Few major trauma events in history match the extent and scope of the Holocaust, which took place merely 60 years ago. The events of the Holocaust, in which persons faced the prospect of being killed or witnessing mass destruction of individuals and communities, clearly qualify as traumatic stressors that would predispose exposed persons to clusters of symptoms characteristic of a DSM diagnosis of posttraumatic stress disorder (PTSD). Although PTSD symptoms may be expected in the immediate aftermath of exposure and for some time afterward
(1), it appears that many of these symptoms may become ingrained and show evidence of chronicity to the extent that acute disabling PTSD symptoms, despite the time elapsed, may still be evident more than 60 years after the traumatic events
(2). In individuals with evidence of PTSD chronicity, it remains unclear, however, how other chronic psychiatric illnesses interact with the traumatic experience and posttraumatic symptoms.
Many Holocaust survivors do not voluntarily disclose their experiences. In addition, some commentators have suggested that the Holocaust, taught as history, has been ignored by many persons in the mental health community. For example, Vigoda wrote: “The patient didn’t talk, and the psychiatrist didn’t know how to ask.…There was a lot of difficulty in dealing with the fear, the loss, the sadness, the loneliness”
(3). Routine brief accounts of patients’ pasts, as rendered in the context of a conventional psychiatric assessment of hospitalized Holocaust survivors, surprisingly do not include extensive personal histories and often omit features of traumatic experiences that may be difficult to elicit without special clinical attention and skills. Such special attention, we suggest, is particularly important in reevaluating patients whose initial hospitalization and diagnoses long predate more recent theoretical developments and clinical formulations regarding the association of PTSD with extreme trauma. The testimony method, pioneered by a group of Chilean therapists, is one such development
(4). The testimony method may be defined as a form of brief psychotherapy used in the treatment of survivors of “state-sponsored violence”
(5). The testimony method alleviates many chronic symptoms by transforming the painful trauma story into a cathartic experience and a document that could be useful to others. Videotaping of the testimony is framed by its purpose: the creation of an autobiographical document that has as its centerpiece the traumatic experience. It is a collaborative venture during which the interviewer recedes into the background and the patient is assisted in entering a new social context by means of the narration of personal experience
(5).
No systematic study has yet been conducted to determine the potential effects and benefits of the testimonial process in Holocaust survivors who are chronically hospitalized patients with mental illness in Israel (18% of the chronic psychiatric hospital population as of 1993)
(6). Some researchers have suggested that ventilation of feelings after severe persecution and the revisiting of previous disturbing experiences such as the Holocaust—rather than a focus on current coping mechanisms, realities, and positive emotions—may be counterproductive to an individual’s mental well-being
(7). However, it remains unknown whether recounting such experiences in the context of a controlled therapeutic environment may be beneficial for elderly patients, for whom the possibility of death is revisited because of old age and ill health
(8). We hypothesized that many of these patients may experience relief if they were enabled to share their history of severe persecution more openly. Our intention was to investigate the role of video testimony as a potentially useful clinical intervention many years after the acute traumatic event and to ascertain positive or negative effects several months after the testimony process.
Method
Study Population
The study population consisted of chronically ill inpatients at the Beer Yaakov and Lev Hasharon Mental Health Centers (two large state referral institutions in Israel) recruited in the years 2002–2003 for study participation. The subjects were drawn from the approximately 100 residents housed in the hostel section for Holocaust survivors established in 2000 at these centers. This Holocaust survivor population has an age range of 59–97 years, and all have severe, chronic mental illness. To be included in the study, subjects had to meet the criteria for having been victims of Nazi persecution, as defined by the Conference on Jewish Material Claims Against Germany, Inc. (experience of being in hiding or sequestered in ghettos or concentration labor and death camps, etc.), had to have been at least 3 years old during the time of persecution, and had to be willing and capable of telling a story, even if only in fragments. Survivors were excluded if they exhibited features of major cognitive impairment or severe psychotic disorganization that would preclude participation in the video testimony process. The study was approved by the local Helsinki Committee Ethical Review Committee and the Yale Human Investigation Committee. The subjects and their legal guardians provided signed informed consent after the nature of the study and its potential risks and benefits were fully explained. Consent was also obtained from each subject’s designated clinician. In addition to being informed of the right to terminate participation at any time during the study, subjects were informed that they had the right to prohibit the sharing of their video testimony and the right to withdraw it at any time from the Fortunoff Video Archive for Holocaust Testimonies or the locked collections for future medical training and research.
Study Design
After baseline clinical ratings, the subjects were randomly assigned to experimental and control groups. The experimental group subsequently underwent the videotaped testimony and its clinical follow-up. The control group continued to receive regular treatment. Four months later, both the experimental group and the control group again were administered the battery of clinical rating tests used at baseline in order to assess the potential significance of the video testimony. After this second evaluation, the control subjects provided video testimony. Four months after the video testimony intervention in the control group, the group again was administered the clinical assessment battery. Both groups continued to receive their regular pharmacological treatment throughout the study.
