Managed care organizations and insurance plans are increasingly adopting step therapy in an effort to contain costs by steering patients away from more costly pharmacotherapies (
1). Step therapy requires a member to try a first-line medication within a drug class, usually a generic alternative, prior to receiving coverage for a second-line agent, usually a branded product (
2). However, step therapy is not the same as generic substitution, since it may require different types of medications to be tried other than just generic substitutes for the same medication in brand form. Currently, most pharmacy benefit managers that implement step therapy allow patients to use a second-line agent if insurance claims are found in the recent past for the first-line agent or if members obtained a prescription for the second-line drug in the recent past (
2). If a prescription for a second-line agent is rejected, members may have their healthcare provider change the prescription to the first-line agent or submit a request for coverage of the second-line agent through a prior authorization (
2).
Although step therapy plans for antidepressant medications have become prevalent, there has been little research examining their effects (
1). Prior research has focused on the effects of step therapy on prescription drug utilization and spending (
3,
4). In contrast, the present study focuses on the effects of step therapy on medication and nonmedication medical care utilization and spending. Specifically, this study aims to provide understanding of the association between step therapy implementation and changes in prescription drug, outpatient, inpatient, and emergency room utilization and spending.
Method
The data source for the study was the Thomson Reuters MarketScan Research Database, which represents the healthcare experience of enrollees in employer-sponsored health plans in the United States. The database, in its entirety, represents more than 60 employers. Thomson Reuters account managers were surveyed to determine whether any of their employer clients either had recently implemented step therapy (i.e., in 2003 and 2004) or did not have step therapy and would be willing to participate anonymously in the study. As an additional requirement, the step therapy program had to be implemented equally across all benefit plans available to an enrollee. Step therapy could not be selected or deselected by the individual enrollee, in order to reduce the likelihood of selection bias. Two firms had recently implemented step therapy programs and were identified as the treatment group. Two employers that did not have a program in effect during the same time were identified as the comparison group. No other employer groups that might have been eligible to participate in the study were identified.
A step therapy program was implemented at the beginning of 2003 in one plan and on April 1, 2004, in the other plan. Both step therapy programs were administered by the same pharmacy benefit manager. The present analysis focuses on step therapy programs for antidepressant medications because these are among the most commonly used medications (
5).
The sample was limited to employees, and their dependents, of the selected employers (step therapy and comparison groups) who were continuously enrolled from 2003 through the third quarter of 2006, were under 65 years of age, and were not Medicare eligible. An analytic file was created using a panel data (repeated-measures) framework with one observation each quarter for each individual. Each enrollee in the analytic file had 15 observations (i.e., quarters of data). The total sample consisted of 269,561 enrollees. Of these, 66,308 were enrolled in step therapy plans and 203,253 were enrolled in comparison plans. We also focused on the subset of enrollees in each plan who were being treated with any antidepressant medication (N=60,796). Of these, 15,552 were in step therapy plans and 45,244 were in comparison plans.
The dependent variables were prescription drug and medical costs and utilization. The following quarterly utilization measures were examined for individuals being treated with antidepressant medication: the number of antidepressant days supplied (within the time period covered by the quarter), the number of prescriptions filled, the number of all disease- (i.e., somatic and mental health conditions combined) and mental health-related outpatient office visits, the number of all disease- and mental health-related emergency room visits, and the number of all disease- and mental health-related inpatient admissions. Mental health-related utilization was defined as services used for a primary psychiatric diagnosis (ICD-9-CM, 290–319). Four spending measures for antidepressant users were examined: outpatient prescription drug costs, emergency room costs, inpatient medical (admissions) costs, and outpatient medical (nondrug) costs. Expenditures were defined as the total amount reimbursed to providers from all sources of payment, including the health plan, the patient, and any third party (coordination of benefits amount). One utilization measure was examined for all enrollees: antidepressant days supplied.
Statistics were performed using UNIX SAS, Version 9.01 (SAS Institute, Inc., Cary, N.C.), and Stata 9.0 for Windows (StataCorp, LP, College Station, Tex.). Chi-square and Student's t tests were computed to compare demographic and clinical characteristics as well as outcome variables between the step therapy and comparison groups after step therapy had been implemented.
The general model specification equation was as follows (where “i” represents person and “t” represents time in quarters): Y=g(a0+β1Stepit+β2AfterStepit+b3TimeStepit+β4Quartert+β5Quarter2t+β6Demit+β7*Clinicalit)
The explanatory variables were defined as follows: Y=medical care utilization or expenditure measure; Step=a 0/1 dummy variable that equals 1 if the employer instituted step therapy at any time during the study period and equals 0 otherwise; AfterStep=a 0/1 dummy variable that equals 1 after the employer instituted step therapy and equals 0 otherwise; TimeStep=a numeric counter measuring the number of quarters since the step therapy program began (i.e.,
1,
2,
3); Quarter=a “time trend” variable to capture the linear utilization and spending trends common to both the step therapy and comparison groups, with the first quarter of 2003 coded as 1 and the third quarter of 2006 coded as 15. Quadratic trends were captured in the Quarter
2 variable; Dem=demographic characteristics, including age, gender, median income in the patient's residential zip code, and percent of college graduates in the patient's residential zip code (from the U.S. Census); Clinical=clinical characteristics, including the number of ICD-9-CM codes and Deyo-Charlson Comorbidity Index ratings, which were measured as lagged variables over a 1-year period prior to the time the outcome was measured.
