Caffeine is the most widely used mood-altering drug in the world, with 80% to 90% of children and adults in North America regularly consuming caffeine-containing foods
(1,
2). Mean daily caffeine consumption among adult caffeine consumers in the United States has been estimated to be 280 mg/day, which is equivalent to about three 6-oz cups of coffee or five 16-oz bottles of cola soft drink
(3,
4).
Several case report studies documented that some people fulfill the DSM-IV diagnostic criteria for substance dependence applied to caffeine use
(5–
7). In a random-digit telephone survey of 162 caffeine users, 30% fulfilled the diagnostic criteria for caffeine dependence, with 56% of caffeine users reporting a persistent desire or unsuccessful efforts to cut down or control caffeine use and 14% reporting continued use despite knowledge of a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by caffeine
(8). Although the diagnosis of caffeine dependence is not included in DSM-IV, the validity of the diagnosis is suggested by two studies that prospectively demonstrated that the incidence of withdrawal
(9) and the severity of withdrawal
(5) were greater in individuals who met the criteria for a caffeine dependence diagnosis, based on the generic criteria for DSM-IV substance dependence.
It has been well established that family members of persons with alcoholism are more likely to be alcohol dependent, and adoption and twin studies have suggested a role for genetic factors in the familial transmission of alcohol and drug dependence
(10–
14). Twin studies have also demonstrated the heritability of problematic caffeine use, including heavy caffeine use, caffeine tolerance, and caffeine withdrawal
(15,
16). With regard to a link between alcoholism and caffeine, there is a high co-occurrence between alcoholism and caffeine use
(5,
17,
18), and twin studies examining alcohol use, caffeine use, and cigarette smoking concluded that a common genetic factor (polysubstance use) underlies the use of these three substances, with 28% to 41% of the heritable effects of caffeine use (or heavy use) shared with those of alcohol use and smoking
(15,
19,
20).
Caffeine use during pregnancy has been associated with a variety of adverse consequences, including decreased fecundity, spontaneous abortion, and reduced fetal growth
(21–
24). Although methodological limitations preclude definitive scientific conclusions
(25), governmental health agencies of the United States, Canada, and the United Kingdom have issued health warnings about limiting the use of caffeine during pregnancy. The U.S. Food and Drug Administration has advised pregnant women to “avoid caffeine-containing foods and drugs, if possible, or consume them only sparingly”
(26), and Health Canada
(27) and the Food Standards Agency of the United Kingdom
(28) have advised that pregnant women consume ≤300 mg/day of caffeine. Although obstetricians frequently counsel women to reduce or eliminate caffeine use during pregnancy
(29), women often continue to consume caffeine throughout pregnancy
(30–
31).
The present study examined caffeine use in women who received advice from their obstetrician to abstain from caffeine use during pregnancy. The study sought to identify factors associated with a woman’s ability to abstain from or reduce prenatal caffeine use. The factors were a history of caffeine dependence (i.e., a lifetime diagnosis of caffeine dependence, based on the DSM-IV diagnostic criteria for substance dependence applied to caffeine use) and a family history of alcoholism. Questionnaire assessments occurred at three prenatal visits 2–3, 3–4, and 7 months after conception, and a personal interview occurred between the second and third questionnaire assessments. Because caffeine use and alcohol use are often associated and because both are known to occur more frequently in some families, it was hypothesized that women with caffeine dependence and a family history of alcoholism would have more difficulty eliminating or reducing caffeine use during pregnancy.
Method
Recruitment
Study participants were drawn from a group of pregnant women seeking prenatal care from a private obstetrics and gynecology practice in a suburban community. Independent of their current or past caffeine use, the women, who were waiting to see their practitioner at their first clinic visit after learning they were pregnant (generally about 8–12 weeks after conception), were invited to participate in a three-session questionnaire study of caffeine use in pregnancy. Of 109 women offered study participation, only nine (8%) refused. Those providing informed consent (N=100) completed a 20-minute questionnaire at this first prenatal visit. Of these, 87 (87%) completed the first follow-up questionnaire at prenatal visit 2 (occurring about 12–16 weeks after conception) and 84 (84%) completed the second follow-up questionnaire at prenatal visit 6 (occurring about 28 weeks after conception). Reasons for dropout or study discontinuation included miscarriage (N=8), change in obstetrician (N=2), decision to discontinue study participation (N=2), and unknown reasons (N=4). Data from an additional subject were eliminated from the data set because she provided contradictory responses. Thus, 83 women provided informed consent and completed all three questionnaires. When these women were offered the opportunity to participate in a personal interview, 65 (78%) consented to the interview and 50 (77%) completed the interview. Of these women, five (10%) reported no prepregnancy caffeine use, and their data were eliminated from subsequent analyses. Data from one additional participant were subsequently eliminated because she miscarried. All interview participants received $50 as compensation for their time and effort.
