Relapse is a significant problem for individuals with eating disorders, with rates of relapse ranging from 22% to 51% across outcome studies of anorexia nervosa and bulimia nervosa
(1–
5). The identification of predictors of postremission relapse could reveal key targets for the prevention of future episodes of illness
(6). Studies of bulimia nervosa have identified a number of posttreatment predictors of relapse
(7–
10). Many of these, such as higher frequencies of vomiting
(7), higher dietary restraint
(8), greater dissatisfaction with body image
(9), and the overimportance of weight and shape
(10), could be characterized as residual symptoms of an eating disorder resulting from a failure to fully respond to treatment. In contrast, studies of anorexia nervosa have provided few posttreatment predictors of relapse
(5), with most studies reporting on the predictive significance of intake variables
(4,
11).
A limitation of previous work on the relapse of eating disorders is the time course used in most treatment outcome studies. These investigations typically have conducted assessments at intake, during treatment, at the end of treatment, and then at a single follow-up. Thus, for several studies, relapse was captured only for individuals who recovered by the end of treatment and who were ill at follow-up. This timeline does not capture events that may occur in the interim, and, for captured events, it provides little to no information concerning how individuals fared between recovery and relapse. Thus, many of these studies do not identify targets for relapse prevention that are distinct from the original targets of treatment.
Method
Definitions
In line with previous work
(6,
13,
14), we used the MacArthur guidelines to define remission and relapse. The Psychiatric Status Rating Scale
(15) was used to denote the level of symptoms according to DSM-III-R criteria. Scores of 5 or 6 indicate a person who meets the full criteria. All participants had scores of 5 or 6 for either anorexia nervosa or bulimia nervosa at study entry. Remission was defined as having a period of 8 consecutive weeks in which no or minimal symptoms of the syndrome were present (Psychiatric Status Rating Scale score of 1 or 2), consistent with the MacArthur guidelines for depression. Relapse represented a return to full syndromal criteria after a period of remission for either anorexia nervosa or bulimia nervosa (Psychiatric Status Rating Scale score of 5 or 6).
Participants
Most participants were women seeking treatment for an eating disorder at the Massachusetts General Hospital Eating Disorders Unit and at other Boston-area eating disorder programs between October 1987 and June 1990. An additional cohort of 21 women who met DSM-III-R criteria for anorexia nervosa was recruited in 1991. The inclusion criteria for participation in the study were 1) a DSM-III-R diagnosis of anorexia nervosa or bulimia nervosa, 2) being female, 3) a minimum age of 12 years, 4) residence within 200 miles of Boston, 5) English speaking, and 6) no evidence of organic brain syndrome or terminal illness. Of the 294 women who met participation criteria, 250 (85%) agreed to participate in the longitudinal study. Four subjects dropped out of the study after their intake interview and before the first follow-up interview. Thus, the total size of the study group was 246. After complete description of the study to the subjects, written informed consent was obtained.
When we retrospectively applied DSM-IV criteria to intake data, 136 (55%) of these women met DSM-IV criteria for anorexia nervosa at intake, and 110 (45%) met DSM-IV criteria for bulimia nervosa at intake. Most participants (N=235, 96%) received some form of treatment during follow-up, and a portion (N=90, 37%) received inpatient treatment. At the last follow-up, 229 (93%) subjects had been retained in the study group. Detailed demographic data for the full group have been presented elsewhere
(16).
As reported previously
(12), the rates of remission were significantly higher in the patients with bulimia nervosa than in those with anorexia nervosa. Over the course of follow-up, 83 women with intake diagnoses of bulimia nervosa (75%) achieved remission, and 42 women with intake diagnoses of anorexia nervosa (31%) achieved remission.
