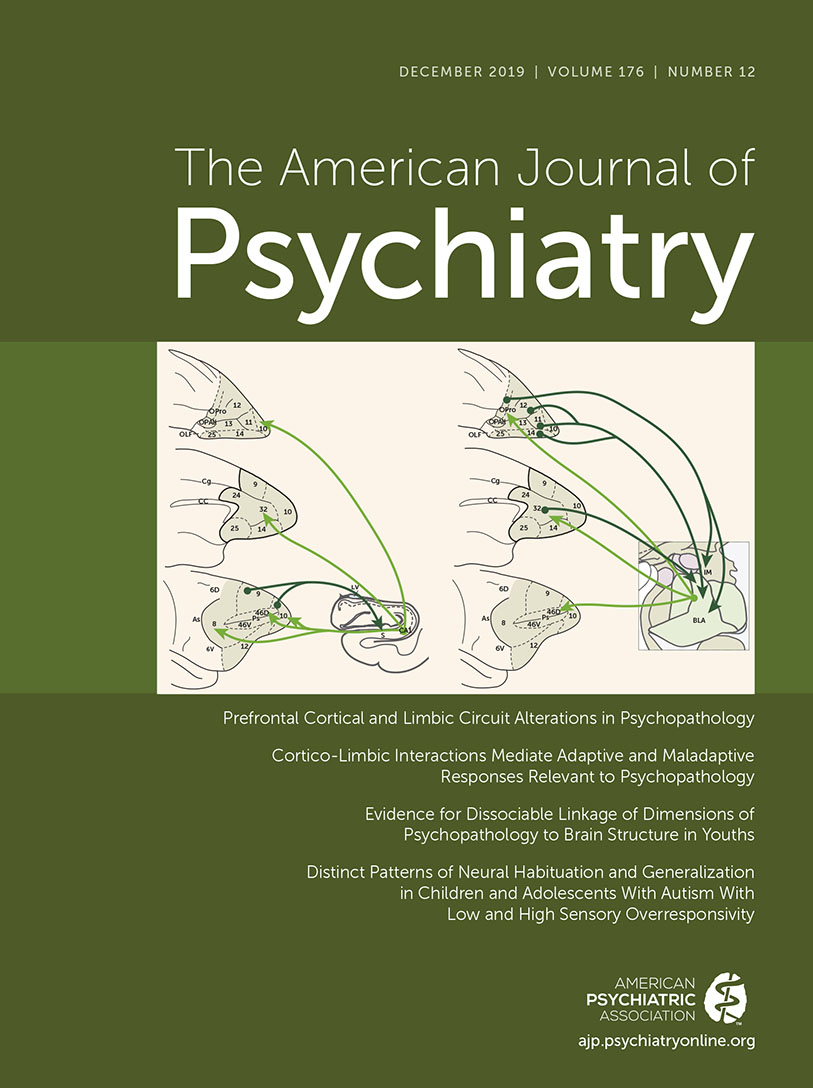
Much research has implicated various brain regions in mediating adaptive and maladaptive behaviors associated with psychiatric illnesses. Recent work has moved away from conceptualizing the role of specific brain regions in psychopathology to considering the role of structurally and functionally coupled regions that form neural circuits or networks. In this regard, focus has been placed on understanding interactions between key cortical and subcortical structures, such as the relation between prefrontal cortical regions and the historically termed limbic system. More specifically, two pathways that are highly relevant to the expression of psychopathology include those between the dorsolateral prefrontal cortex (DLPFC) and the hippocampus and between the orbitofrontal cortex and the amygdala.
In his influential work, Paul MacLean first used the term limbic system to include structures such as the septum, amygdala, hippocampus, and cingulate cortex and later conceptualized these brain components to be part of the instinctual “reptilian brain” (
1). While various definitions of the limbic system exist, it generally is thought of as a “primitive” part of the brain that is evolutionarily conserved across species and that is involved in emotion, motivation, reward, and memory formation at the most rudimentary levels. In contrast, the PFC has evolved to be highly developed in primate species, differing considerably from rodents (
2). The prefrontal cortex constitutes the most anterior cortical areas of the frontal lobe and can be subdivided into dorsolateral, ventrolateral, medial, and ventromedial or orbitofrontal regions. The PFC is thought to be a component of the brain that makes humans uniquely human, as it is involved with higher-order functions of cognition, emotion, motivation, attention, and memory and planning. The PFC integrates these functions, resulting in the ability to engage in abstract thinking and to invoke executive functions. Via its connections to subcortical structures, such as those in the limbic system, the PFC interacts to provide regulatory influences on the processing and expression of emotion and memory recall, as well as in guiding the expression of adaptive behavioral responses.
The case of the 25-year-old railroad worker Phineas Gage, in whom a tamping rod penetrated and damaged his PFC, has been used as a classic example of the higher-order and selective functions of PFC regions. After his accident, a striking change in Gage’s personality occurred, such that he was described as an unreliable, disrespectful, and irresponsible character. These changes were deemed even more significant in relation to the fact that his memory, intelligence, and capacity to learn were preserved. In a paper using modern imaging techniques with Gage’s skull, Damasio and colleagues determined that the damage suffered by Gage likely encompassed his ventromedial PFC, thereby associating this region with decision making and emotion regulation (
3). We now know from neuroanatomical and animal studies that the neural substrate underlying these functions, as well as anxiety regulation and fear extinction, involves the considerable bidirectional interconnectivity between the ventromedial PFC and the amygdala (
4).
Extensive work by the late Patricia Goldman-Rakic in primates was particularly relevant for understanding psychopathology and for setting the stage for understanding the physiological properties of neurons of the DLPFC in relation to function of this region. Her studies not only provided a cellular basis for understanding working memory but also directly tied alterations in executive functions associated with schizophrenia to altered PFC neuronal function (
5). She also described pathways in the primate that connected the DLPFC to the hippocampal formation, specifying circuits by which interactions between these regions facilitated declarative and working memory processes (
6).