Participants
The final study group consisted of 44 women who provided informed consent to a personal interview about caffeine use and other health behaviors and reported some caffeine use in the 3 months before becoming aware of pregnancy. Subjects had a mean age of 31.9 years (SD=4.0); 96% (N=42) were Caucasian; 100% (N=44) were married; and 50% (N=22) had a 4-year college degree, with an additional 23% (N=10) reporting an advanced degree. Nearly three-fourths (73%, N=32) were employed full-time (>35 hours/week), and 23% (N=10) were employed part-time (≤35 hours/week). More than one-half of the women (57%, N=25) met the criteria for a lifetime diagnosis of caffeine dependence (i.e., met the DSM-IV criteria for lifetime substance dependence applied to caffeine use). Eighteen percent (N=8) met the DSM-III-R criteria for lifetime alcohol abuse (2%, N=1) or dependence (16%, N=7); however, none had a current alcohol use diagnosis, and none had been treated for alcohol problems. Seven percent (N=3) of the women met the DSM-III-R criteria for lifetime substance abuse or dependence applied to drugs other than nicotine or caffeine. All of these cases involved past (not current) cannabis use. About one-quarter (27%, N=12) of the women reported a history of daily cigarette smoking, but only three (7%) continued to smoke during their pregnancy.
More than one-half (52%, N=23) of the women reported at least one first-degree relative who met the Family History Research Diagnostic Criteria (FH-RDC) for alcoholism
(32). Specifically, 32% (N=14) of the women reported alcoholism in their biological father, 14% (N=6) in their biological mother, 11% (N=5) in both parents, and 39% (N=17) in at least one sibling. More than one-half (55%, N=24) of the subjects met the DSM-III-R criteria for a lifetime diagnosis of either a mood disorder and/or an anxiety disorder (major depression: 41% [N=18] lifetime, 2% [N=1] current; panic, obsessive-compulsive, and/or generalized anxiety disorders: 20% [N=9] lifetime, 9% [N=4] current).
Questionnaire Data and Saliva Samples
The initial questionnaire, which was completed at the first prenatal visit, assessed caffeine, tobacco, alcohol, and other drug use during the 6 months before pregnancy awareness and during the 7 days before the first prenatal visit. The two follow-up questionnaires assessed changes in caffeine and other substance use since the last visit and specifically for the 7 days before the second and sixth prenatal visits. For caffeine assessments, participants provided the number of days during the last week that they consumed caffeine-containing products as well as the number of servings, serving size, and brand of the caffeinated products they consumed. Previous studies suggested the reliability and validity of self-reports of caffeine use
(33,
34), although pregnant women may underreport drug use to health care workers
(35). The questionnaires were given to the subjects by nurses, sealed in envelopes after completion, and forwarded to research staff for data entry.
To validate the questionnaire data about caffeine consumption, participants provided a 5-ml saliva sample at the first, second, and sixth prenatal visits. The samples were used to assess caffeine levels by using methods previously described (Labstat Inc., Kitchener, Ont., Canada)
(36,
37). The saliva samples and questionnaires were labeled with research identification numbers and collected weekly by research assistants. Thus, the nursing staff and obstetrician were blind to the research data about subjects’ caffeine use throughout the course of pregnancy.
Physician’s Intervention
At the first prenatal visit, after completing the initial questionnaire and the prenatal physical examination, each participant met with the obstetrician (N.B.) for prenatal counseling. As part of the counseling session, the physician stated that caffeine use during pregnancy is associated with a variety of adverse consequences and that his recommendation was for the woman to eliminate all caffeine use for the duration of her pregnancy. In addition, the patient received written materials summarizing the consequences of caffeine use during pregnancy and the benefits of eliminating or reducing such use.