Clinical Assessments
Patients were rated at baseline and at 4-month intervals for the 8-month duration of the study by means of the Positive and Negative Syndrome Scale
(9) and the Clinical Global Impression (CGI) severity and improvement scales
(10). In addition, each subject was rated with the Clinician-Administered PTSD Scale, Form 2
(11), Structured Interview for Disorders of Extreme Stress
(12), and Mini-Mental State Examination (MMSE)
(13). Each subject was evaluated by the same research physician (R.D.S. or B.F.) for the duration of the study in order to preserve continuity and uniformity of assessments.
Patient Monitoring
The study was carried out in an inpatient setting where patients were closely monitored and assessed daily for any adverse events or clinical deterioration after the video testimony intervention. Guidelines for the study stipulated that any evidence of worsening in clinical state was grounds for immediate termination from the study.
Video Testimony
Before the video testimony, the interviewing staff (D.L., I.F., and three additional trained psychologists) underwent a training workshop that covered the organization and content of the video testimony process and outlined interviewer conduct during the process. The video testimony consisted of a preinterview that was intended to acquaint the subject with the interviewer, provide a preliminary impression of the subject’s persecution history, and provide an opportunity for the researchers to respond to any concerns expressed by the subject. The video testimony itself lasted up to 3 hours and was carried out over one or two interview sessions, depending on the subject’s needs, ability, and willingness to give testimony. During a follow-up interview, the interviewer solicited further thoughts and reflections, and the subject had the opportunity to discuss any symptoms or difficulties that occurred after the testimony. The hospital-appointed psychiatrist familiar with each patient was present on-site and available throughout all study procedures. Interviews were conducted in the subject’s preferred language (Hebrew, Yiddish, German, or Polish). While obtaining the subject’s personal and persecution history, the interviewer placed particular emphasis on eliciting details about the individual’s Holocaust experience, “reentry” from persecution, any experiences of waiting for someone to return, the rebuilding of lost ties (with family members, friends, and community members), complicated grief processes, and the early treatment process after mental illness was recognized.
At the conclusion of each interview, the two interviewers discussed the findings and presented a clinical formulation of the subject to representatives of the subject’s treatment team. The treatment team could then decide on short- or long-term treatment interventions, which may have included changes in the patient’s living conditions, reconciliation with and return to living with family members (with any necessary social supports), a change in vocational activities (e.g., supervised leisure activities, sheltered workshops, involvement in art activities), consistent group involvement with other patients who are Holocaust survivors, and gradual development of a stable, continuous one-to-one therapeutic relationship between a member of the treatment team and the patient.
Statistical Analysis
Associations between variables were performed by using Pearson’s correlation coefficients. Changes in CGI and MMSE scores were analyzed by using paired t tests. Changes in Positive and Negative Syndrome Scale scores were analyzed with two-by-three multivariate analysis of variance (MANOVA), with session (before, after) and Positive and Negative Syndrome Scale cluster (positive, negative, general) as within-subject factors. A gender effect was added to the model to form a two-by-two-by-three MANOVA. Significant interactions were analyzed by using Tukey’s honestly significant difference post hoc comparisons. Similar two-by-three analysis of variance (ANOVA) models were applied to the Clinician-Administered PTSD Scale, Form 2, subclusters. Scores on the intensity and functional impairment subclusters were analyzed by using paired t tests. Change of PTSD symptoms was analyzed with the sign test. The prediction of the proportional change in the intensity score was analyzed with a multiple regression model, with stepwise selection of predictors (alpha=0.05). Scores on subscales of the Structured Interview for Disorders of Extreme Stress were analyzed with two-by-six MANOVAs, with session and cluster as within-subject factors, followed by paired t tests. Associations with gender were tested with chi-square tests or grouped t tests, as appropriate, depending on the nature of the variables. In addition, a two-by-two-by-three MANOVA was performed with gender as a between-subject factor and session and cluster as within-subject factors.
Results
The initial study group included 24 patients (10 women, 14 men). Before the analysis, data for three patients with no postinterview assessments were omitted (one subject died of natural causes [cancer] and two subjects refused the 4-month posttestimony interview). Age ranged from 60 to 85 years (mean=71.9 years, SD=7.2). The subjects’ countries of origin were as follows: Poland (N=7), Romania (N=5), Hungary (N=3), and France, Greece, Yugoslavia, Czech Republic, Russia, and Morocco (N=1 each).