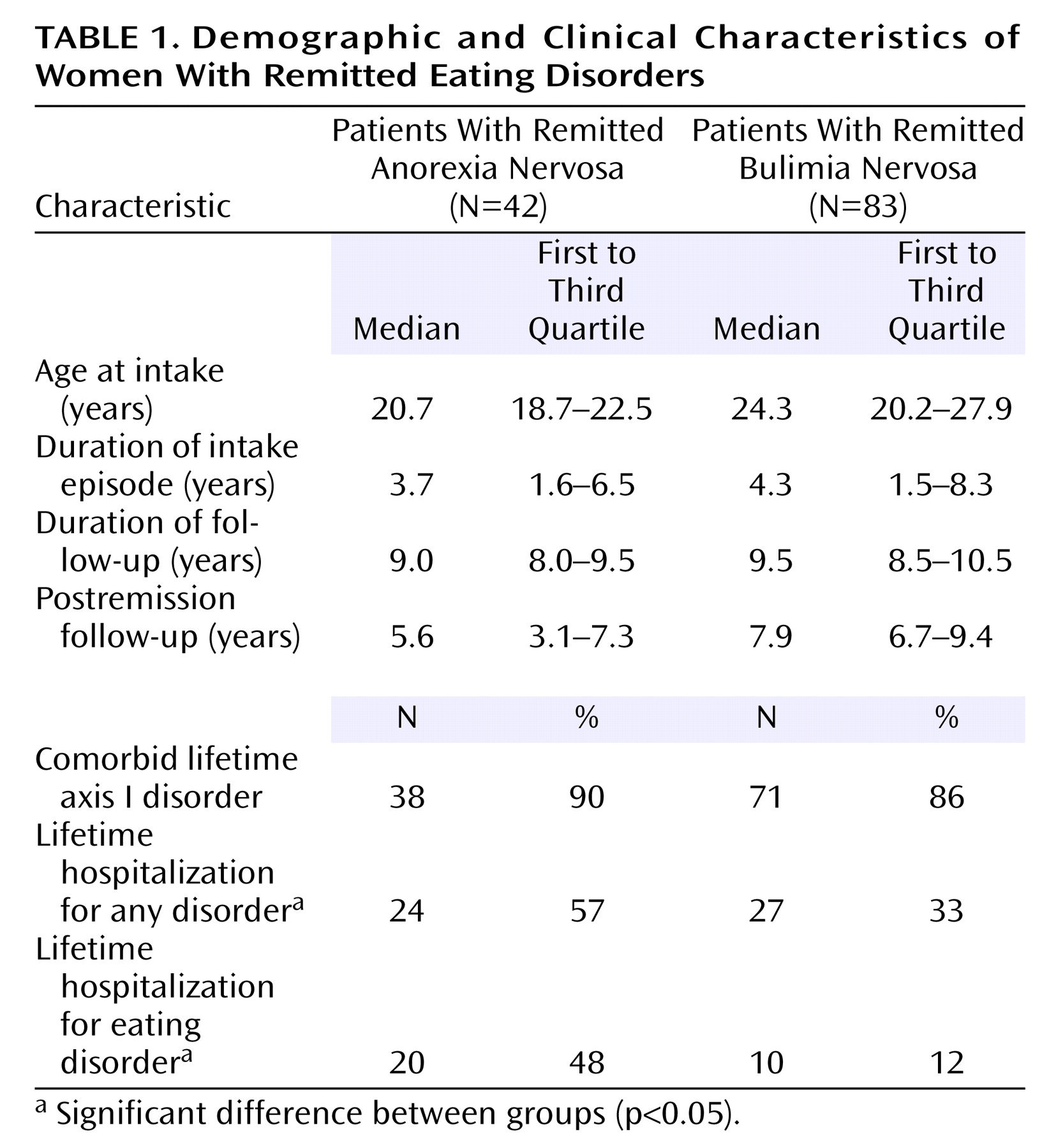
Table 1 provides data regarding age, duration of follow-up, and clinical characteristics for the remitted groups. The patients who recovered from anorexia nervosa had higher weights and shorter durations of illness at intake than those who did not recover
(12). No differences were found between the patients who recovered from bulimia nervosa and those who did not
(12).
Procedure
The individuals who appeared to meet study inclusion criteria were scheduled for an interview that was conducted in person by a trained research assistant. Interviewers confirmed the presence of full-syndrome eating disorders and assessed current and lifetime psychiatric disorders. Objective measures of height and weight were obtained during this intake interview. Follow-up interviews were conducted every 6 months during the first 5 years of the study and then were conducted annually during the remaining years of the study and thus required retrospective recall of the previous 6 months to 1 year. Follow-up interviews were conducted in person whenever possible. Previous research indicates that interview mode (telephone versus in-person) has little effect on reports of eating disorder symptoms in follow-up studies of eating disorders
(17,
18). Mean, median, and modal duration of follow-up for the full study group were 8.6, 9.0, and 9.5 years, respectively. The subjects were paid for the initial and each follow-up interview.