Diagnostic Interview
The diagnostic interviews were conducted by a licensed clinical psychologist (D.S.S.) between the second and third questionnaire assessments. The interview required 60–90 minutes and consisted of the Structured Clinical Interview for DSM-III-R (SCID, axis I) and the Family Alcohol and Drug Survey
(38). The SCID is a reliable and valid semistructured diagnostic interview that is used to assess mood disorders, schizophrenia and other psychotic disorders, anxiety disorders, substance-related disorders, somatoform disorders, and eating disorders
(39). For this study the SCID included a modified E-module (the section on psychoactive substance use disorders) that followed the format of the original E-module and included questions that permitted determination of a caffeine dependence diagnosis (i.e., fulfillment of the DSM-IV diagnostic criteria for lifetime substance dependence applied to caffeine use)
(5). The Family Alcohol and Drug Survey is a semistructured interview that was developed for use in a twin and family study of alcoholism
(38). The interview uses the FH-RDC, which has high reliability and validity for diagnoses of alcoholism in first-degree relatives
(32).
Data Analysis
Caffeine consumption (mg/week) was evaluated over the course of pregnancy by using three-way mixed analysis of variance (ANOVA) with caffeine dependence (lifetime diagnosis of caffeine dependence), family history of alcoholism (FH-RDC-defined alcoholism in at least one first-degree relative), and time (prepregnancy and prenatal visits 1, 2, and 6) as factors. Fisher’s least significant difference procedure was used to assess the significance of decreases in caffeine consumption over time. Planned comparisons (t tests) were used to examine differences in caffeine consumption at each timepoint in women with and without lifetime caffeine dependence and in women with and without a family history of alcoholism. Because the analysis showed an interaction between caffeine dependence and family history of alcoholism, caffeine consumption data were also examined for the four subgroups of women based on the presence or absence of caffeine dependence and a family history of alcoholism: 1) women with both caffeine dependence and a family history of alcoholism (32% [N=14] of the subjects), 2) women with caffeine dependence but no family history of alcoholism (25% [N=11]), 3) women with no caffeine dependence and a family history of alcoholism (20% [N=9]), and 4) women with no caffeine dependence and no family history of alcoholism (23% [N=10]). The analysis used a two-way ANOVA with group and time as factors. Planned comparisons (t tests) were used to examine differences in caffeine consumption at each timepoint in women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism versus all other groups combined.
Another analysis was conducted to determine whether the differences between the women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism versus all other groups combined could be attributed to other disorders. The analysis used a two-way analysis of covariance (ANCOVA) with group (women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism versus all other groups combined) and time as factors and with the following covariates: lifetime history of daily cigarette smoking, DSM-III-R alcohol abuse or dependence, DSM-III-R drug abuse or dependence, and DSM-III-R diagnosis of any other psychiatric diagnosis assessed by the SCID. This model used a type I estimable function to allow the covariates to be entered first. Follow-up planned comparisons (t tests) with the adjusted means were used to examine differences in caffeine consumption at each timepoint in women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism versus all other groups combined.
To assess the validity of self-reported caffeine consumption, Pearson’s correlation coefficients were calculated for the relationship between reported amounts of caffeine consumed (mg/week) and caffeine saliva levels (ng/ml) at each of the three prenatal visits. A t test was used to compare caffeine levels on occasions when subjects reported caffeine abstinence versus occasions when subjects reported caffeine use. Finally, in an analysis similar to that of the caffeine consumption data, caffeine saliva levels were examined for the four subgroups of women based on the presence or absence of caffeine dependence and a family history of alcoholism. The analysis used a two-way mixed ANOVA with subgroup and time (prenatal visits 1, 2, and 6) as factors. Planned comparisons (t tests) were used to examine differences in caffeine saliva levels at each timepoint in women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism versus all other groups combined.
Categorical data (e.g., rates of abstinence, history of daily cigarette smoking, lifetime DSM-III-R alcohol abuse or dependence, DSM-III-R drug abuse or dependence) were compared by using Pearson’s chi square, with Fisher’s exact two-tailed probability levels used when the number of observations per cell was five or less.
For all statistical tests, effects were considered significant at p<0.05.
Results
Caffeine Use Before Pregnancy
In response to the questionnaire about caffeine use before pregnancy awareness, 41% (N=18) of the women indicated that they would find it difficult to be without caffeine. Most (93%, N=41) had experience abstaining from caffeine for a day or more, and 63% (N=26) of those who had abstained endorsed one or more of the following withdrawal symptoms: headache (49%, N=20), fatigue (39%, N=16), anxiety (10%, N=4), and nausea or vomiting (2%, N=1). Fifty-two percent (N=23) of the total study group reported using caffeine to avoid withdrawal symptoms, and 21% (N=9) had previously been told by a health care professional that they should cut back or eliminate their caffeine use because of its association with or effect on various medical conditions, including fibrocystic breast disease, headaches, pregnancy, insomnia, and stomach problems. Twenty-six percent (N=11) reported that they believed they had physical problems that had been caused or made worse by caffeine.