The two preinterview clinical ratings were tested for six control subjects (control subjects had two clinical ratings before the video interview in order to maintain the single-blind nature of the study). The Clinician-Administered PTSD Scale, Form 2, total severity score was higher at the clinical rating, compared to the second/first (first: mean=16.75, SD=15.41; second: mean=34.50, SD=10.38) (t=3.47, df=3, p=0.04). No differences were observed on any measure of any of the other rating scales. The second group of ratings of the control subjects was therefore used for comparison with the postinterview ratings.
Positive and Negative Syndrome Scale, CGI, and MMSE Scores
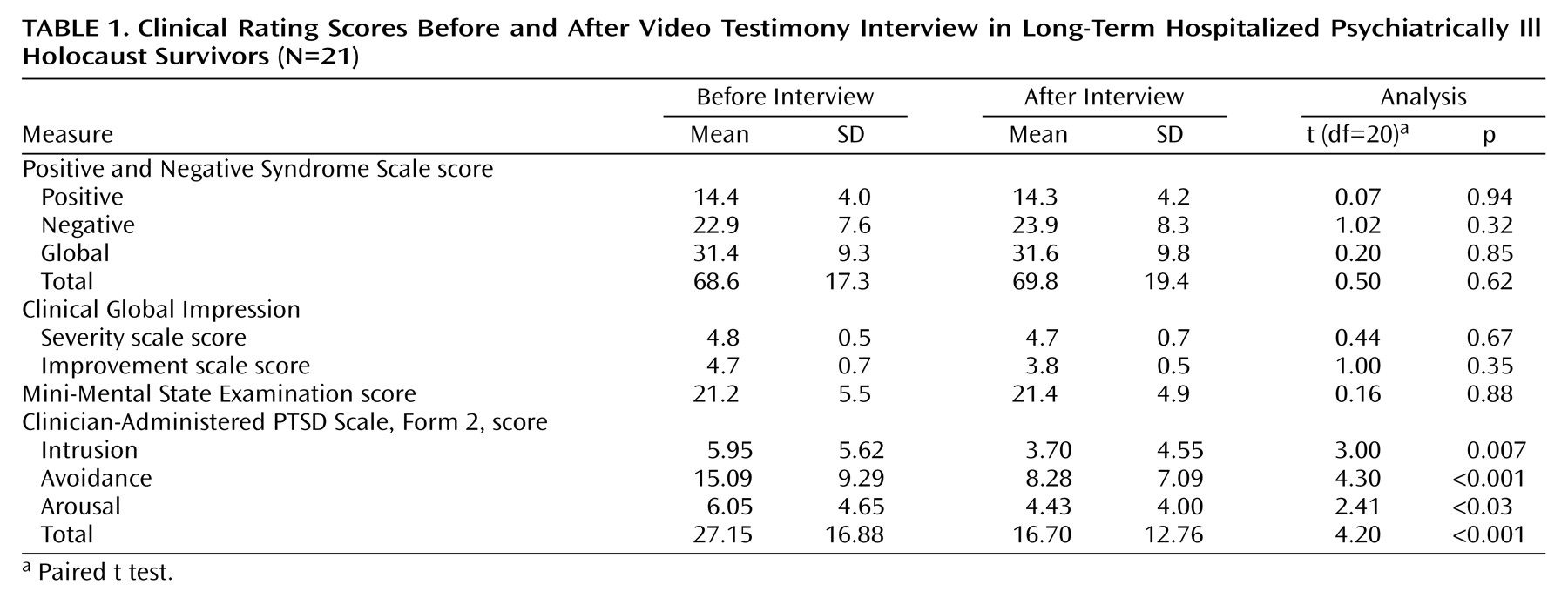
No differences were observed between pre- and postinterview Positive and Negative Syndrome Scale subscale or total scores, CGI scores, or MMSE scores (
Table 1). Correlation analysis revealed that the Positive and Negative Syndrome Scale subscale scores before and after the intervention were associated, with coefficients ranging between 0.71 and 0.89 (all significant at p<0.001).
Clinician-Administered PTSD Scale, Form 2, Scores
PTSD diagnosis
Clinician-Administered PTSD Scale, Form 2, data were analyzed according to the DSM-IV criteria required for a diagnosis of PTSD (endorsement of at least one intrusion, three avoidance, and two hyperarousal items). At the first interview eight patients (38.1%) met the criteria for PTSD; only four patients (19%) met those criteria by the second interview. This difference of 50% was not significant (p=0.12, sign test). It should be noted, however, that although not all subjects exhibited a level of symptoms that met the threshold for a diagnosis of PTSD, all subjects in general reported some posttraumatic symptoms, and many of these “subthreshold” symptoms showed improvement in the majority of the participating subjects.