Multivariate generalized estimating equation models were used to determine the effects of step therapy on spending and utilization while controlling for important covariates. Generalized estimating equation models were used because they adjust the standard errors for the effect of repeated measures by patient and are flexible enough to allow for different distributions of the dependent variables, such as skewed and binary distributions and distributions with a concentration of zero values (
6). Utilization variables, representing counts of each type of service, were estimated with a negative binomial distribution and a log link. Expenditures were estimated using a gamma distribution with a log link.
The effects of step therapy are captured in the coefficients of the AfterStep and TimeStep variables. The first variable (After-Step) captures the immediate and static effects of step therapy, and the second (TimeStep) captures the time varying effects in each quarter after the plan was implemented. In order to estimate the full magnitude of the effects of step therapy on the outcome measures (as expressed in these two coefficients), we calculated a nonlinear prediction (predictnl in Stata) at the mean of each control variable (
7).
Discussion
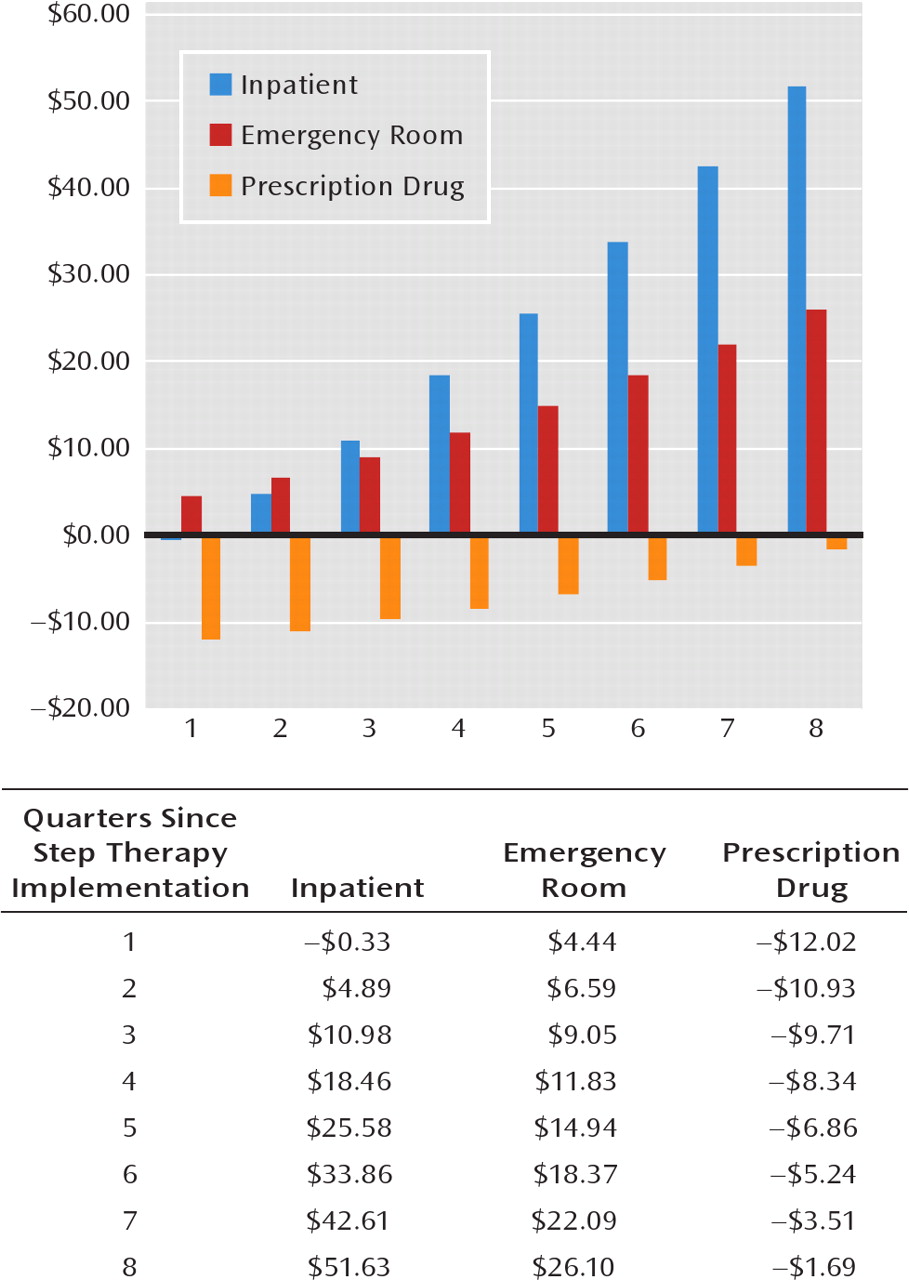
Prior studies have found that antidepressant step therapy increases the use of generic medications and reduces pharmaceutical expenditures (
3). This study expands the research on step therapy by examining its impact on medical care utilization and expenditures in addition to pharmaceutical utilization and expenditures. We found that while step therapy led to some medication cost savings in the short run, the number of antidepressant days supplied declined after step therapy was implemented and inpatient and emergency room admissions and costs increased postimplementation, relative to the comparison plans. Drug savings were offset by higher medical spending, resulting in no net change in total spending.