Diagnostic Interview
More than one-half of the subjects (57%, N=25) fulfilled the DSM-IV criteria for lifetime substance dependence applied to caffeine use by endorsing three or more of the seven diagnostic criteria. The proportion of the study group that endorsed each of the seven DSM-IV criteria were: 1) tolerance as defined by a need for markedly increased amounts of the substance to achieve desired effect, or markedly diminished effect with continued use of same amount of substance (50%, N=22); 2) characteristic withdrawal syndrome or use of the substance to relieve or avoid withdrawal symptoms (77%, N=34); 3) substance taken in larger amounts or over a longer period than was intended (45%, N=20); 4) persistent desire or unsuccessful efforts to cut down or control substance use (45%, N=20); 5) a great deal of time spent in activities necessary to obtain the substance (25%, 11); 6) important social, occupational, or recreational activities given up or reduced because of substance use (0%); and 7) continued use despite knowledge of a persistent or recurrent physical or psychological problem likely to have been caused or exacerbated by the substance (43%, N=19).
Difficulties Complying With Instructions to Stop Caffeine Use
After receiving verbal and written instructions during the first prenatal visit to eliminate all caffeine during pregnancy, almost all of the women (98%, N=43) reported on prenatal visits 2 and 6 that they attempted to completely eliminate or cut back their caffeine use during pregnancy. More than one-half of these women (54%, N=23) reported one or more symptoms that they attributed to quitting or cutting back caffeine use, with 34% (N=15) reporting fatigue, 32% (N=14) sleepiness, 27% (N=12) headaches, 27% (N=12) craving for caffeine, 21% (N=9) yawning, 18% (N=8) nausea, 16% (N=7) less motivation for work, and 7% (N=3) vomiting. Fourteen percent (N=6) of the total study group (or 26% of those reporting withdrawal symptoms) reported that their caffeine withdrawal symptoms were severe enough to interfere with their performance at work, school, or home. Headache did not consistently accompany such functional impairment. Examples of functional impairment provided in written comments to open-ended questions included: “flu symptoms prevented going to work”; “less active at work”; “When I cut back, I am fatigued; it is difficult to concentrate.” Examples of reasons that women provided for failing to eliminate or cut back on their caffeine use included “cravings/headache/nervous,” “migraines,” “need to stay awake/headaches,” “severe withdrawal,” “couldn’t concentrate at work,” and “need coffee to wake up.”
