Posttraumatic stress disorder (PTSD) is often present in patients with other psychiatric disorders, especially major depression
(1–
8). The National Comorbidity Survey found that 15.2% of subjects with major depressive disorder within the preceding 12 months had comorbid PTSD
(2). In a sample of Bosnian refugees, 53% of those with major depressive disorder had PTSD
(5). However, despite its frequency of occurrence, comorbid PTSD is often unrecognized in psychiatric patients, especially those with more severe illnesses, such as severe depression, bipolar disorder, and psychotic disorders
(9–
18).
The clinical relevance of PTSD comorbidity in depressed patients is largely unknown. Several studies have suggested that PTSD is associated with significant disability, impairment, and cost
(4,
19–29). When PTSD is comorbid with another psychiatric illness, these effects may be even greater
(2,
5,
6,
13,
25,
28,
30–33). However, few studies have specifically compared psychiatric patients with and without PTSD, and these studies have been limited to relatively small sample sizes. Also, since most studies have not controlled for total number of psychiatric diagnoses, it is possible that correlates of PTSD comorbidity merely reflect nonspecific correlates of increased psychiatric burden. Finally, the vast majority of studies to date have focused on general community samples, veterans, or refugee populations; few have systematically assessed the specific effects of PTSD comorbidity in a severely mentally ill population, where PTSD comorbidity may be more prevalent but underdiagnosed
(9).
To better understand the impact of PTSD comorbidity in adult patients with severe mental illness, we performed an extensive, retrospective chart review of severely depressed psychiatric inpatients with and without comorbid PTSD. It is important to note that we were most interested in the presence of clinical comorbidity (as opposed to epidemiological comorbidity; see Kraemer
[34] for a review); i.e., we intended to compare short-term clinical outcome (i.e., change in clinical status during psychiatric hospitalization) in depressed patients with and without PTSD at time of admission. The purpose of these exploratory analyses was to determine what differences, if any, in short-term clinical outcome were associated with PTSD comorbidity. It was presumed that any identified differences would help clarify the clinical importance of recognizing comorbid PTSD in severely depressed patients. Recognizing the limitations of a retrospective, case-control design, we carefully matched subjects in each group by age, gender, race/ethnicity, year of hospitalization, primary depressive diagnosis, and presence of substance use disorder diagnosis at time of admission. To better assess the specific associations of PTSD (as opposed to overall increased psychiatric burden), we used total number of psychiatric diagnoses as a covariate in our analyses. We hypothesized that the short-term clinical outcome of depressed patients with PTSD would differ from that of depressed patients without PTSD.
Method
Sample
The initial study sample included all patients psychiatrically hospitalized between 1995 and 2000 at Harborview Medical Center in Seattle, Wash. All patients with a diagnosis of depression (including major depressive disorder, bipolar disorder [depressed phase], dysthymic disorder, depression not otherwise specified, or adjustment disorder with depressed mood) were first selected. All patients with a diagnosis of PTSD were then identified. Depressed patients with PTSD were matched with depressed patients without PTSD, selected from the original sample of depressed patients, according to age, gender, race/ethnicity (white versus nonwhite), year of admission (1995–1996, 1997–1998, 1999–2000), primary depression diagnosis (major depressive disorder, bipolar disorder [depressed phase], or other [dysthymic disorder, depression not otherwise specified, or adjustment disorder with depressed mood]), and current substance abuse or dependence (i.e., present at time of admission). Patients admitted on a planned basis as part of a structured program for patients with extremely high utilization of inpatient services were excluded. The study procedure was approved by the Institutional Review Board of the University of Washington Medical School and Harborview Medical Center.
