Suicide is a major global social and public health problem. It is commonly associated with depressive disorder, which carries a 2%–12% lifetime risk of dying by suicide (
1). Suicide attempts, typically defined as self-destructive acts with some intent to end life (
2), are strongly correlated with major depressive disorder (
2), and a history of attempts is the strongest predictor of eventual completed suicide (
3). Thus, suicide attempts represent an important intervention point, and understanding their neural correlates may inform this intervention. However, the neurobiology of suicide attempts in depression is largely unknown. Despite some inconsistencies among reports, meta-analysis has found suicidal behaviors to be associated with polymorphisms in the gene for tryptophan hydroxylase 1 and the serotonin (5-HT) transporter gene (
4). Both genes mediate serotonin function, and suicide attempters also show serotonin-related abnormalities, such as decreased CSF 5-hydroxyindoleacetic acid, decreased serum serotonin, reduced serotonin transporter numbers in the prefrontal cortex, and upregulation of postsynaptic 5-HT1A and 5-HT2A receptors (
5). Structural neuroimaging in depressed suicide attempters has shown periventricular white matter hyperintensities (
6), while suicide risk in unipolar depression is related to basal ganglia gray matter hyperintensities (
7). Thus, there are biological differences between patients who do and do not attempt suicide. However, they are poor predictors of individual suicide risk (
6).
Although the studies of suicidal behaviors published so far have focused on gray matter differences, several lines of evidence suggest that white matter may also be affected. First, gray matter differences between suicidal and nonsuicidal depression are likely to be the result of or lead to white matter differences over time (
8). Second, abnormalities in white matter (
9,
10) and functional integration (
11) have been reliably reported in patients with major depressive disorder. It is therefore possible that these abnormalities are more pronounced in suicidal depression relative to nonsuicidal depression. Third, the 5-HT transporter gene, which mediates suicidal behavior, has been shown to affect both gray and white matter (
12,
13). Thus, it is plausible that genetic vulnerability to suicidal behavior may result in both gray and white matter differences between suicidal and nonsuicidal depression. Advances in high-field magnetic resonance neuroimaging provide new opportunities to characterize both gray and white matter alterations in suicidal behavior.
Diffusion tensor imaging combines a conventional magnetic resonance imaging (MRI) sequence with additional magnetic field gradients to quantify water diffusion; namely, fractional anisotropy, the degree to which diffusion is directionally hindered, reflects the integrity of the white matter tracts. Diffusion tensor imaging data can be quantified by either voxel-based analysis or region-of-interest methods. Whole-brain voxel-based analysis investigates region-specific changes in gray and white matter by averaging results, spatially normalizing (coregistering) brain images across subjects, and performing statistical tests at each voxel. It is highly reproducible, user-independent (for a specific algorithm), and can explore differences across the entire brain without anatomically specific prior hypotheses (
14). In contrast, region-of-interest methods, often more sensitive, are used for testing anatomically specific hypotheses (
14) and are usually applied in the original image space. Finally, voxel-based morphometry is a fully automated whole-brain image analysis technique involving voxel-wise comparison of segmented gray and white matter (
15).
The aim of the present study was to use diffusion tensor imaging and optimized voxel-based morphometry with a 3.0 Tesla scanner to characterize microstructure abnormalities in individuals with major depressive disorder with and without a history of suicide attempts. We hypothesized that gray and white matter reductions would be specifically associated with suicide attempt in major depressive disorder, which would provide insight into the neurobiology of suicidal behavior and inform the possible early identification of individuals at high risk of suicide.
Discussion
We have previously demonstrated differences in brain microstructure and perfusion between the subclasses of refractory depressive disorder and nonrefractory depressive disorder (
22,
23). In the present study, we have extended this by using the magnetic resonance technique of diffusion tensor imaging to compare patients with major depressive disorder (but no other axis I psychiatric comorbidities) with and without a history of suicide attempts and healthy comparison subjects.