Amount of Caffeine Use in Pregnancy
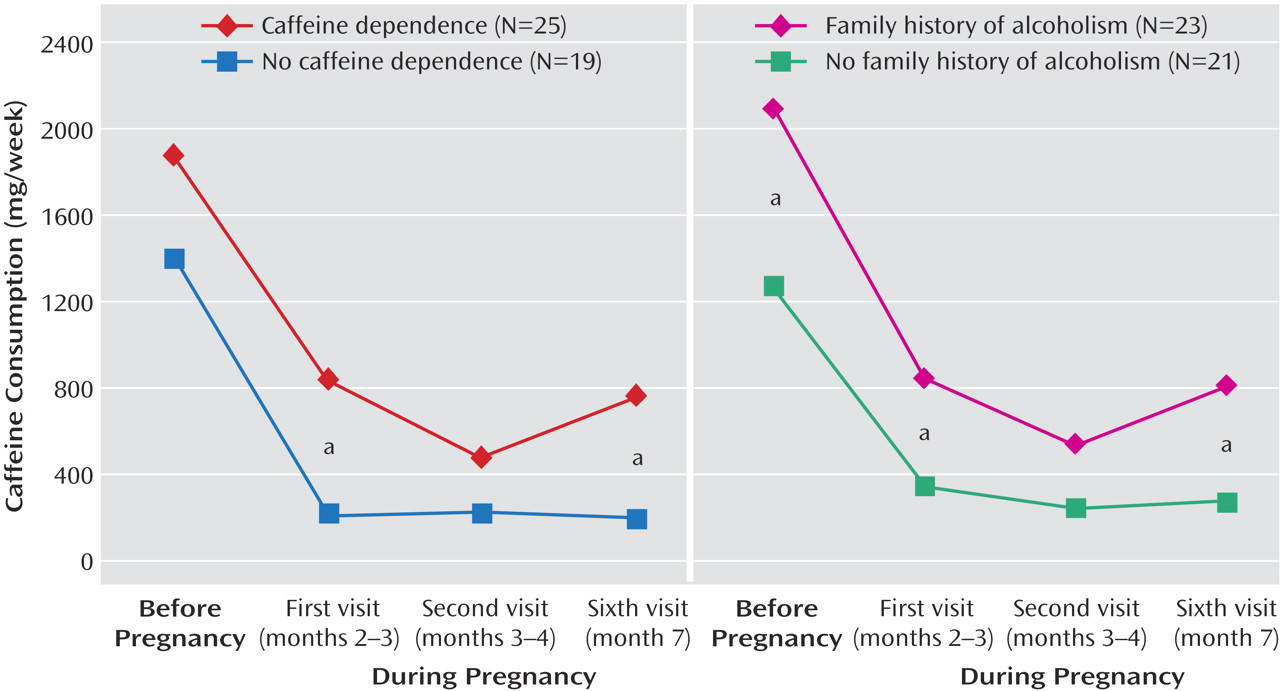
Data on caffeine consumption in women with and without a lifetime diagnosis of caffeine dependence and a family history of alcoholism are summarized in
Figure 1. The ANOVA results suggested effects on caffeine consumption of caffeine dependence (F=6.94, df=1, 40, p<0.01), family history of alcoholism (F=7.69, df=1, 40, p<0.01), time (F=28.32, df=3, 120, p<0.001), and the interaction of caffeine dependence and a family history of alcoholism (F=6.17, df=1, 40, p<0.05). Caffeine consumption (mg/week) was significantly higher in the 6 months before pregnancy awareness (mean=1671 mg/week, SD=1197) than it was at each of the three prenatal visits. Caffeine consumption decreased to 571 mg/week (SD=825) at the time of the first prenatal visit and then decreased further at the second visit, which followed the visit during which subjects received the physician’s advice to eliminate caffeine use (mean=366 mg/week, SD=682). At the sixth prenatal visit (approximately 4 months later), average caffeine consumption was 519 mg/week (SD=838).
At all timepoints caffeine-dependent women consumed more caffeine than those without caffeine dependence; these differences were significant at the first and sixth prenatal visits (
Figure 1, left panel). Similarly, women with a family history of alcoholism consumed more caffeine than those without a family history of alcoholism; these differences were significant before pregnancy and at the first and sixth prenatal visits (
Figure 1, right panel).
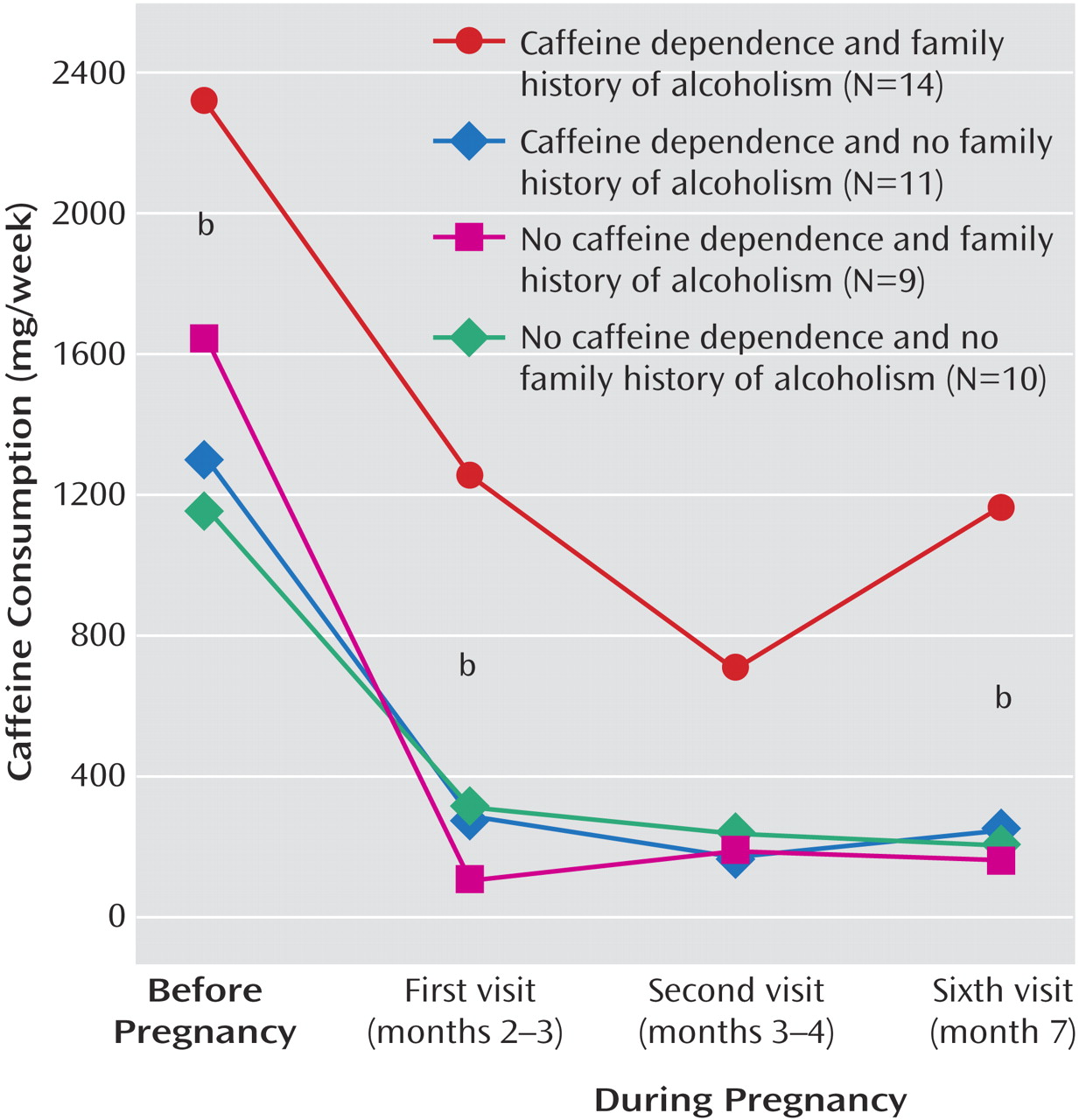
Patterns of caffeine use before pregnancy awareness through the sixth prenatal visit for the four subgroups are summarized in
Figure 2. There were significant group (F=8.25, df=3, 40, p<0.001) and time (F=28.32, df=3, 120, p<0.001) effects. The planned t tests showed that women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism differed in caffeine consumption from the other three groups combined before pregnancy and at the first and sixth prenatal visits. Across the three prenatal visits, women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism consumed 3.4–5.4 times more caffeine than the other subjects. The ANCOVA confirmed these results after adjustment for lifetime history of daily cigarette smoking, DSM-III-R alcohol abuse or dependence, DSM-III-R drug abuse or dependence, and presence of any other DSM-III-R psychiatric diagnosis. The planned t tests with the adjusted means were significant for the period before pregnancy and for the first and sixth prenatal visits.