Data Collection/Assessments
For all patients, a board-certified University of Washington faculty psychiatrist performed a standardized assessment battery within 24 hours of admission and discharge. This battery
(35) included a demographic questionnaire, a semistructured psychiatric interview, the 23-item behaviorally anchored Psychiatric Symptom Assessment Scale
(36), which includes domains similar to the Brief Psychiatric Rating Scale, and the DSM-IV Global Assessment of Functioning (GAF) scale. The semistructured diagnostic interview identified axis I and select axis II disorders (borderline personality disorder and antisocial personality disorder) using a symptom checklist based on DSM-IV criteria. This assessment battery has been shown to be reliable and valid for use with psychiatric inpatients in our setting
(35). An extensive chart review was performed to confirm the presence of diagnostic criteria and the absence of any exclusionary criteria for the major diagnoses considered in this study (depression and PTSD). An automated hospital database was used to obtain length of stay and discharge status (regular or against medical advice).
Individual items on the Psychiatric Symptom Assessment Scale ranged from 0 (no severity) to 6 (most severe); the total score could range from 0 to 138. Cronbach’s alpha for internal consistency reliability of the total Psychiatric Symptom Assessment Scale was 0.74 at admission and 0.78 at discharge. To assess depression severity, the scores of six Psychiatric Symptom Assessment Scale items associated with depression (withdrawal, motor retardation, helplessness/hopelessness, suicidality, depressed mood, blunted affect) were combined into a single score. To account for potential missing values on some items, the mean of the summed scores was calculated. In a similar fashion, an anxiety subscore was calculated by averaging the anxious mood, tension, excitement, and hyperactivity items into a single score, and a hostility subscore was calculated by averaging the uncooperativeness and hostility/aggression items into a single score. Factor analyses confirmed these subscales. Items in the depression subscore had an internal consistency reliability of 0.77 at admission and 0.78 at discharge. Items in the anxiety subscore had an internal consistency reliability of 0.73 at admission and 0.69 at discharge. Items in the hostility subscale had an internal consistency reliability of 0.73 at admission and 0.79 at discharge.
The assessment battery used in this study was not designed to establish the severity or time of onset of each psychiatric disorder diagnosed, nor was the source of PTSD clearly documented in each patient. However, to address the important question of how chronicity and type of PTSD might affect these results, a more detailed chart review was performed on a random sample of 178 (30%) of patients with depression and PTSD. In this subset, nine patients (5.1%) had acute PTSD that co-occurred with, or was preceded by, depressive symptoms; thus, approximately 95% of patients with PTSD in this study had chronic PTSD that preceded the current depression. Given the small proportion of patients with acute PTSD, we did not extend this chart review nor did we perform separate analyses on patients with acute PTSD. Additionally, among the 37 veterans with PTSD (6% of the PTSD sample), only 18 (3% of the PTSD sample) had combat-related PTSD. Given this small proportion, we did not compare results between PTSD subjects with or without combat trauma.
Statistical Analyses
For demographic comparisons, chi-square tests with a continuity correction were performed for categorical variables and independent sample t tests were used for age. For clinical severity analyses, the two groups were compared at admission and discharge on total Psychiatric Symptom Assessment Scale score; depression, anxiety, and hostility subscale scores; and GAF score. Logistic regression was used for categorical variables, and analysis of covariance was used for continuous variables. Number of psychiatric diagnoses was used as a covariate for all analyses. Substance abuse/dependence was not considered a primary or comorbid psychiatric diagnosis, since this was used as a primary matching variable. Admission values were used as covariates in analyses of discharge variables.
Characteristics of the hospital stay were analyzed by comparing the two groups on likelihood of involuntary hospitalization, likelihood of discharge against medical advice, and length of stay. Length of stay analyses used number of diagnoses and admission clinical severity (total Psychiatric Symptom Assessment Scale score) as covariates. Separate comparisons were made for patients admitted voluntarily and involuntarily. Also, patients discharged against medical advice were excluded from these analyses to decrease bias from unexpectedly short hospital stays.
All statistical analyses were two-tailed. Given the exploratory nature of these analyses, a significance level of p=0.01, without correction for multiple comparisons, was used.