Measures
At baseline, each participant’s lifetime axis I psychiatric history was assessed by using the Schedule for Affective Disorders and Schizophrenia—Lifetime Version
(19) that was modified to include DSM-III-R diagnostic criteria for anorexia and bulimia nervosa. The 1983 Metropolitan Insurance Company’s height and weight norms were used to calculate percent expected body weight
(20).
During follow-up assessments, the Longitudinal Interval Follow-Up Evaluation
(21), adapted for eating disorders by inclusion of a section to probe for symptoms of eating disorders, was used to assess eating pathology, comorbid axis I disorders, psychosocial function, and treatment. In addition to the behavioral eating disorder symptoms indicated in DSM-III-R, the following DSM-III-R cognitive symptoms were probed: fear of becoming fat, misperception of body weight or shape, and overconcern with weight or shape. Undue influence of weight or shape on self-evaluation was not measured because this was introduced in DSM-IV in 1994 after the initiation of the longitudinal study. Research has indicated that both overconcern with weight and shape and undue influence of weight and shape were equally effective in differentiating patients with bulimia nervosa from comparison subjects with no eating disorders
(22). Relevant to the present study, the Longitudinal Interval Follow-Up Evaluation adapted for eating disorders probed for information to determine the presence of comorbid mood disorders, alcohol use disorders, and drug use disorders according to the Research Diagnostic Criteria (RDC), coded in weekly intervals.
Use of the following forms of treatment was also assessed on a weekly basis: individual outpatient psychotherapy, clinician-led group psychotherapy (either inpatient or outpatient), treatment with fluoxetine, and inpatient treatment. Fluoxetine was analyzed specifically because it has been associated with improved outcome and few negative side effects and, during the course of the study, was the only medication approved by the U.S. Food and Drug Administration for bulimia nervosa
(23). Coding ranges for predictor variables appear in
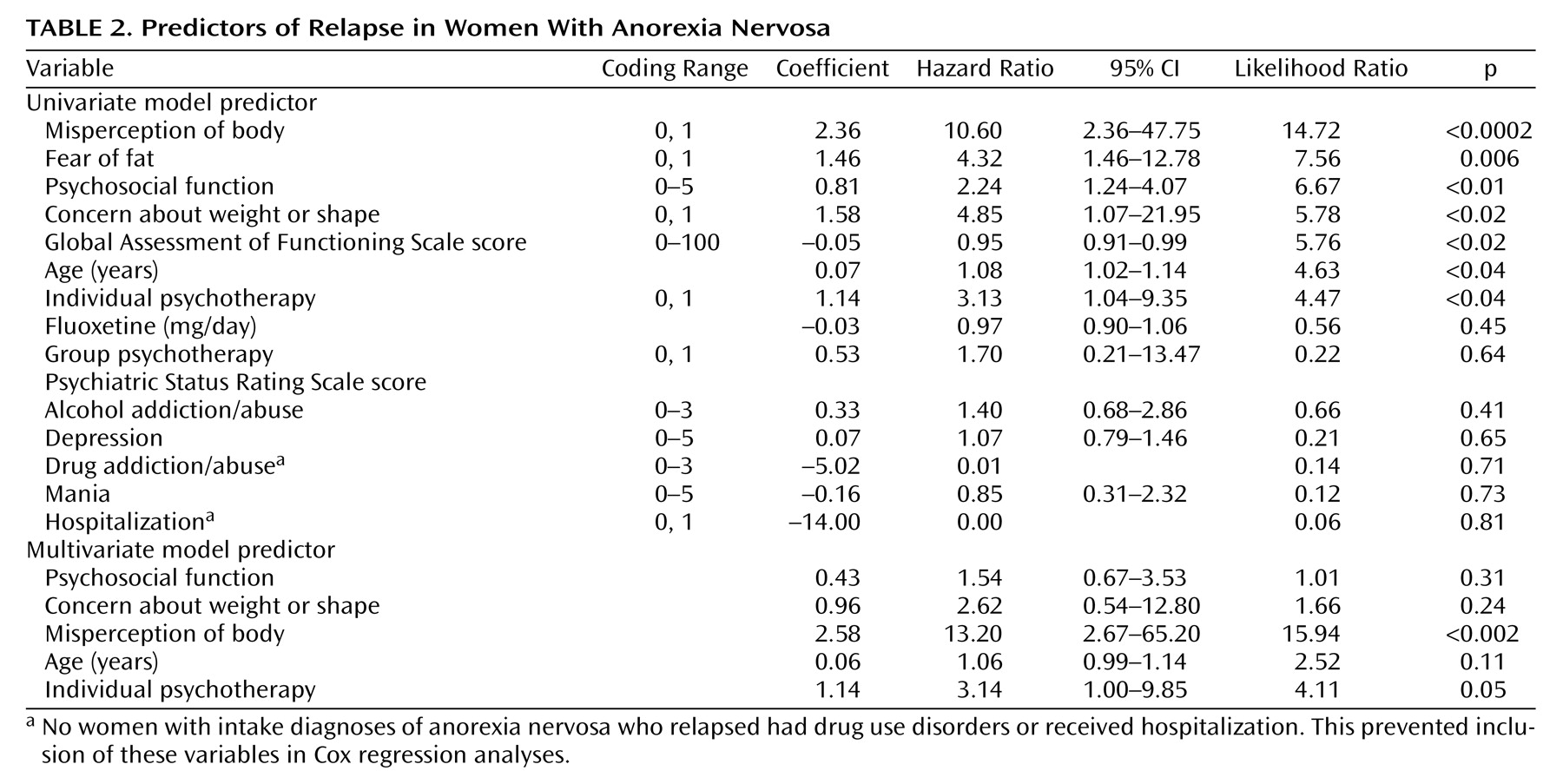
Table 2.
Training and Reliability of Interview Assessments
Because of the duration of follow-up within the longitudinal study, significant effort went into training interviewers and ensuring adequate interrater reliability. A five-step training program modeled after the National Institute of Mental Health’s Collaborative Psychobiology of Depression Study was implemented for training interviewers. First, interviewers learned the RDC nosological categories. Second, they