Step therapy has become a common aspect of private health insurance plans. In theory, if step 1 (preferred) medications were perfect substitutes for step 2 medications and selecting the preferred drug was administratively seamless, then one would anticipate that step therapy would lower medication costs with no negative effects on drug use patterns, outcomes, or expenditures.
However, step therapy may have unintended consequences. Rather than shifting patients to generic or other preferred medications, step therapy may deter patients from filling prescriptions all together. This may happen for several reasons. Physicians may generally not know that patients only have coverage for step 1 medications and may still be prescribing step 2 medications. Patients may only find out about their limited coverage for step 2 medications once they try to obtain a prescription from a pharmacy and might be deterred by the time and administrative constraints of obtaining a prescription for a step 1 medication or an exemption for a step 2 medication. As a result, patients might decide not to fill the prescription at all.
Some prior studies support this scenario. During the first 4 months of the Medicare prescription drug benefit, a study of dual-eligible psychiatric patients found that among patients with “fail first” or step therapy policies, 78% reported an access problem, a much greater percentage of access problems relative to those without step therapy policy (
8). A study of Medicaid prior authorization and step therapy plans for antipsychotic medications found that the programs resulted in greater medication discontinuation (
9).
In another study, Motheral et al. (
4) surveyed plan members who had been subject to step therapy edits (i.e., denied prescriptions for a step 2 medication) for proton pump inhibitors, selective serotonin reuptake inhibitors, and nonsteroidal antiinfiammatory drugs. They found that nearly 17% received no medication and another 10% only received a sample or an over-the-counter alternative. Finally, a study using the same employers we utilized in the present study, but focused on antihypertensives versus antidepressants, found that step therapy resulted in a decline in the number of antihypertensive medications supplied and an increase in inpatient and emergency room utilization (
10).
A clear direction for future research is to understand in more depth the nature of the potential administrative barriers that step therapy and fail first policies are creating that may be preventing people from filling needed prescriptions. For example, private and public third-party payers may need to understand how quickly and easily patients can obtain provider authorization for step 2 medications. Additionally, there is a need to understand how well “step edits,” which rely on claims history to determine prior use of step 1 and 2 medications, are accurately capturing prior use or might be missing claims, for example, because a patient recently switched plans. Finally, research and perhaps more education is needed to explain to patients the direction that they can take when they are denied a step 2 medication.
Another possible hypothesis as to why step therapy participants experienced lower days supplied and more hospitalizations and emergency room visits is that the step 1 medications were less efficacious or were associated with more side effects than the step 2 medications. The research to support efficacy differences among anti-depressants is limited, although most clinical trials are not conducted with the power to test noninferiority and may not capture modest differences in efficacy (
11). Moreover, comprehensive reviews find that antidepressants cannot be considered identical drugs, and evidence supports differences with respect to onset of action, side effects, and effects on health-related quality of life (e.g., sexual functioning) (
11). It may be true that despite limited differences in average efficacy, when physicians are provided with a range of treatment options, they select antidepressants for particular patients while taking into account the patient's treatment history as well as side effect concerns, which in turn promotes adherence and hence efficacy.
One policy implication of this line of research is that programs that are structured to only address pharmaceutical utilization in isolation from medical utilization may be operating at cross purposes. For example, pharmaceutical benefits that are managed by pharmaceutical benefit managers who are operating under incentives to reduce pharmaceutical costs and only view pharmaceutical claims may not have the motivation or information necessary to consider the impact of their policies on medical care expenditures. In the areas of copayment design, recognition of this type of misalignment because of silos in benefit management has led to the idea of a value-based insurance design, where copayments are adjusted to encourage appropriate use of medications, such as better adherence for patients with diabetes (
12).
Our study should be understood in light of its strengths and limitations. Step therapy is implemented in various ways by different pharmacy benefit managers and health plans. By its nature, it must be examined through a natural experiment, which was done in this study. Although we employed a strong pre/post design, estimating the common effects of step therapy plans instituted at two different points in time relative to a contemporaneous comparison group, it is possible that studies of other step therapy systems would yield different results. In particular, it may be that the comparison and step therapy plans were starting at different baselines, which influenced the relative change after step therapy. Additionally, this study examined utilization and cost outcomes, and other outcome measures, such as psychiatric symptoms and functioning, are not captured in insurance claims but are important to evaluate. Finally, while the study examined differences in expenditures and utilization, it did not decompose changes in expenditures into changes in price and changes in utilization. Such an analysis would further inform the effect of step therapy. Clearly, there is a need for additional research to understand both the strengths and limitations of step therapy as a cost saving tool.