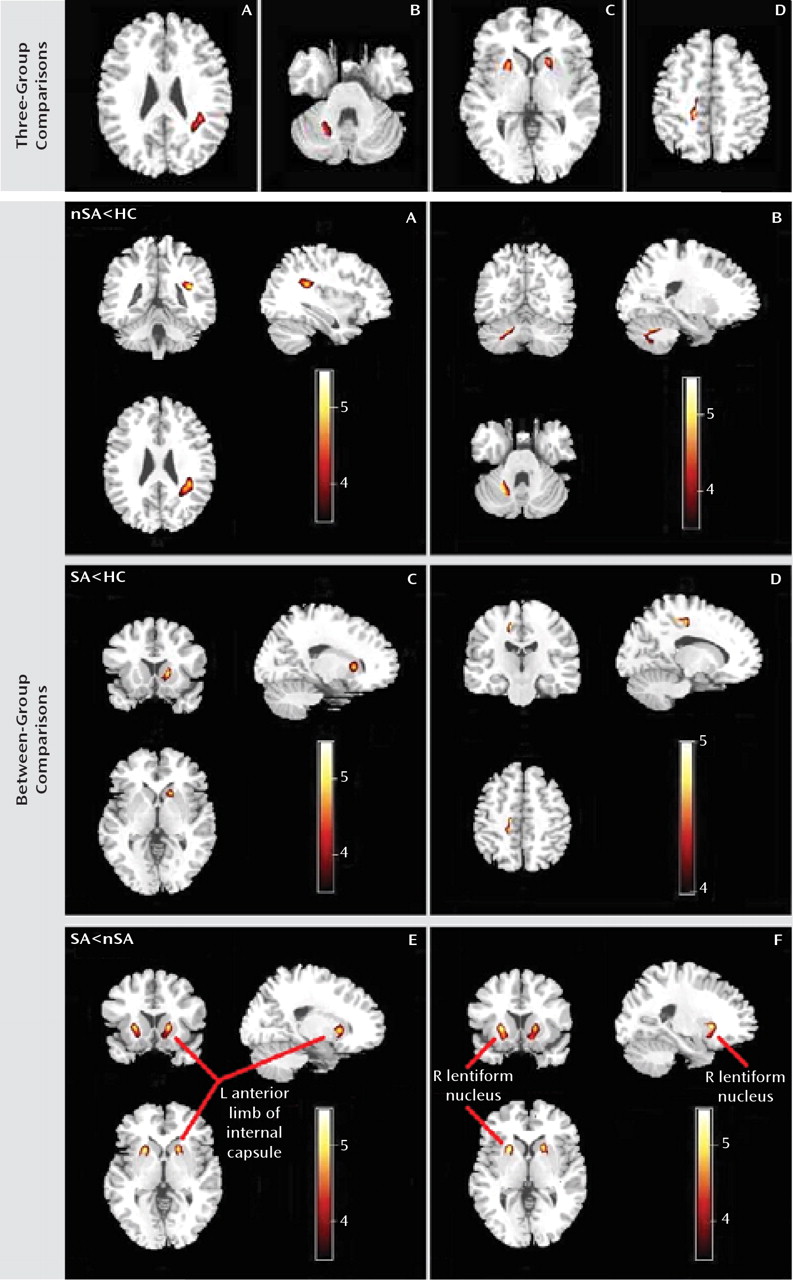
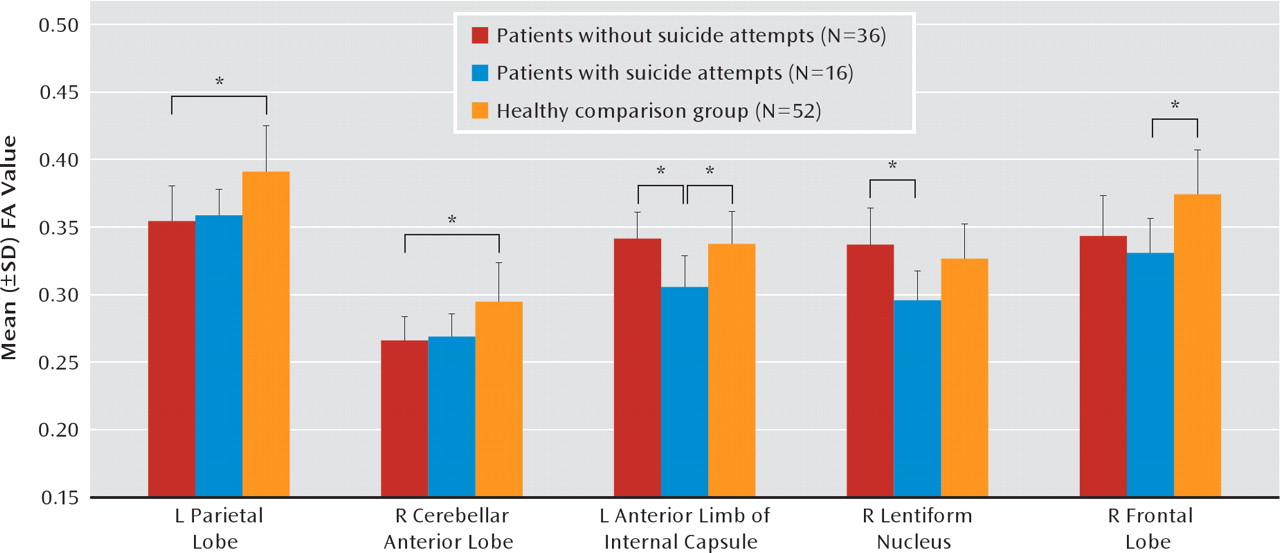
The main findings are that suicide attempters had lower fractional anisotropy in the left anterior limb of the internal capsule relative to both nonsuicidal patients and healthy comparison subjects. In addition, suicide attempters had lower fractional anisotropy in the white matter of the right frontal lobe relative to healthy comparison subjects and in the right lentiform nucleus relative to nonattempters. Furthermore, nonattempters had reduced fractional anisotropy in the white matter of the left parietal lobe and right cerebellum relative to healthy comparison subjects.
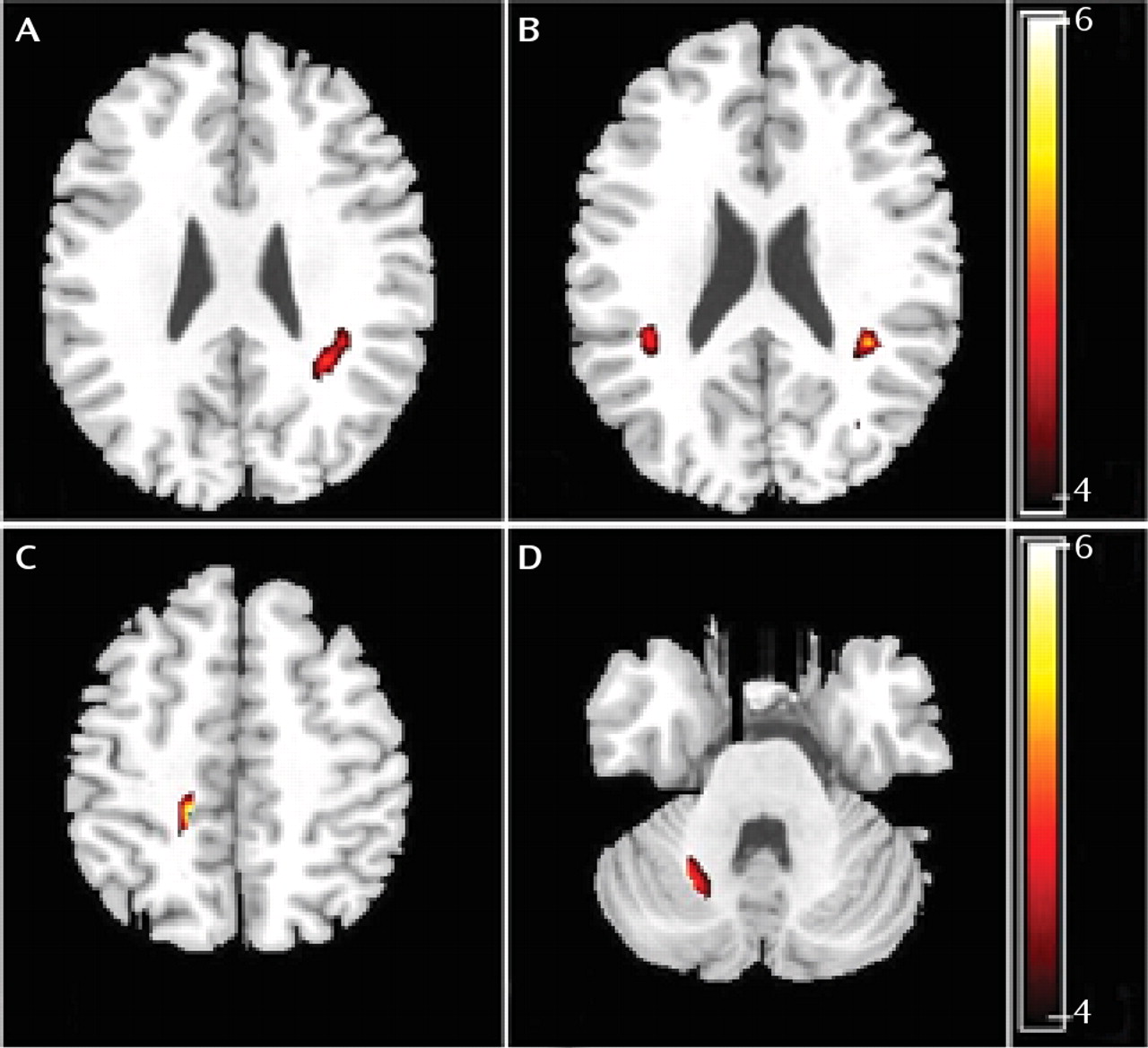
Optimized voxel-based morphometric analysis detected no morphological changes in gray or white matter comparison among the three groups. This appears to be inconsistent with voxel-based analysis of fractional anisotropy, for which there are several possible reasons. Voxel-based morphometry allows unbiased and objective comparison of local gray matter concentration between groups (