practiced interviews on nonpatient volunteers and trained interviewers who engaged in role-playing as patients. Third, they observed and scored training tapes of expert interviewers and resolved any deviations from expert ratings. Fourth, they observed actual interviews. Fifth, they were observed by a senior interviewer while conducting study interviews. Ongoing supervision by a senior interviewer was available throughout the study.
To ensure high interrater reliability, a semiannual monitoring and recertification program was conducted. Audiotaped interviews of the participants with anorexia nervosa and those with bulimia nervosa were randomly selected for review and coding by all active raters working on the study at that time, excluding the original interviewer. Three measures of rater agreement were performed: kappa, percentage, and interclass correlation coefficients (ICC). The interviewers were required to achieve a kappa of at least 0.6; otherwise, retraining was instituted. For the most recent 6-month period for which we collected reliability data, across all categories and three raters, agreement ranged from 88% to 90% and ICCs (3,3 two-way mixed-effect, with Spearman-Brown correction) ranged from 0.93 to 0.94.
Statistical Methods
We used time-varying proportional hazards (Cox) regression
(24) to determine the influence of course variables after remission on time to relapse. Thus, week 1 represented the first week of the 8-week period that defined remission. Predictors were examined prospectively from week 1 until 12 weeks before the onset of relapse. By time-lagging predictor variables, we ensured that the predictors preceded the event they were intended to predict rather than potentially being a consequence of relapse. We focused on variables measured prospectively after remission to take advantage of the prospective study design and because these variables have the greatest relevance as targets for relapse prevention.
Nested models were compared by using the likelihood ratio test statistic that follows a chi-square distribution. A Cox model produces a model coefficient (βi), a hazard ratio (exp[βi]), a confidence interval (CI) for the hazard ratio, a likelihood ratio for the coefficient, and a p value for the coefficient. Hazard ratios greater than 1 increase hazard (shorten time to relapse), and ratios less than 1 decrease hazard (lengthen time to relapse). A ratio that does not differ significantly from 1 has no statistically significant effect on time to relapse. Because of the large number of univariate analyses, a p value of 0.01 was set for statistical significance for interpretation of these analyses.