Symptom severity
Analysis of data on symptom severity revealed a more definitive picture (
Table 1). Severity data were based on the sum of frequency and intensity measures of the Clinician-Administered PTSD Scale, Form 2; the total severity score is the sum of the scores for the three diagnostic clusters (avoidance, intrusion, arousal). There was a significant reduction of symptom severity for all diagnostic clusters, with avoidance severity showing the most robust reduction. This result was supported by a two-by-three MANOVA with session (before, after) and cluster (avoidance, intrusion, arousal) as the within-subject factors; this analysis revealed a significant session effect (F=17.65, df=1, 19, p<0.001) and a significant session-by-cluster interaction (F=8.78, df=2, 38, p<0.001). Tukey’s honestly significant difference post hoc comparisons indicated a significant reduction in avoidance symptoms (p<0.001) but not in intrusion and arousal symptoms.
Frequency and intensity data
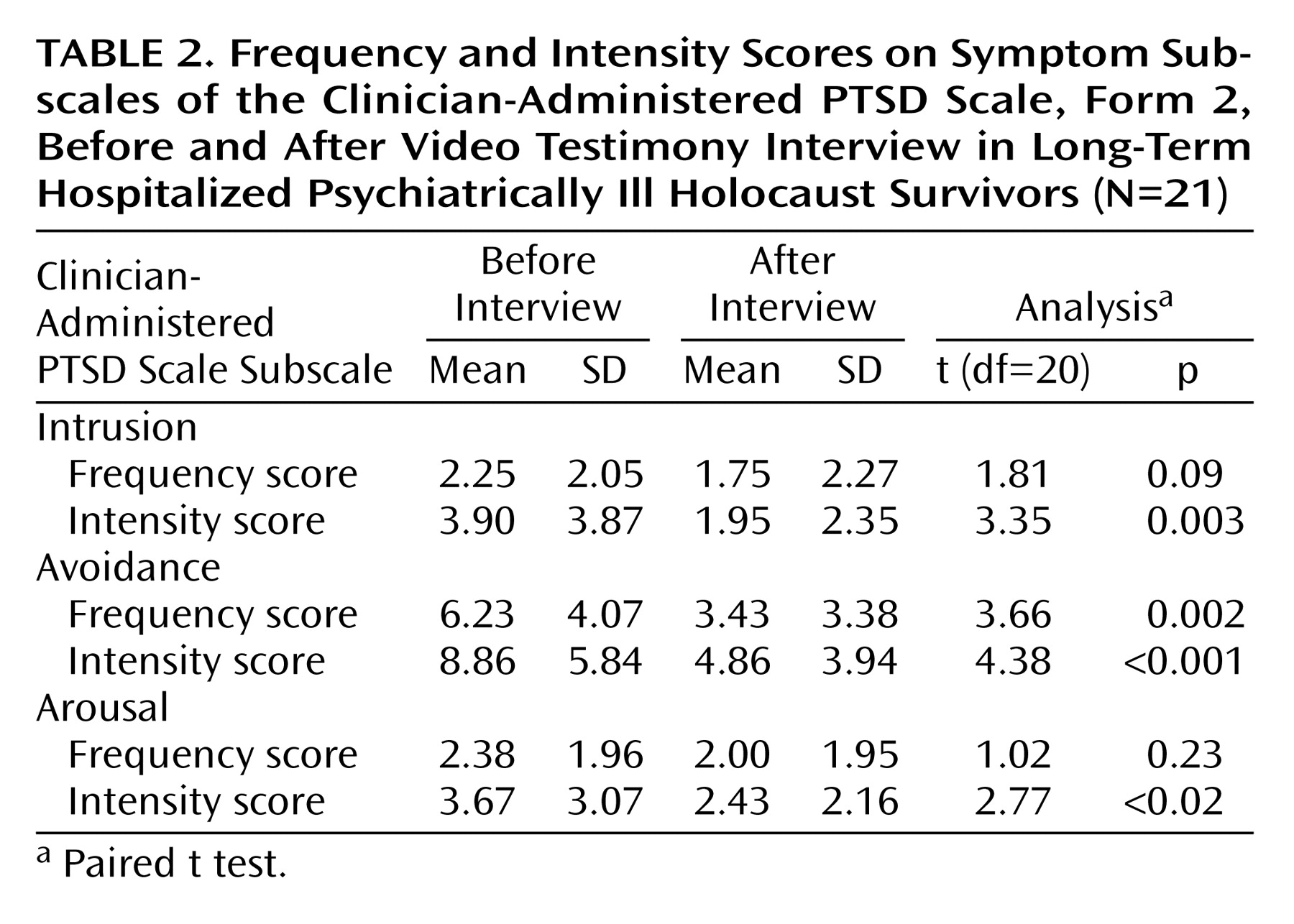
In order to elucidate the source of the differences, the symptom frequency and intensity data were tested separately (
Table 2). There was a significant reduction in the intensity of the three diagnostic clusters. However, a significant change of frequency was seen only in the avoidance cluster. An analysis of frequency data (
Table 2) was done with a two-by-three MANOVA, with session (before, after) and cluster (avoidance, intrusion, arousal) as within-subject factors; a significant session effect (F=13.97, df=1, 19, p<0.001) and a significant session-by-cluster interaction (F=8.30, df=2, 38, p<0.001) were found. Tukey’s honestly significant difference post hoc comparisons indicated a significant reduction in avoidance symptoms (p<0.001) but not in intrusion and arousal symptoms. In the analysis of the intensity data (
Table 2), a two-by-three MANOVA with session (before, after) and cluster (avoidance, intrusion, arousal) as within-subject factors yielded a significant session effect (F=18.64, df=1, 20, p<0.001) and a significant session-by-cluster interaction (F=9.17, df=2, 40, p<0.001). Tukey’s honestly significant difference post hoc comparisons indicated a significant reduction in avoidance symptoms (p<0.001) and in intrusion symptoms (p<0.01) but not in arousal symptoms.
