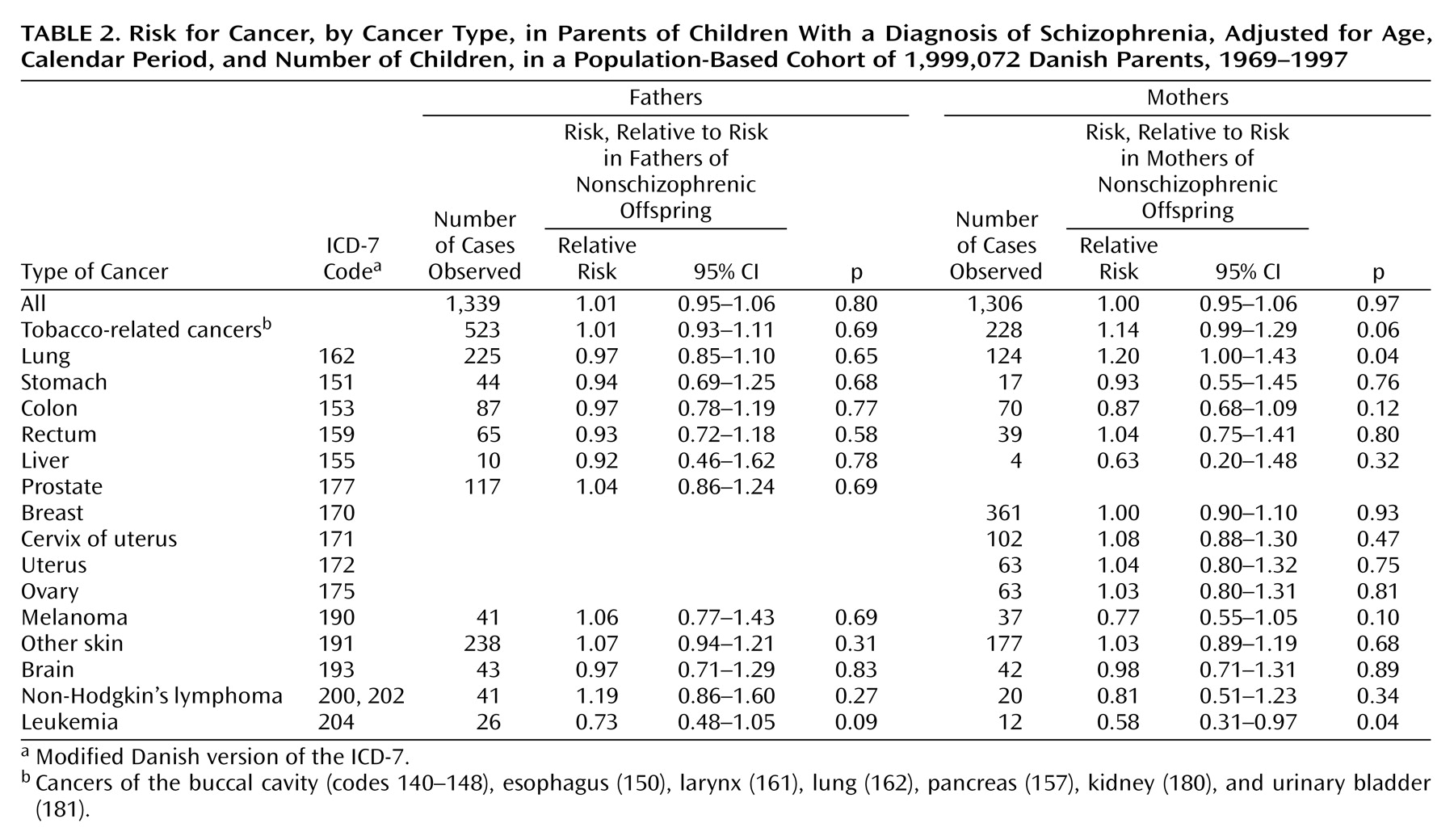
A total of 2,645 cases of cancer of all types were diagnosed among the parents of the patients with schizophrenia, whereas 209,036 cancers were diagnosed among the parents without schizophrenic offspring (
Table 1), corresponding to an adjusted relative risk for all cancers of 1.01 for fathers (based on 1,339 cases) and 1.00 for mothers (based on 1,306 cases) (
Table 2). The results were no different when exposure was applied as a time-dependent variable, with adjusted relative risks of 1.00 (95% CI=0.92–1.07, p=0.92) for the fathers and 0.97 (95% CI=0.89–1.05, p=0.43) for the mothers (data not shown).