Inspection of the distribution of caffeine consumption across participants revealed that 50% of the women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism reported consuming more than 2100 mg/week of caffeine (or >300 mg/day) and 43% reported consuming more than 2800 mg/week (or >400 mg/day) at one or more of their prenatal visits. In contrast, no women from any of the other three subgroups reported consuming more than 2100 mg/week of caffeine on any occasion. The difference in the proportion of women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism versus all others with consumption of more than 2100 mg/week during 1 or more weeks was significant (χ2=17.84, df=1, Fisher’s exact p<0.001).
Caffeine Abstinence in Pregnancy
More than one-third (39%, N=17) of the women reported abstinence (i.e., no self-reported use) from caffeine during the week before the first prenatal visit. This abstinence rate increased to 50% (N=22) in the week before the second prenatal visit, with an intermediate rate of 41% (N=17) at the sixth prenatal visit. Almost one-half of the women (48%, N=21) reported consuming some caffeine during the week before all three prenatal visits, and 30% (N=13) reported caffeine abstinence at all three visits.
The rates of abstinence (i.e., no self-reported use during the assessed week) were lower for women with caffeine dependence, compared to women without caffeine dependence, at the first (32% versus 47%), second (44% versus 58%), and sixth (33% versus 46%) prenatal visits, but these differences only approached significance. The rates of abstinence in women with a family history of alcoholism were about one-half of those of women without a family history of alcoholism at the first (26% versus 52%) (χ2=3.20, df=1, p=0.07), second (35% versus 67%) (χ2=4.46, df=1, p=0.04), and sixth (24% versus 57%) (χ2=4.84, df=1, p=0.03) prenatal visits. Concordant with the analysis of amounts of caffeine, the subgroup of women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism had lower rates of abstinence than the other women at the first (14% versus 50%) (χ2=5.14, df=1, Fisher’s exact p=0.04), second (21% versus 63%) (χ2=6.71, df=1, Fisher’s exact p=0.02), and sixth (23% versus 48%) (χ2=2.37, df=1, p=0.18) prenatal visits, although the difference was not significant at the sixth prenatal visit.