Finally, we developed a multivariate regression model to predict time to relapse using methods suggested by Hosmer and Lemeshow
(25). Briefly, this approach involves inclusion of variables demonstrating a univariate association with an outcome at the p≤0.20 level as well as any variables of clinical importance, regardless of their univariate association. After fitting this initial multivariate model, each covariate of the model is removed. The remaining covariates are evaluated to determine whether the new model has lost an important effect (a 20% or greater change in the coefficient of any of the remaining covariates is evidence of an important interaction or confounding effect for the removed covariate). This process continues until no variables can be removed from the model. A p value of 0.05 was set for statistical significance of variables in the final multivariate model. Statistical analyses were performed using the R statistical package
(26,
27).
Results
Forty-two women with intake diagnoses of anorexia nervosa (31%) achieved remission during the course of follow-up. Among these women, 15 relapsed (representing 36% of those whose illness remitted, or 11% of the total group). Although there was no significant difference in the rates of relapse between the women with intake diagnoses of restricting anorexia nervosa and the women with intake diagnoses of binge-purging anorexia nervosa, the majority of the women who relapsed reported binge eating (10 of 15, 67%) or purging (11 of 15, 73%) during their relapse episode. One-third (5 of 15, 33%) of the women with intake diagnoses of anorexia nervosa developed bulimia nervosa in their relapse episode. Only two women (13%) reported no bulimic symptoms during their relapse episode. One of these women had an intake diagnosis of anorexia nervosa, restricting subtype, and the other woman had an intake diagnosis of anorexia nervosa, binge-purge subtype.
Eighty-three women with intake diagnoses of bulimia nervosa (75%) achieved remission during the course of follow-up. Among these, 29 relapsed (representing 35% of those whose illness remitted, or 26% of the total group). In contrast to symptomatic patterns in the relapse of anorexia nervosa, most patients with intake diagnoses of bulimia nervosa who relapsed returned to having symptoms of bulimia nervosa (27 of 29, 93%). Only two women (7%) developed anorexia nervosa in their relapse episode. Despite differences in remission rates and patterns of symptoms after relapse, the women with intake diagnoses of anorexia nervosa and bulimia nervosa did not demonstrate significantly different relapse rates (log rank χ2=0.0007, df=1, p=0.98). Thus, just over one-third (35%) of both groups with remitted illnesses relapsed.
Table 2 presents predictors of relapse in women with anorexia nervosa. From univariate models of variables measured prospectively after remission, predictors of relapse included misperception of body weight or shape, fear of gaining weight or becoming fat, and worse psychosocial function. In the final multivariate model for anorexia nervosa, psychosocial function, overconcern with weight or shape, misperception of body weight or shape, age, and individual psychotherapy all demonstrated a significant effect. Among these variables, a misperception of body weight or shape and more individual psychotherapy demonstrated statistical significance in increasing the risk of relapse.