Results
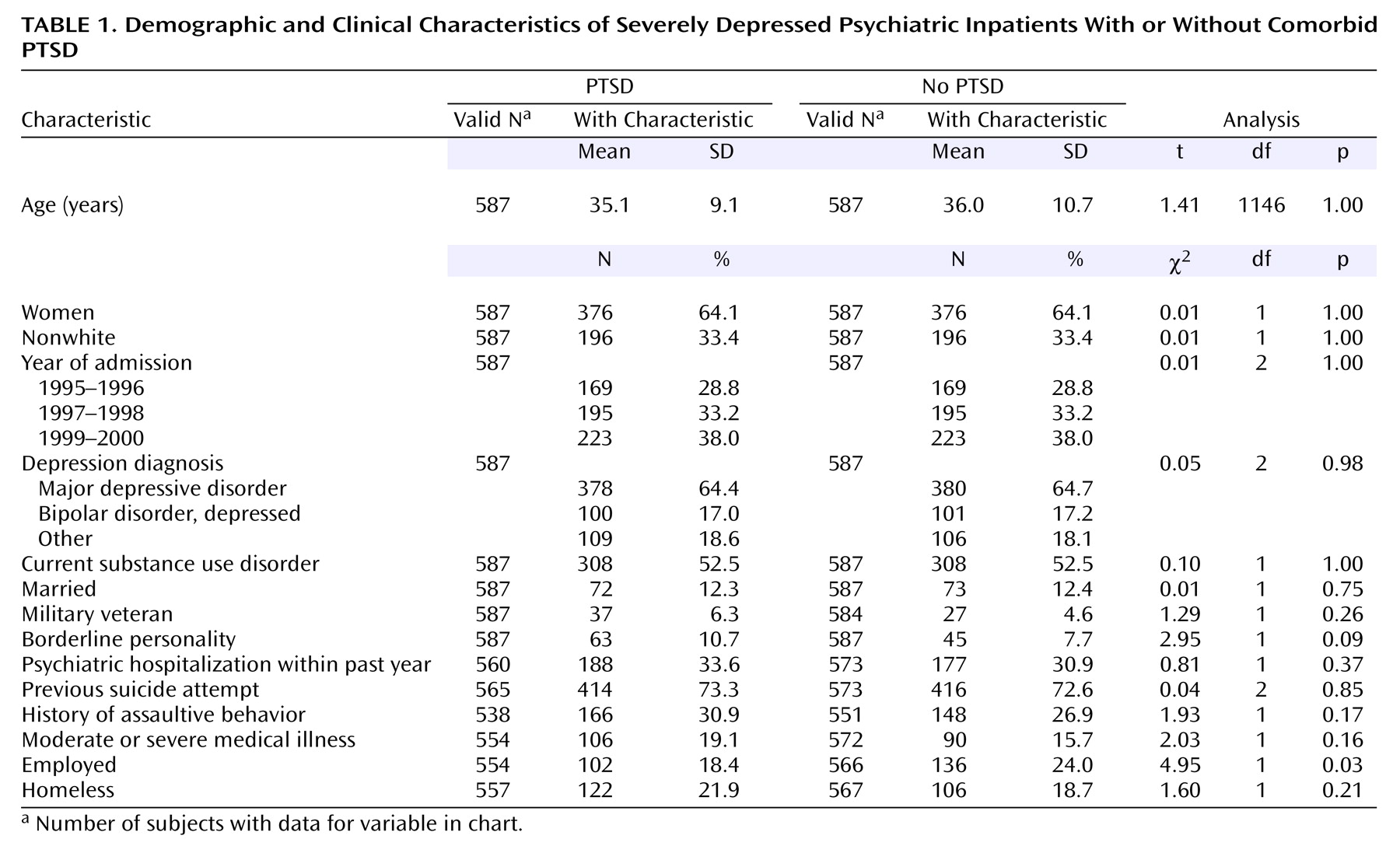
A total of 4,182 psychiatrically hospitalized patients with depression were initially identified. Within this group, 587 patients (14%) with comorbid PTSD were matched with 587 depressed patients without PTSD to provide the study sample. Patients were matched in terms of gender, race/ethnicity, age, year of admission, depression diagnosis, and current substance abuse/dependence. There were no significant differences between depressed patients with or without PTSD on demographic variables (
Table 1), although there was a tendency for fewer patients with PTSD to be employed.