24,
25). However, it is susceptible to normalization and segmentation confounds that may affect sensitivity (
15). For example, nonlinear distortions in MRI may compromise registration accuracy, affecting the group comparison (
15). Furthermore, group-specific patterns of abnormal anatomy may result in group-specific misregistration (
24,
25). Finally, one experimental group may move more in the scanner than the other, resulting in group-specific motion artifact, which may interact with the segmentation to produce systematic classification differences (
24,
25). Alternatively, diffusion tensor imaging may be more sensitive to subtle white matter abnormalities without volumetric changes detectable by structural MRI, for example, in neurological disorders (
26).
Fractional anisotropy, the fraction of directional diffusion in white matter, is influenced by fiber organization, myelination, and integrity. We found that suicide attempters had significantly lower fractional anisotropy than healthy comparison subjects in white matter of the left anterior limb of the internal capsule, while nonattempters did not. Microstructure abnormalities in this region are likely to involve demyelination or axonal damage and might be expected to trigger malfunctions in other areas of the emotional regulatory circuit (
27). Axonal damage leads to a marked decrease in axial diffusivity and only modest decreases in radial diffusivity. In contrast, demyelination (e.g., in multiple sclerosis) leads to an increase in radial diffusivity without change in axial diffusivity (
28). The reduced fractional anisotropy in the left anterior limb of the internal capsule was associated with decreased axial diffusivity but unchanged radial diffusivity, suggesting that it was not a result of demyelination but of gross reduction in axonal number and/or size.