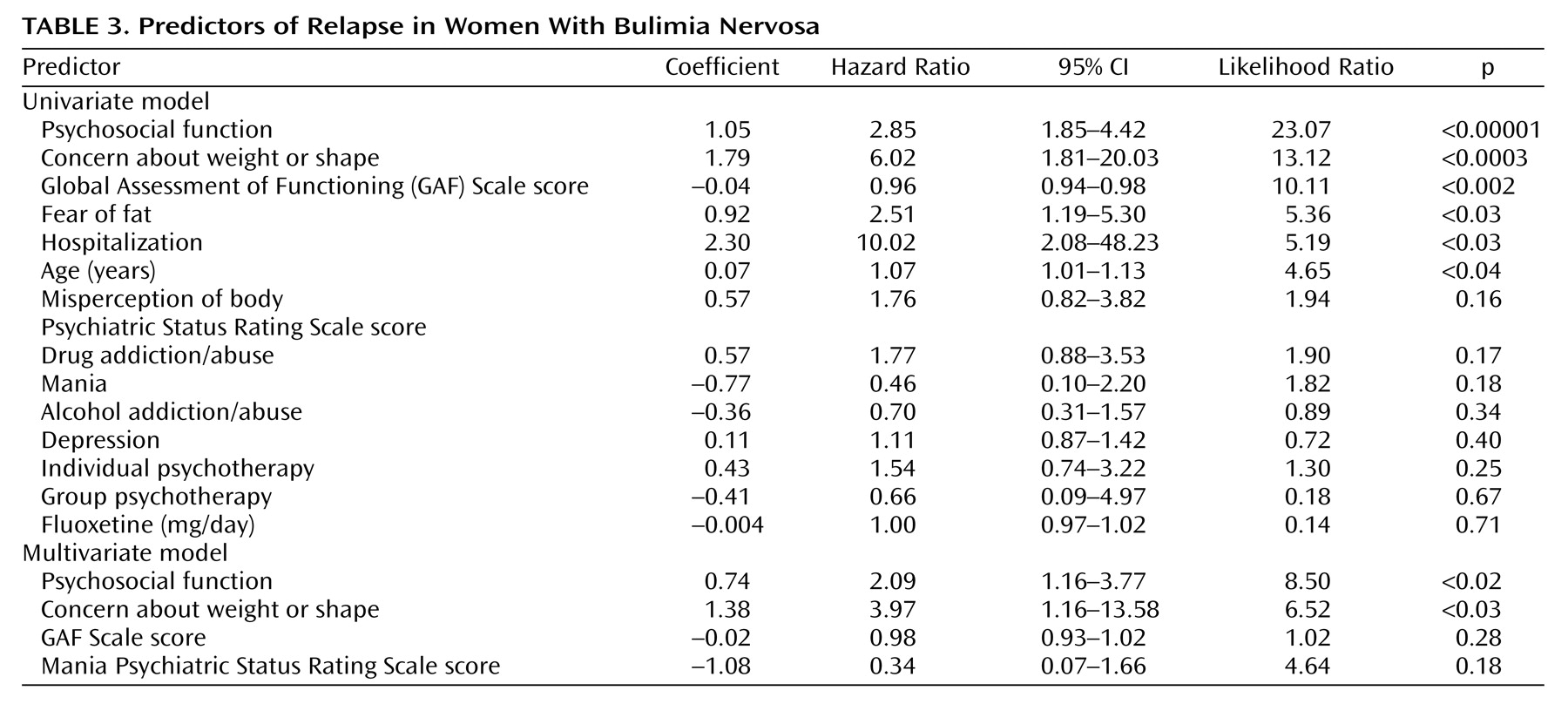
Table 3 presents predictors of relapse in women with bulimia nervosa. From univariate models of variables prospectively measured after remission, predictors of relapse included worse psychosocial function, overconcern with weight or shape, and worse scores on the Global Assessment of Functioning Scale (GAF) (DSM-IV). In the final multivariate model for bulimia nervosa, psychosocial function, overconcern with weight or shape, GAF Scale scores, and mania score on the Psychiatric Status Rating Scale all demonstrated a significant effect. Among these, worse psychosocial function and overconcern with weight or shape demonstrated statistical significance in increasing the risk of relapse.
Discussion
Overall, just over one-third of the women who recovered from either eating disorder relapsed. These rates are consistent with previous studies
(1–
5). One interesting distinction between relapse in women with anorexia nervosa and women with bulimia nervosa is the extent to which crossover occurred predominantly in one direction. That is, the women who recovered from anorexia nervosa frequently relapsed into a bulimic syndrome. However, the women who recovered from bulimia nervosa did not relapse into an anorexic syndrome. This may reflect factors that contribute to achieving remission, a prerequisite for relapse. A minority of women with intake diagnoses of anorexia nervosa achieved remission over the period of observation (N=42, 31%). Thus, we examined relapse predictors in women with anorexia nervosa who were in some ways less representative of their diagnostic group. Conversely, most women with bulimia nervosa did achieve remission (N=83, 75%). Potentially, features that contribute to an increased probability of remission may have made women from both diagnostic groups more similar, contributing to similar rates of relapse and relapse symptom patterns, even though these features are fairly common in women with bulimia nervosa and not as common in women with anorexia nervosa. Such features may relate to the difficulty of sustaining low weight, either because of metabolic pressure to maintain weight or behavioral pressure to develop binge episodes in response to dietary restriction.