In this issue of the
Journal, we present articles that are focused on brain alterations across various disorders, with an emphasis on cortical and limbic regions. As you read these articles, it is important to keep in mind that more complex neural circuits and networks are involved in modulating the function of the regions that are highlighted in these reports. This issue begins with an overview by Rothem Kovner, Jonathan Oler, and me that lays the groundwork for understanding the neuroanatomical and functional components of the limbic system and its prefrontal connectivity that are pertinent to understanding their involvement in mediating psychopathology (
7).
Using a large sample of youths from the Philadelphia Neurodevelopmental Cohort, Kaczkurkin et al. (
8) report data focused on neural alterations that are associated with fear-related symptoms across different diagnoses. The authors used a method to derive structural brain networks and found widespread reductions in cortical thickness that were specifically associated with dimensional measures of fear. Notably, the correlations between cortical thickness and fear were found in numerous regions, including the cingulate, temporal, and orbitofrontal cortex. In contrast to the relation between fear and reductions in cortical thickness, the authors also found that an individual’s overall burden of psychopathology was associated with a different cortical measure; that is, reductions in gray matter volume. In an accompanying editorial (
9), Michael Posner and Mary Rothbart, emeritus professors from the University of Oregon and experts in the development of attentional mechanisms, learning, and temperament, underscore the importance of the developmental approach used in this article and point to the value of studying brain-symptom relations dimensionally and across diagnoses.
In another article involving youths with autism spectrum disorder (ASD), Green et al. (
10) characterize differences in neural responsivity in individuals who are very sensitive to sensory input. This study helps to address the mechanisms underlying the heterogeneity of symptoms in patients with ASD by revealing that sensory stimulation–induced amygdala activation, as well as activation in relevant sensory cortical regions, fails to habituate in individuals who are highly sensitive to sensory stimulation. The authors also note that these individuals with sensory overresponsivity demonstrate alterations in orbitofrontal cortical habituation and in amygdala-orbitofrontal measures of functional connectivity. In an editorial (
11), Danny Pine, a deputy editor of the
Journal and branch chief at the National Institute of Mental Health, discusses these findings as well as a different pattern of altered neural function observed in individuals with ASD who are much less responsive to sensory stimuli. He also more broadly reflects on issues relevant to developing pediatric imaging measures for clinical use.
Two articles in this issue address alterations in limbic function in patients with schizophrenia. Using a meta-analytic approach, Dugré and coworkers (
12) conclude that patients with schizophrenia demonstrate increased activation of limbic structures, including the amygdala and hippocampus, when exposed to so-called emotionally neutral stimuli. Interestingly, these patients do not appear to differ from control subjects in response to negatively valanced stimuli. The authors interpret these findings to suggest that schizophrenia is associated with aberrant activation of the limbic system in relation to nonthreatening stimuli and that this could be relevant to the formation of delusions. However, when considering this interpretation, it should be noted that the conditions associated with performing an MRI can be quite stressful and that it is likely more stressful for individuals suffering with severe mental illness than normal subjects. Therefore, it is difficult to know what constitutes a truly “neutral” stimulus or context and how this may interact with an individual who is considerably less comfortable in the world.
In another article, McHugo et al. (
13) present data in patients with nonaffective psychotic disorders who are studied during the early phase of their illness. The data demonstrate that at baseline, using cerebral blood volume measures, these patients have increased anterior hippocampal activity. Importantly, this increased baseline activity is associated with decreased task-induced anterior hippocampal activation as measured with functional MRI. The authors conclude that the increased hippocampal basal activity could account for decreased hippocampal-related performance issues and that these findings support the idea of focusing on hippocampal dysfunction as a treatment target. In his editorial (
14), Daniel Ragland, an expert in early psychosis from the University of California at Davis, discusses the importance of using multimodal imaging methods as exemplified in this study that relate basal hippocampal activity to task-related activation. He also provides an overview of data and prevailing theories regarding hippocampal dysfunction in schizophrenia.
Finally, in an article by de Kovel et al. (
15), from the Enhancing Neuro-Imaging Genetics Through Meta-Analysis (ENIGMA) consortium, data are presented from an extremely large sample indicating that brain structural asymmetries are not associated with major depressive disorder. Although previous work from this group supports depression-related structural alterations in various brain regions, including decreased hippocampal volume and a thinner orbitofrontal cortex (
16,
17), the results presented here, using formal testing of asymmetry, do not find asymmetries in brain structure to differ between depressed and control subjects. This negative finding is interesting and important, as much smaller studies have reported some structural asymmetries. In addition, other data using EEG have supported asymmetric function of frontal regions, such that subjects with depression have been noted to have decreased left, compared with right, frontal alpha power. The authors note that the absence of structural asymmetries does not preclude the possibility of functional asymmetries and that it is possible that more subtle asymmetric neural differences exist that are not detectable by current imaging methods.
In summary, this issue of the Journal highlights cortical and limbic circuit alterations that are associated with various psychopathologies. It is not surprising that these circuits are prominently associated with psychopathology, as they are critical in mediating the adaptive regulation of emotion, in integrating cognitive with emotional responses, and in guiding the selection of motivated behaviors. A significant theme that emerges from the papers in this issue relates to understanding the degree to which structural and functional brain alterations are specific to an illness or are more general across illnesses. Additionally, it is important to emphasize that findings derived from neuroimaging studies are largely correlative and should not be interpreted in relation to causality. This speaks to the importance of integrating preclinical mechanistic animal model research with human neuroimaging studies, which is crucial in providing a neural circuit–based approach to improving diagnoses and treatments.