Relationship to Histories of Other Substance Use
Women who had a caffeine dependence diagnosis were almost nine times more likely to report a period sometime before pregnancy during which they smoked cigarettes daily, compared to women without the diagnosis (44% versus 5%) (χ2=8.17, df=1, Fisher’s exact p=0.006). Although a family history of alcoholism alone was not related to daily smoking, women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism were more than six times more likely to report a history of daily smoking than were the other women (64% versus 10%) (χ2=14.18, df=1, Fisher’s exact p<0.001), and all three subjects who continued to smoke during pregnancy were in the group with a lifetime diagnosis of caffeine dependence and a family history of alcoholism.
Although presence of a caffeine dependence diagnosis was not related to having a DSM-III-R diagnosis of lifetime alcohol abuse or dependence, women with a family history of alcoholism were more likely than those without a family history of alcoholism to have a diagnosis of lifetime alcohol abuse or dependence (30% versus 5%) (χ2=4.86, df=1, Fisher’s exact p=0.05). Women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism were more than six times more likely to have a DSM-III-R diagnosis of lifetime alcohol abuse or dependence, compared to the other women (43% versus 7%) (χ2=8.40, df=1, Fisher’s exact p=0.008).
Only four subjects had a DSM-III-R diagnosis of lifetime drug abuse or dependence, all involving cannabis. Neither caffeine dependence nor family history of alcoholism was related to lifetime drug abuse or dependence. However, women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism were seven times more likely than the other women to have a DSM-III-R diagnosis of lifetime drug abuse or dependence (21% versus 3%), although the difference was not statistically significant (χ2=3.78, df=1, Fisher’s exact p=0.09).
Caffeine Levels in Saliva
To determine the validity of the self-reported amounts of caffeine consumption, subjects provided saliva samples at each of the three clinic visits. Correlations between the amount of caffeine consumed (mg/week) and the caffeine saliva level (ng/ml) at each of the three timepoints ranged between 0.48 and 0.54 and were significant. Furthermore, the mean caffeine level on occasions when the subjects reported that they abstained from caffeine (mean=124 ng/ml, SD=192) was consistent with levels reported to be associated with abstinence in previous studies
(40,
41) and was significantly lower (p<0.001, t test) than the mean level on occasions when the subjects reported that they were not abstinent (mean=647 ng/ml, SD=936).
Corresponding with the analysis of differences in caffeine intake shown in
Figure 2, the ANOVA of data on caffeine salivary levels showed significant effects of group (F=4.00, df=3, 40, p<0.05) and time (F=5.42, df=2, 80, p<0.01). The women with a lifetime diagnosis of caffeine dependence and a family history of alcoholism had a higher mean caffeine saliva level than all other subjects at the first (mean=464 ng/ml, SD=535, versus mean=107 ng/ml, SD=165), second (mean=860 ng/ml, SD=1212, versus mean=232 ng/ml, SD=310), and sixth (mean=1255 ng/ml, SD=1539, versus mean=330 ng/ml, SD=301) prenatal visits. These differences were significant at the first (t=–2.44, df=42, p<0.05) and sixth (t=–2.23, df=42, p<0.05) prenatal visits.
Discussion
A primary finding of the present study was that women with both a lifetime diagnosis of caffeine dependence and a family history of alcoholism maintained higher levels of caffeine use throughout pregnancy and had lower rates of caffeine abstinence than women without these two characteristics. These relationships were demonstrated with data on self-reported caffeine consumption and by measurement of caffeine levels in saliva samples. The observation that the combination of a history of caffeine dependence and a family history of alcoholism is necessary for the effect suggests that a genetic vulnerability reflected in the family history of alcoholism may be necessary to express the problematic features of caffeine dependence. The suggestion of a genetic component to problematic caffeine use is consistent with previous studies showing a greater co-occurrence of heavy caffeine use, caffeine tolerance, and caffeine withdrawal in monozygotic than in dizygotic twin pairs, with heritabilities of these characteristics between 35% and 77%
(15,
16).