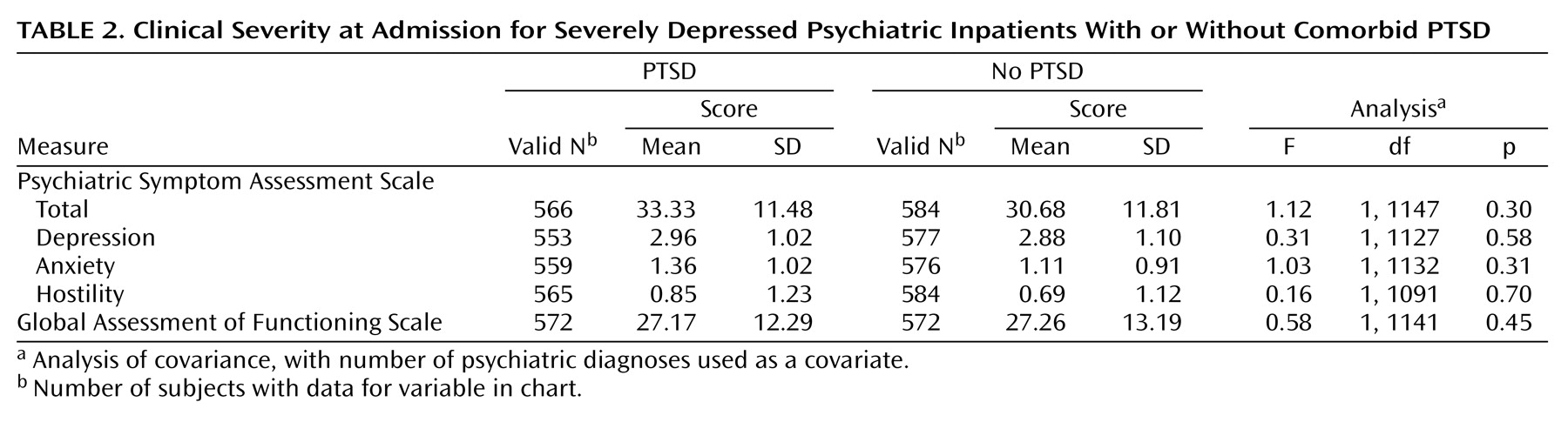
On admission, there were no differences between the two groups on clinical severity (
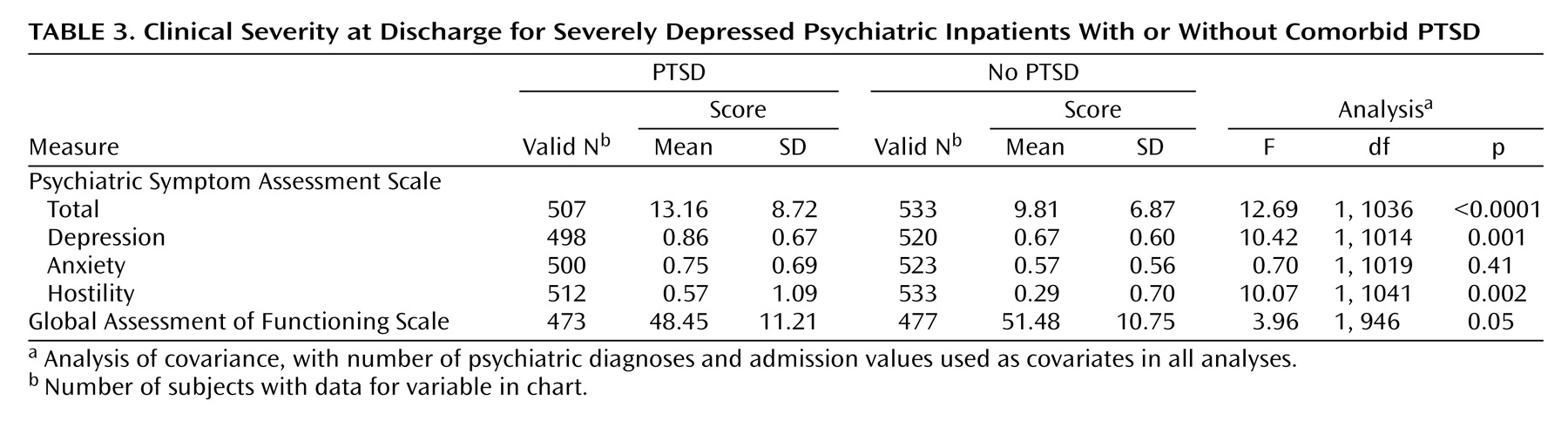
Table 2). However, at discharge the PTSD group had a significantly higher total score on the Psychiatric Symptom Assessment Scale and higher scores on the depression and hostility subscales than did patients without PTSD (
Table 3). There also tended to be lower discharge GAF scores in the PTSD group. Because differences in length of stay and rates of discharge against medical advice could account for differences in discharge clinical severity, we performed post hoc analyses covarying for these variables. Covarying for length of stay did not alter the statistical significance of any of the original findings. Among patients discharged regularly (i.e., not against medical advice), patients with PTSD continued to show higher total scores on the Psychiatric Symptom Assessment Scale (F=9.09, df=1, 982, p=0.003) and higher depression subscale scores (F=8.52, df=1, 961, p=0.004) than patients without PTSD. The hostility subscale score remained higher, but not significantly so (F=2.96, df=1, 985, p<0.09). There continued to be no significant differences in anxiety subscale scores or discharge GAF scores. Given the small proportion of patients discharged against medical advice (<7% of total sample), we did not perform post hoc analyses in this group.
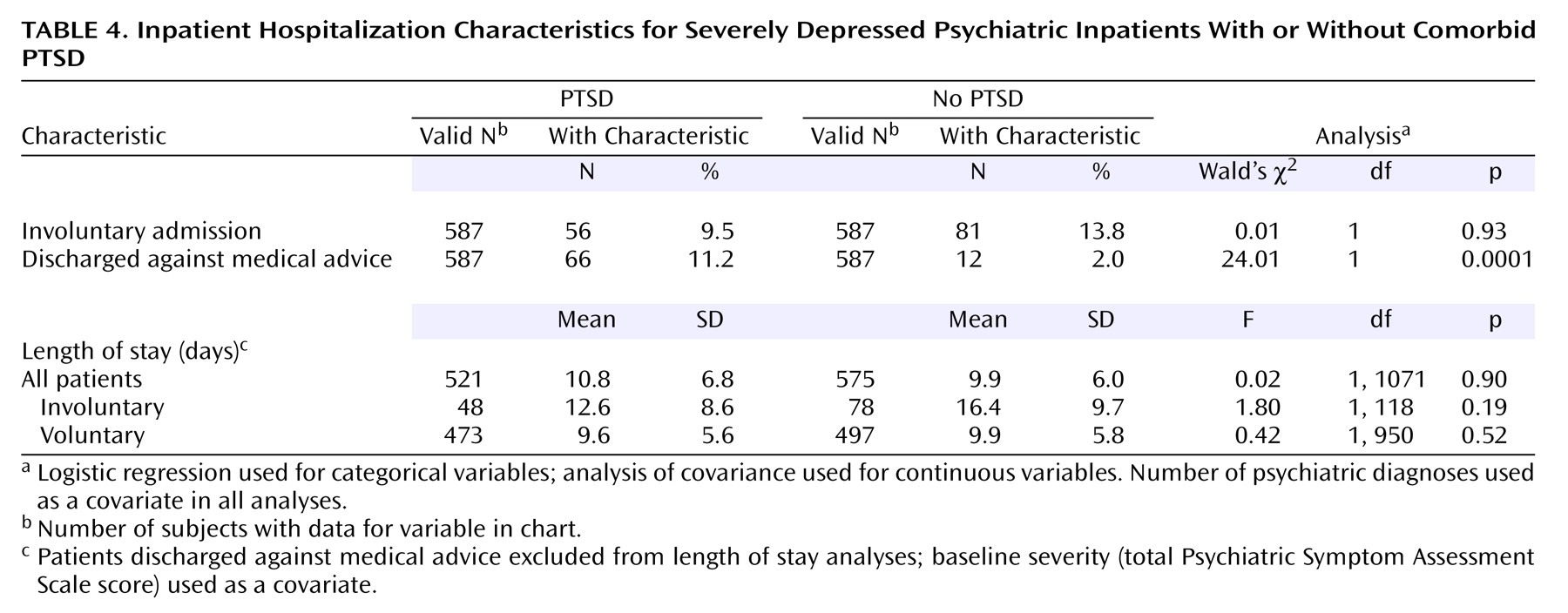
Length of hospitalization and the proportion of patients hospitalized involuntarily did not differ significantly between the groups (