We observed an increased risk of 1.20 for lung cancer and a similar increase of 1.14, albeit not significant, in the risk for tobacco-related cancers combined in the mothers of schizophrenic children, whereas the risks of the fathers for both tobacco-related cancers combined and lung cancer were close to unity. The mothers of schizophrenic children had a decreased risk for leukemia (relative risk=0.58), with a similar reduction in fathers although not significantly so (relative risk=0.73). The results were essentially no different when the time-dependent exposure status was applied (data not shown). In general, there was no difference when the analyses were stratified by the sex of the offspring, although the increased risk for lung cancer appeared to be confined to the mothers of schizophrenic sons or of both sons and daughters (of which at least one was schizophrenic) (relative risk=1.41, 95% CI=0.97–1.97, p=0.05, and relative risk=1.24, 95% CI=0.88–1.70, p=0.17, respectively). The mothers of schizophrenic girls only had no increased risk for lung cancer (relative risk=0.97, 95% CI=0.54–1.57, p=0.90) (data not shown).
Discussion
No difference in risk for cancer was found among the parents of schizophrenic children when compared with the parents of children without schizophrenia in this large population-based cohort covering all of Denmark. The only findings were of increased risk for lung cancer in mothers and a tendency to a decrease in risk for leukemia in both mothers and fathers of schizophrenic children.
This study took advantage of the virtually complete population-based registries in Denmark, which contain uniform, identifiable, continuously updated information on births, psychiatric hospitalizations, cancer development, and vital status. The strengths of this database are that all exposures are recorded independently of the outcome and that reporting is mandatory throughout the country. Therefore, this study can be considered free of the influence of recall bias. The classification and registration of schizophrenia in the Psychiatric Case Register was assumed to be comparable throughout the study period, although the ICD-8 was used to classify diagnoses from 1969 to 1994 and the ICD-10 from 1994 forward. There have been no reported differences in basic epidemiological characteristics, such as sex, age, family history, and urbanization, of schizophrenics diagnosed in Denmark in the two different periods
(25,
26). With regard to cancer registration, the same classification system, a revised version of the ICD-7, was implemented throughout the full period, and the registry is considered highly valid
(19,
21–23).
Moreover, the population-based nature of the material, in combination with the cohort design, minimizes the effect of selection bias. The inclusion of outpatient information was only possible from 1995 to 1997, but within the data set, there was insufficient power to examine parents of outpatients versus parents of inpatients separately. The decision of whether a patient should be referred to in- or outpatient treatment, however, does not rely on factors relevant to cancer risk in the Danish health system, leaving possible bias due to such selection minimal. Some degree of misclassification of exposure might have been present because we categorized parents as exposed from the time of the birth of their child with schizophrenia on the basis of the assumption that a familial association with cancer risk would manifest throughout the life of a first-degree relative. Some of the offspring would probably not have survived long enough for schizophrenia to be diagnosed, and their parents would have been categorized as unexposed throughout the follow-up. This misclassification would probably result in a bias toward the null hypothesis.
The only other study, to our knowledge, of the risk for cancer in first-degree relatives of schizophrenic patients was a population-based study in Finland of some 53,000 siblings and 40,000 parents of 27,000 schizophrenic patients
(16). The authors reported a reduced incidence of all cancers in both parents and siblings as well as in cancer of the lung, breast, and uterus in mothers, colon cancer in both mothers and fathers, and a nonsignificantly reduced risk of prostate cancer in fathers when compared with the rate of cancer in the general Finnish population
(16).
We did not find a similar pattern of cancer risk in the present study; several differences in design between the two studies apply that could possibly account for the discrepant results. First, we were able to follow up for cancer at an individual level and thus to compare the parents of schizophrenic patients with those of nonschizophrenic children. We chose this comparison group on the basis of the assumption that it is more suitable than the background population because only parents are at risk of having a child with schizophrenia and, furthermore, parents may resemble each other in some important respects. Second, we compared only the rates of first primary cancers, so that the risk estimates excluded an effect of persons with a previous diagnosis of cancer who might be at increased risk for cancer owing to the late effects of treatment and shared risk factors. We explored the apparently disparate results further by calculating standardized incidence rates and corresponding 95% confidence intervals based on the national age-, sex-, and calendar-period-specific incidence rates of cancer, thus paralleling the method used by the Finnish researchers. The results of this method applied on the Danish data showed remarkable similarities to the Finnish results. The risk for overall cancer was reduced significantly in both fathers (standardized incidence rate=0.90, 95% CI=0.85–0.95) and mothers (standardized incidence rate=0.91, 95% CI=0.86–0.96), thus paralleling the Finnish findings of standardized incidence rates of 0.93 (95% CI=0.90–0.96) and 0.89 (95% CI=0.86–0.92) in fathers and mothers, respectively. When considering the site-specific risks, our results were generally in line with the Finnish data demonstrating a comparable reduced risk for the cancer sites mentioned (lung, breast, uterus, colon, and prostate). This tendency to a reduction of cancer risk in the parents of schizophrenic offspring in comparison with the general population that is not apparent when in comparison to other parents we attribute to a positive effect of being a parent on cancer risk rather than to being a first-degree relative of a schizophrenic patient. This effect has been observed in cancer epidemiological studies in which the parents of children with cancer were found to have a tendency for a reduced risk for total cancer and several specific cancer forms, e.g., lung cancer as well as a reduced mortality for, for example, myocardial infarct and myocardial arteriosclerosis, in comparison to the background population, which is suggestive of a “healthy parenthood effect”
(27,
28). The healthy parenthood effect is here used as the denotation of the selective processes that lead to both the formation and maintenance of a family life. It is probable that parents have a relatively healthier and more regular life style than the general population
(27,
28).