Like findings from previous investigations
(9,
10), predictors of relapse included cognitive features of anorexia nervosa and bulimia nervosa. However, to the extent that these symptoms are part of the definition of both disorders, their continued presence would logically be related to the return of the full disorder. Thus, the association between body image disturbance and relapse may reflect a limitation in how we defined recovery from eating disorders
(28). Within the current study, remission was defined as a score on the Psychiatric Status Rating Scale of 1 or 2 for 8 consecutive weeks. Although both scores require abstinence from eating-disordered behaviors, a score of 2 on the Psychiatric Status Rating Scale allows lingering concerns about weight and shape. This was intended to reflect normative discontent that is present in women who have never suffered from an eating disorder, and it is consistent with how many eating disorder studies define remission
(29). Because these concerns appear to increase the risk for relapse, focused work on body image
(30,
31) may help patients achieve lasting recovery from both behavioral and cognitive symptoms of eating disorders. Unfortunately, data collected on ongoing therapy did not reveal the content of that treatment before, during, or after remission from eating disorders. After remission of an eating disorder, it is quite likely that ongoing treatment would be related to other axis I disorders. Thus, it is not possible to evaluate the possible efficacy of focused work on body image on reducing the risk of relapse in the present study group. In addition, naturalistic follow-up studies are not designed to evaluate treatment efficacy because the same factors that might predict increased treatment-seeking likely contribute to relapse
(32). This may explain why relapse in anorexia nervosa was predicted by increased individual psychotherapy.
Worse psychosocial function was retained in the final multivariate model for predicting relapse in both anorexia nervosa and bulimia nervosa and was a significant predictor in the multivariate model for relapse in patients with bulimia nervosa. This result may explain the association between psychosocial stressors and relapse previously described for bulimia nervosa
(33). Women with poor psychosocial function may be less equipped to cope with life stressors. Thus, stress coupled with poor coping may lead to a return of symptomatic behaviors. Troop and Treasure
(34) reported significant differences in coping responses to life stressors in the year before the onset of an eating disorder among patients with anorexia nervosa, bulimia nervosa, and comparison subjects with no history of eating disorders. In addition, poor psychosocial function among recovered patients may contribute to the emergence of such stressors. Such a pattern may explain why interpersonal psychotherapy has demonstrated efficacy in the treatment of bulimia nervosa at follow-up
(35). Interpersonal therapy may reduce the risk of relapse by helping women recognize and cope with psychosocial stressors that contribute to disordered eating. Alternatively, problems in psychosocial function may not directly affect the risk of relapse but may serve as a marker of a third underlying variable—such as severity of axis II pathology—that increases the risk for relapse. Although axis II disorders were assessed at baseline, they were not assessed throughout the follow-up period and could not be included in analyses of postremission predictors of relapse.
The strengths of this study include the careful assessment of the course of eating disorders in a large group of women with intake diagnoses of either anorexia nervosa or bulimia nervosa. Both the long duration of follow-up and the low rate of attrition increased the probability that events of remission and relapse were captured. The weaknesses of this study include the low rates of full remission of anorexia nervosa. Although this is representative of results from other anorexia nervosa outcome studies
(36), the low rate of remission reduced the number of women who had the potential to relapse and limited our power for the prediction of relapse. Thus, analyses for anorexia nervosa could detect only large effect sizes and may have captured some false positives. Finally, our results may not generalize to individuals who never seek treatment or who differ from our group demographically.
Future studies should examine interventions targeted at helping individuals improve body image and cope with psychosocial stressors to prevent relapse. Perhaps individuals with poor psychosocial function funnel distress into body dissatisfaction as a retreat to something they feel they can control. However, attempts to alter shape and weight do not improve psychosocial problems. Thus, the combination of poor psychosocial function and increased concern about weight and shape may trigger the return of full eating disorders. Teaching patients to cope effectively with psychosocial stressors and to accept their bodies may help prevent relapse into eating disorders.