Another intriguing finding is that women with both caffeine dependence and a family history of alcoholism were more likely to have a history of daily cigarette smoking as well as a lifetime diagnosis of alcohol or drug abuse or dependence. These observations extend previous findings that suggested a high co-occurrence between caffeine use, alcoholism, and cigarette smoking
(42); between caffeine use and alcoholism
(5,
17,
18); and between caffeine use and cigarette smoking
(17). Furthermore, twin studies indicated that a common genetic factor (polysubstance use) underlies the use of caffeine, alcohol, and tobacco
(15,
19,
20).
The present study provides valuable new information about a DSM diagnosis of substance dependence applied to caffeine. Three previous studies described a series of case reports of caffeine dependence in adults and adolescents
(5–
7), but they provided no meaningful information on the prevalence of the disorder. The present study showed that more than one-half (57%) of a group of employed and highly educated caffeine-using pregnant women fulfilled the DSM-IV criteria for lifetime substance dependence applied to caffeine, with 45% of the group reporting that they had persistent desire or unsuccessful efforts to cut down or control caffeine use and 43% reporting continued use despite knowledge of a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. The only previous study of the prevalence of caffeine dependence was a random-digit telephone survey conducted in 162 caffeine users in Vermont
(8). In that study, 30% of the sample fulfilled the DSM-IV substance dependence criteria applied to caffeine, 56% endorsed a persistent desire to cut down or quit, and 14% endorsed continued use despite problems.
The present study helps validate the diagnosis of caffeine dependence as a clinically significant phenomenon. Women in this study were instructed by their physician to quit caffeine use during pregnancy, and 98% reported attempting to quit or reduce use. Those who reported failing to eliminate or cut back on caffeine use (predominately women with caffeine dependence and a family history of alcoholism) cited withdrawal symptoms, functional impairment, and craving as reasons they continued to use the substance. Furthermore, 50% of the women who had both caffeine dependence and a family history of alcoholism reported continuing to use caffeine in amounts (>300 mg/day) greater than those thought to be safe during pregnancy
(22,
27,
28).
The present study also contributes new information about the caffeine withdrawal syndrome. Despite the fact that more than 66 experimental and survey studies have characterized various aspects of the caffeine withdrawal syndrome
(43), a diagnosis of caffeine withdrawal is not officially recognized in DSM-IV
(44). In the present study, more than one-half of the women reported withdrawal symptoms when they attempted to eliminate or cut back their caffeine use during pregnancy, with 14% of the overall study group (26% of those reporting withdrawal symptoms) reporting that their caffeine withdrawal symptoms were severe enough to interfere with their performance at work, school, or home. This rate of functional impairment because of caffeine withdrawal is comparable to the 13% rate of clinically significant distress and functional impairment reported in experimental studies of caffeine abstinence in healthy volunteers
(43). The importance of the current study is that it extends the demonstration of functional impairment because of caffeine withdrawal to a medical population.
The small number of subjects (N=44) and the homogeneous nature of the population are limitations of the study. Replication of the study in a larger and more heterogeneous group of subjects would be valuable. There were, however, also strengths in the homogeneity of the study population, which consisted primarily of well-educated, employed, Caucasian pregnant women who reported low current rates of nicotine use and of alcohol or drug problems. As reflected in the low rates of substance use, these women appeared to be quite medically conscientious, with 98% reporting that they attempted to eliminate or reduce caffeine use during pregnancy. The good correspondence between the biological measure of caffeine use and subjects’ self-reported use suggests that the participants were also conscientious in completing the questionnaires and interviews for the study.
The present study has clinical implications for medical management of pregnancy as well as other medical conditions for which caffeine use may be contraindicated. As for pregnancy, the present study shows that the majority of pregnant women spontaneously reduce caffeine intake at time of pregnancy awareness and maintain low levels throughout pregnancy. The study also shows that caffeine-dependent women with a family history of alcoholism had higher levels of caffeine consumption before and throughout pregnancy, compared with women without both characteristics. This subgroup appears to require intervention in addition to instructions from their physician and written materials in order to assure caffeine abstinence.
Finally, the observation that caffeine-dependent women with a family history of alcoholism had higher rates of past cigarette smoking and problematic alcohol use, and possibly other drug use, suggests that the caffeine dependence diagnosis may be a useful clinical and scientific marker for vulnerability to dependence on other drugs of abuse. Because there is little social stigma attached to caffeine use, self-reports may be more accurate for caffeine dependence than for problematic use of alcohol or drugs. Scientifically, it would be valuable if future studies of vulnerability to the more classic forms of drug abuse included measures of caffeine dependence.