T
o the E
ditor: Augmenting treatment with antidepressants with second-generation antipsychotics for partial- and nonresponders to first treatment and for psychotic depression is recommended on the basis of excellent evidence by most pharmacological treatment guidelines for depressive disorders (
1). The data from the Research on Asian Psychotropic Prescription Patterns for Antidepressants (REAP-AD) study include information on pharmacological treatment for outpatients with depressive disorders over the period March to June 2013 in 10 Asian countries: China, Hong Kong, Japan, Korea, Singapore, Taiwan, India, Malaysia, Thailand, and Indonesia (
2). A total of 827 outpatients, aged from 18 to 80 years and diagnosed with depressive episode (F32) or recurrent depressive disorder (F33) according to ICD-10, were enrolled.
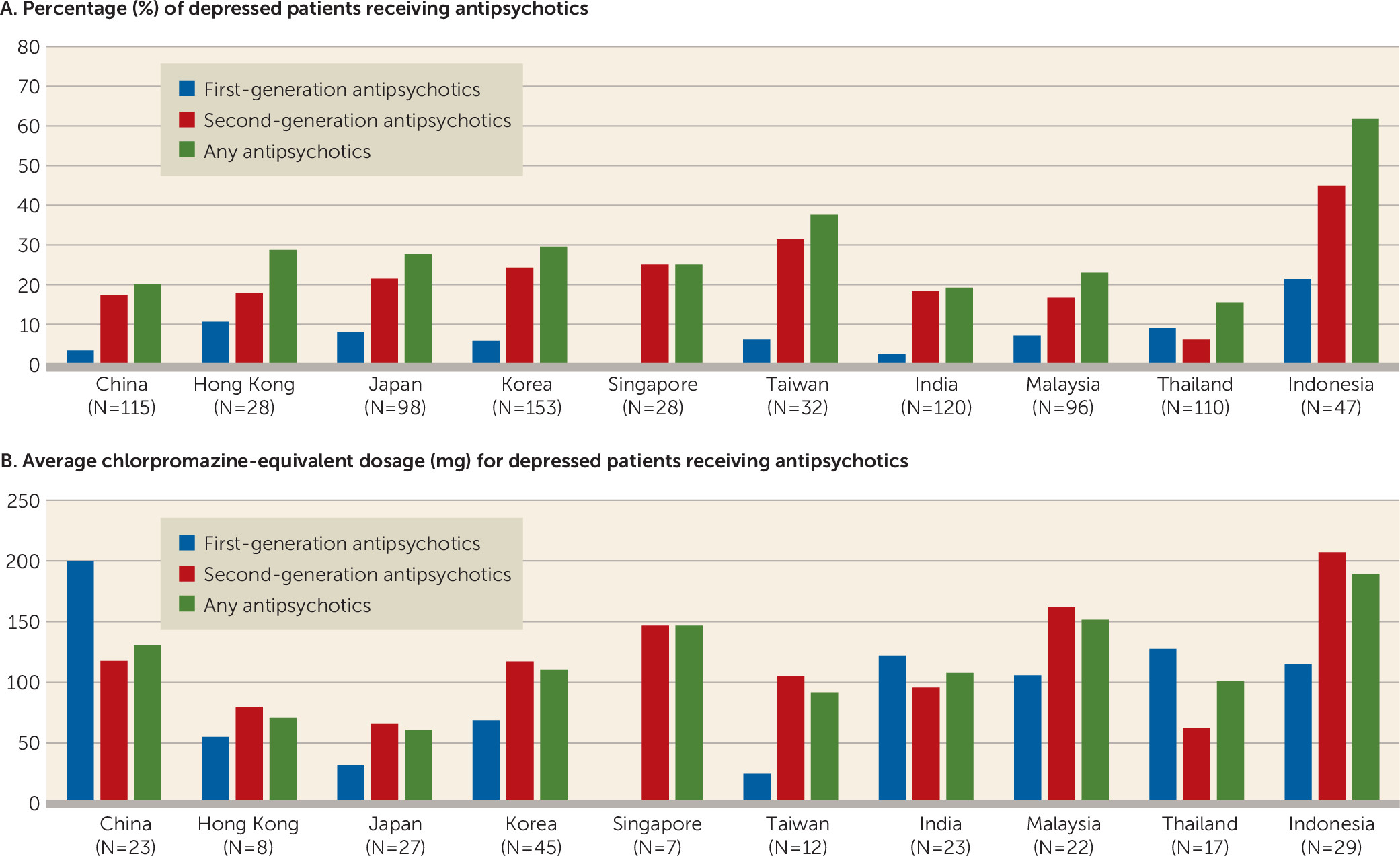
The average antipsychotic prescription rate in these depressed outpatients in Asia was 25.8% (N=213). As shown in
Figure 1A, there was a tendency for the percentage prescription of second-generation antipsychotics to be greater than that of first-generation antipsychotics in all countries/regions, and the percentage of depressed outpatients receiving any antipsychotic ranged from 15.5% (Thailand) to 61.3% (Indonesia). The percentage of prescriptions for adjunctive antipsychotics in Indonesia was much greater than in any other country/region (χ
2=46.652, p<0.0001). The percentage of depressed outpatients receiving second-generation antipsychotics ranged from 6.3% (Thailand) to 44.7% (Indonesia), compared with 0.0% (Singapore) to 21.3% (Indonesia) for first-generation antipsychotics. As shown in
Figure 1B, the average chlorpromazine-equivalent dose for depressed outpatients prescribed with antipsychotics ranged from 61.2 mg (Japan) to 189.8 mg (Indonesia). Especially, the chlorpromazine-equivalent dose for depressed outpatients in Indonesia was greater than that in the other countries (F=2.908, p=0.003). More specifically, the average chlorpromazine-equivalent doses for depressed outpatients prescribed first- and second-generation antipsychotics ranged from 25.0 mg (Taiwan) to 200.0 mg (China) and from 62.6 mg (Thailand) to 207.1 mg (Indonesia), respectively.
A cohort study of depression in individuals ages 18 to 64 in Florida Medicaid (1996–2005) revealed a 10-year trend in which the percentage of adjunctive antipsychotic use rose from 25.9% to 41.9% (
3). The results of the present study suggest that the percentages of adjunctive antipsychotic prescriptions in the 10 Asian countries, excluding Indonesia, are somewhat lower than in the United States. Higher percentage and average chlorpromazine-equivalent dose of adjunctive antipsychotic prescription in outpatients with depression in Indonesia can be influenced by greater prevalence of psychotic symptoms and uncontrolled behaviors and economic advantages for antidepressants. Moreover, international differences in clinical manifestations of depressive disorder can be attributed to the pathofacilitative or pathoreactive effects of specific cultures (
4). In addition, adjunctive antipsychotic prescriptions for depressed outpatients can be influenced by psychopathology, cultural effects, clinical practice guidelines, national insurance systems, clinicians’ preferences, and other factors. To understand the pattern of antipsychotic supplementation for depressed outpatients in Asia, a further study identifying the most important contributing factors is needed.