Functional impairment
In addition to the presence of the three major diagnostic clusters, the DSM-IV criteria for PTSD include functional impairment. Although this requirement may seem redundant in a hospitalized population, analysis of the functional items of the Clinician-Administered PTSD Scale, Form 2 (items 18 and 19 indicating social and occupational functioning, respectively), showed that a reduction in impairment was present from the preinterview (mean=3.38, SD=1.94) to the postinterview session (mean=2.62, SD=1.88) (t=2.61, df=20, p<0.02).
Associated features
Of the associated features assessed with the Clinician-Administered PTSD Scale, Form 2 (items 23–30), only severity (frequency plus intensity) of memory impairment showed significant improvement postintervention (before: mean=3.67, SD=1.11; after: mean=2.67, SD=1.75) (t=2.84, df=17, p<0.02).
Change in total severity scores
The proportional change in total severity score (severity after interview/severity before interview) was calculated for each patient. Proportional changes equal to 1.00 indicate no improvement or worsening of PTSD symptoms, changes less than 1.00 indicate improvement (after < before), and changes greater than 1.00 indicate worsening (after > before). Data for one patient were omitted from the analysis because of major fluctuations in the proportional change scores, including a 570% increase in the arousal score and decrease of 4% in the intrusion score. The average proportional change was 0.68 (SD=0.34), with a range from 0.12 to 1.05. Six subjects showed no change, and one subject showed an increase of symptoms (proportional change=1.05). All other subjects showed improvement, and nine subjects had improvement of 30% or more. Of the three symptom clusters, the intrusion cluster had the greatest change (mean change=0.67, SD=0.42, median=1.0), followed by the avoidance cluster (mean change=0.72, SD=0.37, median=0.86), and the arousal cluster (mean change=0.78, SD=0.35, median=0.85). A regression model predicting the total severity of proportional change, with age, sex, severity of intrusion, severity of avoidance, and severity of arousal as predictors, was significant (F=8.20, df=2, 12, p=0.003) and explained 50% of the variance. Significant predictors were preinterview severity of avoidance (beta=–0.85, t=4.05, p=0.001) and preinterview severity of arousal (beta=0.47, t=2.30, p=0.04). The results suggest that higher avoidance scores and lower arousal scores predict greater reduction of total severity scores.
Structured Interview for Disorders of Extreme Stress Scores
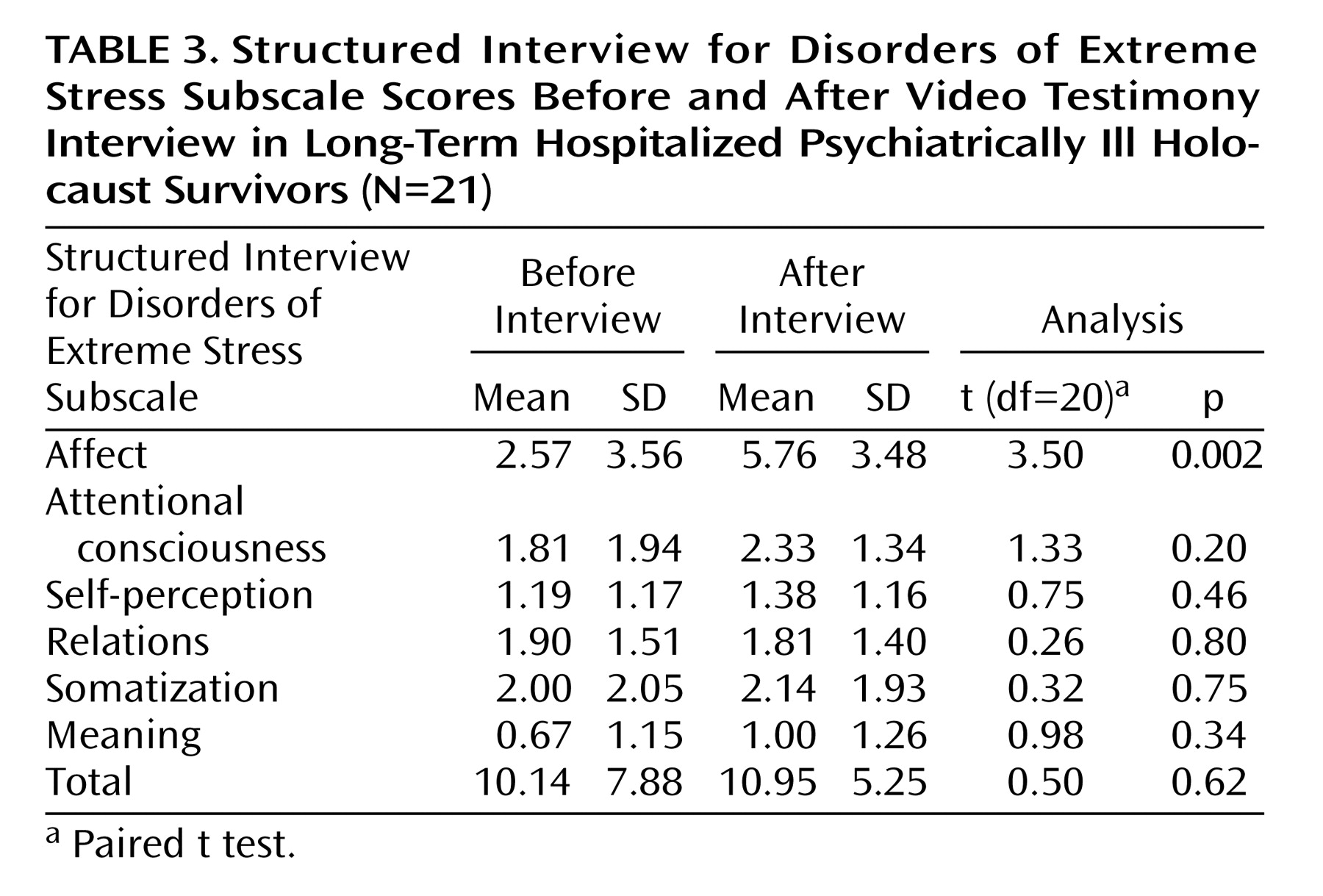
Data from the Structured Interview for Disorders of Extreme Stress were analyzed according to the six subscales and a total score (
Table 3). In general, the postinterview scores tended to be higher than the preinterview scores. The two-by-six ANOVA model did not reveal a significant main effect of session or a session-by-cluster interaction. However, a significant increase occurred after the video interview in scores the subscale that measures alteration and regulation of affect and impulses. No other changes were detected after the interview.