Table 4). However, likelihood of discharge against medical advice was significantly higher in the PTSD group, with an odds ratio of 6.10 (95% CI=2.96–12.57). When separate analyses for likelihood of discharge against medical advice were done for voluntary (N=67 [with PTSD: N=58, no PTSD: N=9]) and involuntary (N=11 [with PTSD: N=8, no PTSD: N=3]) admission patients, this difference remained significant for voluntary admission patients (odds ratio=7.26, 95% CI=3.22–16.35; Wald’s χ
2=22.92, df=1, p<0.0001) but not involuntary admission patients (odds ratio=2.38, 95% CI=0.44–12.95; Wald’s χ
2=1.01, df=1, p<0.32). However, the small sample size of involuntary patients discharged against medical advice limits the power of this comparison.
While our assessment battery was not designed to obtain data on the chronicity or source of PTSD, these features were investigated in a subset of the depressed patients with PTSD. Of 178 patients (30% of PTSD sample), nine (5.1%) had acute PTSD, 53 (29.8%) had chronic PTSD related to childhood trauma, 48 (27.0%) had chronic PTSD related to multiple traumas (often including childhood trauma), and 39 (21.9%) had chronic PTSD related to adult trauma. For 29 patients with chronic PTSD (16.3%), the source of the PTSD could not be identified from the chart review.
Discussion
To date, this is one of the largest studies of PTSD comorbidity in depressed patients and one of the first to systematically investigate the effects of PTSD comorbidity on clinical outcome in a severely depressed, hospitalized population. In this study, depressed inpatients with comorbid PTSD were more psychiatrically impaired, more depressed, and more hostile at time of discharge than depressed patients without PTSD. Also, hospitalized patients with depression and PTSD were much more likely to be discharged against medical advice.