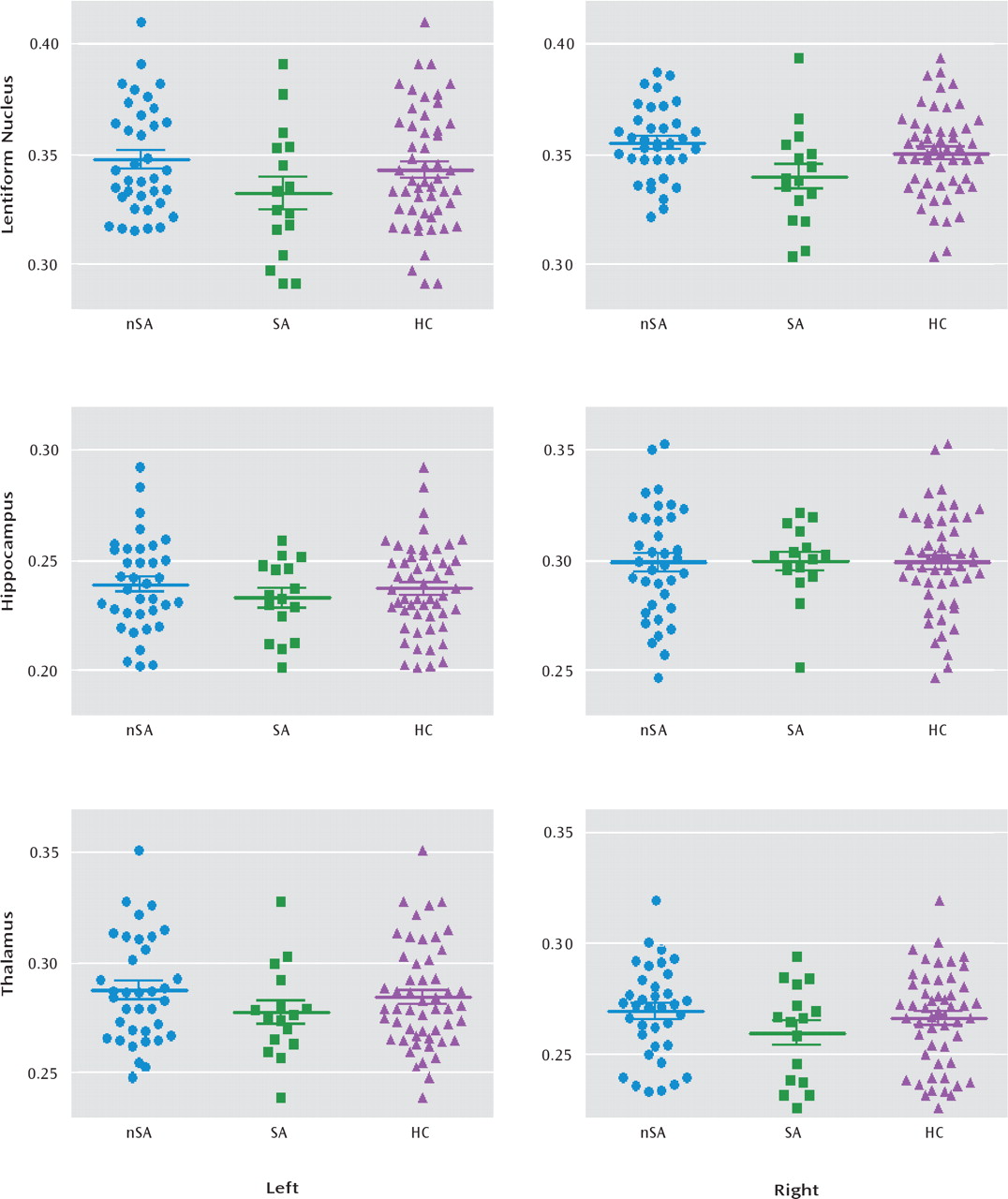
In addition, both voxel-based and region-of-interest analysis revealed that suicide attempters had reduced fractional anisotropy in the right lentiform nucleus relative to nonattempters, although neither patient group differed significantly from healthy comparison subjects in this area. This is consistent with a previous report that showed major depressive disorder patients with a history of suicide attempts had significantly more subcortical gray matter hyperintensities than nonsuicidal patients (
7). The lentiform nucleus, which is the part of the corpus striatum lateral to the internal capsule, has been reported to be associated with experiencing sad events or unpleasant stimuli (
29). This area is dense with dopamine innervation and has a moderate amount of serotonin innervation (
30). Dopamine and serotonin are thought to be connected with suicidal behavior in depressed patients (
31). It is therefore possible that altered white matter integrity in the right lentiform nucleus is related to abnormalities in dopamine and serotonin function, although the causal direction of such association is yet to be established. The lentiform nucleus also belongs to the limbic-striatal-pallidal-thalamic circuit, which plays an important role in the regulation of affect and cognition (
19). Different parts of the lentiform nucleus have distinct afferent and efferent connections with other regions of this network. Thus, it is possible that a localized abnormality of the lentiform nucleus may affect other regions of the network, contributing to the pathogenesis in those major depressive disorder patients who intend to commit suicide.