Video Interview Responders
Patients were defined as responders to the video interview if their proportional severity score showed a reduction of 30% or more and as nonresponders if the reduction was less than 30%. According to this categorization, 11 patients were responders and another 10 were nonresponders. Associations between response category and background and clinical data were calculated. Only three variables showed associations with response category: preinterview avoidance frequency and intensity scores (for both, responder > nonresponder) and postinterview Structured Interview for Disorders of Extreme Stress subscale of attention consciousness (responder < nonresponder). It should also be noted that of the seven subjects with initial PTSD who completed the study (the eighth patient refused the poststudy interview), five showed an improvement of 30% or more (range=30% to 66%), one patient showed milder improvement of 11%, and another patient showed no change.
Gender Effects
Before the video testimony interview, female subjects had a higher prevalence of PTSD symptoms (55.6%) than male subjects (16.7%), although the difference only approached significance (χ2=3.50, df=1, p=0.06). This differential effect remained after the interview process, with 33.3% of female subjects and no male subjects meeting the PTSD criteria (χ2=4.67, df=1, p<0.04). A two-by-two-by-three MANOVA analysis of the severity of different diagnostic clusters revealed a significant gender effect (F=12.59, df=1, 18, p=0.002) but no gender interaction. Female patients had higher severity scores both before and after the interview (before: mean=39.12, SD=17.10; after: mean=26.00, SD=14.26), compared to male patients (before: mean=19.17, SD=11.50; after: mean=10.50, SD=6.87). A significant main effect of gender was observed for total Positive and Negative Syndrome Scale scores (F=5.49, df=1, 19, p=0.03); male patients had higher Positive and Negative Syndrome Scale scores both before and after the interview (before: mean=74.73, SD=17.73; after: mean=78.17, SD=18.33), compared to female patients (before: mean=61.00, SD=14.34; after: mean=58.67, SD=18.32). A two-by-two MANOVA performed on CGI severity scores revealed a significant gender effect (F=4.50, df=1, 16, p<0.05) and a significant gender-by-session interaction. The scores of male patients increased after the interview (before: mean=4.89, SD=0.60; after: mean=5.11, SD=0.60), and those of female patients decreased (before: mean=4.67, SD=0.50; after: mean=4.33, SD=0.50). Post hoc comparisons with Tukey’s honestly significant difference test revealed that male and female patients differed only on postinterview scores (p<0.001). No gender differences were observed for CGI improvement, MMSE, and Structured Interview for Disorders of Extreme Stress scores.