These results are consistent with previous reports that have suggested that psychiatric patients with comorbid PTSD are more symptomatic and more impaired than individuals without PTSD comorbidity
(2,
5,
6,
13,
19,
20,
25,
28,
30–33). It is important to note that in this study, such effects were noted only at discharge (versus admission), suggesting that hospitalized, depressed patients with PTSD have poorer short-term clinical outcomes than patients without PTSD. Whether these effects are specific to PTSD or related to overall psychiatric impairment has been questioned
(37). Since overall burden of psychiatric illness was entered into analyses as a covariate, our results indicate that PTSD comorbidity is independently associated with poorer clinical outcome in hospitalized, depressed patients.
One of the most striking findings in this study is the greatly increased likelihood of discharge against medical advice among patients with comorbid PTSD. Depressed patients with PTSD were more than six times as likely to leave the hospital against medical advice than those without PTSD. This finding was present even in the absence of differences between the two groups on a number of variables known to predict discharge against medical advice (age, gender, race, substance abuse/dependence, severity of medical comorbidity)
(38). While a previous study found that primary psychiatric diagnosis did not predict discharge against medical advice
(38), our results indicate that PTSD comorbidity may have specific and profound effects on the likelihood of discharge against medical advice in depressed patients. This finding adds to growing evidence that patients with PTSD may be particularly difficult to engage in mental health treatment
(19,
39–42) and has important implications for treatment planning for psychiatric patients with comorbid PTSD.