Further, voxel-based analysis also revealed fractional anisotropy in the subgyral white matter of the right frontal lobe to be significantly reduced in suicide attempters relative to healthy comparison subjects, although not in nonattempters. Reduced fractional anisotropy in the frontal lobe was associated with increased radial diffusivity and unchanged axial diffusivity, which suggests reduced axonal myelination and/or alterations in the axonal cyto-skeleton, increasing water diffusion perpendicular to the primary axonal axis. An earlier diffusion tensor imaging study reported an association between impulsivity and the reduction of microstructural integrity of frontal white matter systems in other psychiatric diseases characterized by disturbed serotonin function (
32). The study also suggested that decreased serotonin activity in the frontal lobes may contribute to the pathogenesis of major depressive disorder patients who attempt suicide (
33).
We also found that relative to healthy comparison subjects, nonattempters had lower fractional anisotropy in the left subgyral parietal lobe and right cerebellum. Although there was no significant difference between suicide attempters and comparison subjects in these regions, this decrease in fractional anisotropy is perhaps related to major depressive disorder per se. The abnormality in white matter of the left parietal lobe is consistent with a previous report of structural abnormalities in treatment-naive young adults with major depressive disorder (
34).
The cerebellum is anatomically and functionally connected to the prefrontal cortex, subcortical limbic structures, and monoamine producing brainstem nuclei (
35). Disruption of the functional connections between the cerebellum and frontal lobes impairs expression of emotion (
36). The cerebellum is also implicated in dysregulation of affect (
36). A recent study using repetitive transcranial magnetic stimulation showed that inhibition of cerebellar function leads to impaired regulation of emotion and increased negative mood (
37). It is possible that the reduction in fractional anisotropy in the cerebellum is related to the reductions observed in the cerebellar levels of glial fibrillary acidic protein in individuals with major depressive disorder (
38).
Neither voxel-based nor region-of-interest analysis yielded any evidence of reduced fractional anisotropy in the bilateral hippocampus and thalamus in either patient group, which was unexpected, since these parts of the limbic system are thought to play a crucial role in the early pathogenesis of major depressive disorder (
39). Nevertheless, this finding is consistent with a previous study that reported no significant differences in the volume of the hippocampus and thalamus in suicidal and nonsuicidal female patients with major depressive disorder (
40).
Our study has some limitations. First, the subgroup of suicide attempters was relatively small, which may have limited statistical power. However, we maximized sensitivity in crucial areas by performing a region-of-interest analysis in conjunction with the whole-brain voxel-based analysis. Second, there was no psychiatric comparison group (e.g., schizophrenia patients with a history of suicide attempts). Therefore, it cannot be concluded from our study that reduced fractional anisotropy in the left anterior limb of the internal capsule, right frontal lobe, and right lentiform nucleus is specific to suicidality in major depressive disorder. Indeed, a recent study of structural correlates of past suicidality in schizophrenia implicates the fronto-temporo-limbic circuits (
41). To clarify this, future studies should include subjects with different psychiatric disorders with and without a history of suicide attempts. Third, specific modes, such as violent versus nonviolent suicide behaviors, are believed to be associated with particular phenotypes (
42). It may be of interest to examine their changes in fractional anisotropy, for which a large cohort study would be required. Finally the present results cannot establish the direction of causality (i.e., whether reduced fractional anisotropy causes a predisposition to suicide attempts or vice versa or whether both are the result of a separate cause). To clarify this, a longitudinal approach would be required to examine patients before and after a suicide attempt.
The frontal-striatal-thalamic-cortical circuits, connected by the anterior limb of the internal capsule, play an important role in behavioral regulation (
43), and the anterior limb of the internal capsule is the most frequent therapeutic target in obsessive-compulsive disorder and depression (
44,
45). The decreased fractional anisotropy we observed in the frontal lobe, anterior limb of the internal capsule, and lentiform nucleus in suicide attempters suggests a possible abnormality of neuroanatomic pathways in frontal-striatal (lentiform nucleus) circuits passing via the anterior limb of the internal capsule. Specific lesions or disrupted connections involving areas regulating affect and behaviors might trigger the onset of depression and confer a biological vulnerability, which in combination with environmental stressors results in suicidal behaviors.
In summary, the present study suggests that fractional anisotropy reductions in the left anterior limb of the internal capsule characterize those patients with major depressive disorder who have made suicide attempts. In order to identify those at greatest risk and eventually develop more effective preventive strategies, future longitudinal studies should use neuroimaging techniques in conjunction with genetic approaches for a multidimensional characterization of predisposition to suicidality in major depressive disorder.