Associations Between Clinical Measures
Associations observed between total rating scores included an inverse correlation between total Clinician-Administered PTSD Scale, Form 2, scores and total Positive and Negative Syndrome Scale scores both at baseline (r=–0.45, N=20, p<0.05) and at follow-up (r=–0.44, N=21, p<0.05) and a positive correlation between CGI severity scale scores and total Positive and Negative Syndrome Scale scores at baseline (r=0.62, N=18, p=0.006) and at follow-up (r=0.75, N=18, p<0.001).
Discussion
The study results indicate significant improvement in posttraumatic symptoms in chronically hospitalized psychiatrically ill Holocaust survivors after video testimony, although no difference was noted in psychotic symptoms. A notable improvement of symptom severity was observed in all PTSD diagnostic clusters, particularly in severity of avoidance. Because the content of the traumatic event was being addressed and focused on, increases were noted in the current relevance of the event to the individual. Greater PTSD severity scores were noted in female subjects, similar to findings in other studies
(14). It is interesting to note that a decrease in overall illness severity (CGI severity scale score) was found in female subjects, compared to a slight increase in male subjects, suggesting that women in particular may benefit from such video testimony.
In addition to the expected and intuitive correlation between illness severity and psychotic symptoms, a particularly noteworthy finding of the study is the observation of an inverse correlation between PTSD symptoms and overall psychotic state. Although this finding is speculative, it may be explained by an increased awareness of and increased capacity to focus on traumatic memories in patients with less severe psychosis who would then be exposed to more painful memories and the potential for posttraumatic symptoms. Moreover, a highly psychotic state with major mechanisms of denial and distortion of reality may serve as a protective shield against the real experience of the traumatic event. When psychosis is less pronounced, awareness of the “real world” and painful memories comes to light. From a psychoanalytic perspective, the relationship between Clinician-Administered PTSD Scale, Form 2, and Positive and Negative Syndrome Scale scores can be attributed to the gender effect noted previously. The finding that female patients scored higher on PTSD symptom scales might be related to a gender difference in ability to maintain “neurotic defenses” in the face of extreme traumatization such as the Holocaust. Female patients may have been able to maintain such defenses and, as a result, developed PTSD symptoms in the face of trauma, while male patients were less able to maintain such defenses and developed psychotic features.
The psychotherapeutic benefits of the testimonial process, observed in traumatized political refugees
(5), may also be observed in Holocaust survivors with severe, chronic mental illness who were victims of persecution and human rights violations. Sharing the story through testimony psychotherapy, even in the context of a single extended interview process many years after the intensely traumatic event, can reduce chronic posttraumatic symptoms and thus may be likely to improve psychosocial functioning and quality of life. Evidence for such improvement may be noted in the following vignette. “Sara” described hiding in a house for 2 years in Belgium before being reported to the Gestapo by a neighbor:
We lived in constant fear and were always scared. We never left the house in 2 years…in the end they really did come and get us. They took us all standing in a cattle car to Auschwitz. Three days. Three nights. There they separated us from Mother. We never saw her again.
The hospital staff members had not been aware of Sara’s experience of hiding and were not aware of the intensity of her experiences during the war. Her psychiatric history supported a consistent picture of anxiety related to traumatic experience. She still had nightmares about her experiences at Auschwitz. She rarely ventured outside the hospital premises, and on occasions when she was convinced to participate in outings, she remained tense and hypervigilant. After Sara’s video testimony, staff members more clearly recognized the connection between her traumatic childhood and her suspicious behavior, lack of trust, and self-neglect. After the interview and her sharing of her experience, her rapport with staff and involvement in activities, including outings, significantly improved.
We are by no means the first researchers to interview Holocaust survivors about their experiences. Many others have done so, including David Boder, who used primitive wire-recording devices in interviews in the late 1940s
(15). However, we appear to be one of the first groups to use the testimony method with the goal of symptom monitoring at baseline and at follow-up. We suggest the process of creating video testimonies can be cathartic, as well as a source of material for therapeutic work and modification of the treatment approach. Moreover, the testimonial event may set in motion a process of self-reflection and a need to share thoughts about past experiences with fellow patients, family members, and health care providers. This process results in an overall improvement in posttraumatic symptoms, despite a lack of noticeable effect on the underlying schizophrenia illness. In addition, it can be expected that improvement in posttraumatic symptoms will have secondary effects on depressive ideation, which is frequently associated with PTSD in Holocaust survivors
(16). The positive effects of video testimony were observed regardless of the subject’s age at the time of the Holocaust experience. Because individuals with severe mental illness such as schizophrenia may underreport trauma exposure, the results of this study suggest the importance of addressing such issues in individuals who may be expected to have developed PTSD symptoms, given their exposure to trauma, but who may not overtly report such symptoms
(17).