In this study, hospitalized depressed patients with PTSD did not differ significantly from depressed patients without PTSD on a number of demographic variables, nor was the presence of PTSD comorbidity associated with differences in clinical severity on admission. In particular, we did not replicate findings reported by other groups that PTSD comorbidity is associated with increased suicidality
(2,
13,
25,
30). However, the similarity in clinical presentation at admission, including history of suicide attempts, between hospitalized depressed patients with and without PTSD likely represents a threshold effect for admission in a population of severely ill patients already at high risk for suicide.
It is interesting that depressed patients with comorbid PTSD did not demonstrate higher anxiety at admission or discharge than did depressed patients without PTSD. The absence of a difference in anxiety in this sample is somewhat surprising, given that patients were stratified by presence or absence of a comorbid anxiety disorder (i.e., PTSD). A possible explanation of this finding is that patients with PTSD in this study (most of whom had very chronic PTSD that preceded the diagnosis of depression) overall were more likely to demonstrate withdrawal and avoidance (perhaps demonstrated by the higher rate of discharge against medical advice) and less likely to show obviously increased anxiety (as measured by the anxious mood, tension, excitement, and hyperactivity items of the Psychiatric Symptom Assessment Scale).
Taken together, these results strongly suggest that for severely depressed patients, comorbid PTSD is associated with a poorer outcome during psychiatric hospitalization, including a greater likelihood for discharge against medical advice. This emphasizes the importance of recognizing PTSD comorbidity in such patients and raises the question of whether depressed patients with comorbid PTSD might benefit from more specialized treatment during psychiatric hospitalization.
Certain limitations must be considered when interpreting these results. Most important, diagnoses were not obtained through the use of a fully structured diagnostic instrument such as the Structured Clinical Interview for DSM-IV Axis I Disorders
(43). However, our goal in this study was to include data from a large number of severely ill, hospitalized patients in order to generate a sample size that would allow for analyses not possible in previous smaller studies. To do this, we included naturalistic data collected on all patients hospitalized over a 6-year period, using the assessment battery described earlier. The semistructured diagnostic interview used in this battery has been shown to be valid in other settings and reliable for use with psychiatric inpatients in our setting
(35,
44). In addition, an extensive chart review was used to confirm presence or absence of PTSD and depression diagnoses in the study sample. While the likelihood of false positives is potentially higher with this approach, the accuracy of diagnoses in this study is likely to be greater given the high prevalence of mood disorders and PTSD in an inpatient setting. Since PTSD is commonly underdiagnosed, it is certainly possible that some depressed patients may have been incorrectly categorized as not having comorbid PTSD.
With this data set, we were not able to control for type and number of traumatic experiences or for duration of PTSD (although a subsample analysis suggested about 95% of patients had chronic PTSD that preceded the current depression). The severity of PTSD was also not consistently tracked, so the effects of PTSD severity on the outcome measures in this study are unknown. Also, the nature of the data collection did not allow for meaningful analysis of a number of health care utilization measures of interest (e.g., number of hospitalizations or frequency of emergency room visits), since a bias toward patients admitted earlier would have been present.
Retrospective chart reviews may be limited by data missing because of inadequate documentation. Missing data were encountered in this study and account for the variability in sample size among the different comparisons. It is important to note that there were no significant differences in the amount of missing data between the two groups for these analyses. Also, it should again be noted that this retrospective chart review allowed for the collection of an extensive dataset on a very large sample of patients.
Given the nature of the data used in this study, a case/control design was employed for analyses. Case/control studies may be limited by lack of randomization resulting in systematic differences between groups. To limit this, we employed extensive matching of depressed patients with and without PTSD. Accordingly, demographic comparisons suggested the groups were quite similar on a number of variables that could have confounded the results (e.g., age, gender, substance abuse/dependence, primary depressive diagnosis, year of admission) (
Table 1).
Despite these limitations, these results clearly show that comorbid PTSD is associated with important and independent differences in short-term clinical outcome, especially rate of discharge against medical advice, in patients with severe depression. These findings strongly suggest that identifying PTSD comorbidity is relevant to the care of psychiatric inpatients with depressive illness. A next step will be to investigate whether identification and treatment of PTSD in these patients can ameliorate the effects of PTSD comorbidity observed in this hospitalized cohort of severely depressed patients.