In the present analysis, we have not included information on cancer risk in the siblings of schizophrenic patients. Only siblings born after 1935 could be included, and because of their low mean age and thus their low baseline risk for cancer, this would compromise the statistical power.
The hypothesis of a decreased risk for cancer among first-degree relatives of patients with schizophrenia derives from several observations of a reduced cancer risk among schizophrenics
(7–
10), which might be explained by a genetically determined reduced susceptibility to cancer. However, the findings for cancer risk among schizophrenics were also different in the Danish and Finnish studies. In the Danish patients, a reduced risk for all cancers was observed among males
(9), which was attributable to reduced risks for cancers of the testis and skin (including malignant melanoma), and cancers of the prostate, colon, rectum, and lung also occurred at notably low rates
(9). Among Finnish schizophrenics, the risk for rectal cancer was reduced, but the risks for cancers of the lung, pharynx, gall bladder, and uterus were increased
(16). Both the Danish and Finnish cohorts were relatively young: the Danish cohort comprised all schizophrenic patients first admitted in 1970–1987, and the Finnish patients were all born after 1940. In a new Danish study that included all patients admitted with schizophrenia between 1969 and 1993 and followed up through 1995, the risk for all smoking-related cancers combined was lower in male schizophrenics and the risk for lung cancer was nearly significantly reduced (standardized incidence rate=0.82, 95% CI=0.65–1.02) (S.O. Dalton, doctoral thesis, Copenhagen University, 2002). However, further analysis of this finding indicated that the apparent protection against lung cancer in these patients applied mainly to older patients, who probably smoked less than younger patients and less than the general population. The findings of an increased risk for lung cancer in the younger schizophrenics in the later periods of the study of the Danish cohort (S.O. Dalton, 2002) might correspond to the Finnish findings of an increased risk of lung cancer in the relatively young Finnish cohort
(16), although we could not make comparisons by age group or period. The increased risk for cancer among Finnish schizophrenics and the decreased risk in their first-degree relatives were interpreted as reduced cancer susceptibility, overridden by the augmented risk behavior of persons with schizophrenia. The findings of our study do not support the theory of a genetic risk factor for both vulnerability to schizophrenia and low cancer risk, expressed as a reduced risk for cancer in the parents. In fact, the parents appeared to have no consistently different pattern of cancer risk from other parents.
The risk for leukemia seemed to be decreased in both the mothers and fathers of schizophrenic children. The risk for this type of cancer was not found reduced in previous Danish studies
(7–
9) or, to our knowledge, in any other study of cancer risk in schizophrenics
(10,
16,
29,
30). The risk for leukemia was not evaluated in the Finnish study of first-degree relatives
(16). Because a large number of analyses were performed, interpretation of this unexpected finding must be cautious.
The finding of increased risks for lung cancer and for tobacco-related cancers combined in the mothers of schizophrenic patients may probably be explained by a greater frequency of smoking. An association between low birth weight and risk for schizophrenia has been found consistently in epidemiological studies
(31–
33), and heavy smoking by mothers during pregnancy may be suggested as an explanation for this association. Another hypothesis suggests that a low prenatal vitamin D concentration is a risk factor for schizophrenia
(34). The mothers of schizophrenic patients in the present study showed no reduction in risk for malignant melanoma or nonmelanoma skin cancer, and although this can only be considered an overall measure of accumulated exposure to ultraviolet radiation, it indirectly weakens this hypothesis.
In conclusion, we were not able to replicate the previous findings of a reduced risk in parents to schizophrenic offspring and ascribe this discrepancy to methodological reasons. This large population-based study did not show a reduced risk for cancer among the parents of schizophrenic patients and therefore offers no support for the hypothesis of a genetically determined reduced risk for cancer in schizophrenic patients.