After providing videotaped testimony, subjects may finally feel relieved to some extent of the burden of their story because it has been entrusted to safekeeping, and they may no longer fear that the knowledge will vanish. The benefits of testimony are likely to be generalizable to other patients with PTSD and psychosis, especially those who have experienced severe persecution. The study results provide the grounds for further specific studies of severe and long-standing PTSD, which may be associated with psychosis, and of the therapeutic effect and impact of testimony on individualized treatment. In addition, by giving their testimonies to the Fortunoff Video Archive for Holocaust Testimonies, individuals are afforded the opportunity to help create for themselves and others a living memorial to counteract forgetfulness, ignorance, and Holocaust denial.
Although the study observations indicating improvement in PTSD symptoms (and not psychosis) after testimony were robust, the findings may to some extent challenge the idea that patients who have been chronically hospitalized with a schizophrenia diagnosis may instead have chronic PTSD with psychosis
(6). The scenario of PTSD with psychosis masquerading as schizophrenia has been suggested for populations with childhood sexual and physical abuse
(18) and combat trauma
(19), as well as other subpopulations exposed to severely traumatic events (reviewed in reference
20). In addition, classic psychoanalytic theory suggests that psychosis is a defensive response against intense internal traumatic experience
(21). Further investigation is required to clarify whether some of the patients in this study may have chronic PTSD with associated psychosis rather than chronic schizophrenia. It is important to note that regardless of the diagnostic formulation (PTSD with psychosis or schizophrenia), the study observations indicate that treatment approaches such as the testimony intervention appear to be beneficial.
It is interesting to note that individuals with schizophrenia may be more vulnerable to the development of PTSD because of a higher risk of exposure to trauma in general, a lower threshold for coping with stressful life events, and potentially decreased inhibitory function of dopamine in the locus ceruleus as a result of chronic antipsychotic use, leading to noradrenergic activity enhancement and arousal as seen in PTSD (reviewed in reference
22). An alternative hypothesis within the context of a stress-diathesis model is that dehumanizing trauma and consequent PTSD provokes schizophrenia in vulnerable individuals who otherwise may not have become psychotic
(22).
In this study, the mean MMSE score suggested signs of dementia in many subjects. Although Yehuda et al.
(23) found accelerated cognitive decline and specific memory disturbances in Holocaust survivors with chronic PTSD symptoms, it remains unclear whether the relatively low MMSE scores in our study were influenced by the subjects’ chronic PTSD symptoms or were solely a reflection of chronic schizophrenia and the aging process. It has also been suggested that PTSD symptoms may have a delayed manifestation and may appear only with dementia onset
(24).
Potential risks of the study, anecdotally reported by other trauma survivors who underwent video testimony, include temporary anxiety before and after the testimonial process and/or sleep disturbances. In this study, however, no short-term or long-lasting adverse effects were noted, even though the subjects were strongly encouraged to share any difficult experiences with their clinicians. The limitations of the study include the inability to generalize the findings to other traumatized groups, given the relative uniqueness of the trauma and the specific ethnocultural characteristics of the subjects. Although the follow-up period in this study was limited to only 4 months, it is the intention of the investigators to follow this cohort of patients for a more extended period (more than 1 year) in order to clarify long-term effects of the study intervention.
In conclusion, the study results indicate the robust usefulness of a testimony interview in the alleviation of many posttraumatic symptoms in a cohort of psychiatrically ill Holocaust survivors, despite an interval of as many as 60 years since the traumatic event. The circumstances of the testimony process, including the use of videotaping and preservation of the interviews as part of the history of the Holocaust, may have had a special effect on these patients. In light of the videotaped testimony, aspects of the patients’ care may need to be addressed, including clinical reassessment in view of a history of trauma. For example, such a history may have resulted in symptoms that could be partly alleviated and that could be made a focus of management in many, but not necessarily in all, such patients
(25). In addition, rehabilitative efforts should address the specific needs that emanate from the interaction of past trauma, long-term hospitalization, and the processes of aging. We suggest that video testimony could come to play a role in treatment planning and in the design of a specialized treatment program for such individuals, including steps to address countertransference responses in staff. Further research in subpopulations of patients with comorbid PTSD and chronic schizophrenia is needed to clarify these findings and test them in the context of larger double-blind studies.