Coercive treatment within inpatient psychiatric facilities is widely used in daily practice (
1 ). This situation is sharply criticized by various organizations and institutions (
2 ). Many believe that these procedures signal failures in care (
3 ). However, others are of the opinion that eliminating restraint and seclusion may be difficult when treating individuals who have acute psychosis and a history of violence and whose recent violent behavior led to hospitalization (
4 ). In Europe the pattern of coercive psychiatric treatment varies widely between countries with regard to its frequency, type, and legal regulations. It is a very sensitive but rarely studied issue (
5 ).
The aim of this study was to assess the frequency and type of coercive measures used with involuntarily admitted patients in facilities in ten European countries and to identify patient characteristics that are associated with the use of coercive measures.
Methods
The main objective of the European Evaluation of Coercion in Psychiatry and Harmonization of Best Clinical Practice (EUNOMIA) project was to analyze national variations in coercive psychiatric treatment within the European region, along with influencing factors and outcomes. The project was conducted as a multicenter prospective cohort study in 11 European countries and Israel: Dresden, Germany; Sofia, Bulgaria; Prague, Czech Republic; Thessaloniki, Greece; Tel Aviv, Israel; Naples, Italy; Vilnius, Lithuania; Wroclaw, Poland; Michalovce, Slovak Republic; Granada and Malaga, Spain; Orebro, Sweden; and London, United Kingdom.
The characteristics of the individual centers, including the number of hospital beds per 100,000 inhabitants, the number of staff per bed, and the average number of beds per room were assessed with the European Service Mapping Schedule, version 3 (
6 ) and with a special instrument that helped to document the characteristics of hospitals (
7 ); these characteristics were described in our previous article (
8 ). For the evaluation reported here the centers in Israel and in the Slovak Republic were excluded because of shortcomings in their databases, which left ten countries in the sample. Two centers were sampled in Spain, and one center was sampled in each of the other nine countries.
Each participating center recruited all patients who were legally involuntarily admitted between July 2003 and December 2005 and who fulfilled the following criteria: aged between 18 and 65 years; able to sign an informed (written) consent form; not admitted to a special unit for only forensic or intoxicated patients; not admitted to a special treatment program for eating disorders, because that type of treatment would automatically include coercive treatment; no diagnosis of dementia; not included in the study before (repeated admissions during the study period); not transferred to a participating clinic from another hospital; and having a permanent living address in the catchment area of the participating hospitals.
Each patient who fulfilled the criteria was assessed at three different time points: within the first seven days of admission (time 1), at four weeks (time 2), and at three months after admission (time 3), independent of the patient's current living situation. This article discusses assessments from time 1 and time 2. Symptom levels were assessed with the 24-item Brief Psychiatric Rating Scale (BPRS) (
9 ), which was administered in most cases within the first three days after admission and very rarely up to seven days after admission. All evaluators were trained to use this scale. Interrater reliability was assessed throughout the project (assessed with videotaped interviews on the international level and with personal interviews on the national level).
Data concerning details of each application of coercive measures during the first four weeks of hospitalization (or less, if the patient was discharged earlier) were gathered using a special 16-item questionnaire designed by the EUNOMIA group for this study (
8 ). Coercive measures were defined as follows: Seclusion is the involuntary placement of an individual locked in a room alone, which may be set up especially for this purpose. Restraint is fixing at least one of the patient's limbs with a mechanical device or being held by a staff member for longer than 15 minutes. Forced medication refers to activities using restraint or strong psychological pressure (involving at least three staff members) to administer medication against the patient's will.
Informed consent was obtained from all patients in this study after they were provided a complete description of the study. The national or regional review boards of the participating centers approved the study.
All statistical analyses were performed with SPSS, version 17.0. One-way analysis of variance (ANOVA), chi square analysis, and Fisher's exact tests were performed to determine group differences in age, gender, and some clinical characteristics. The prevalence of diagnoses in countries was compared with Kruskal-Wallis test and the differences in the types and frequency of coercive measures used among countries were compared with the Kolmogoroff test.
Results
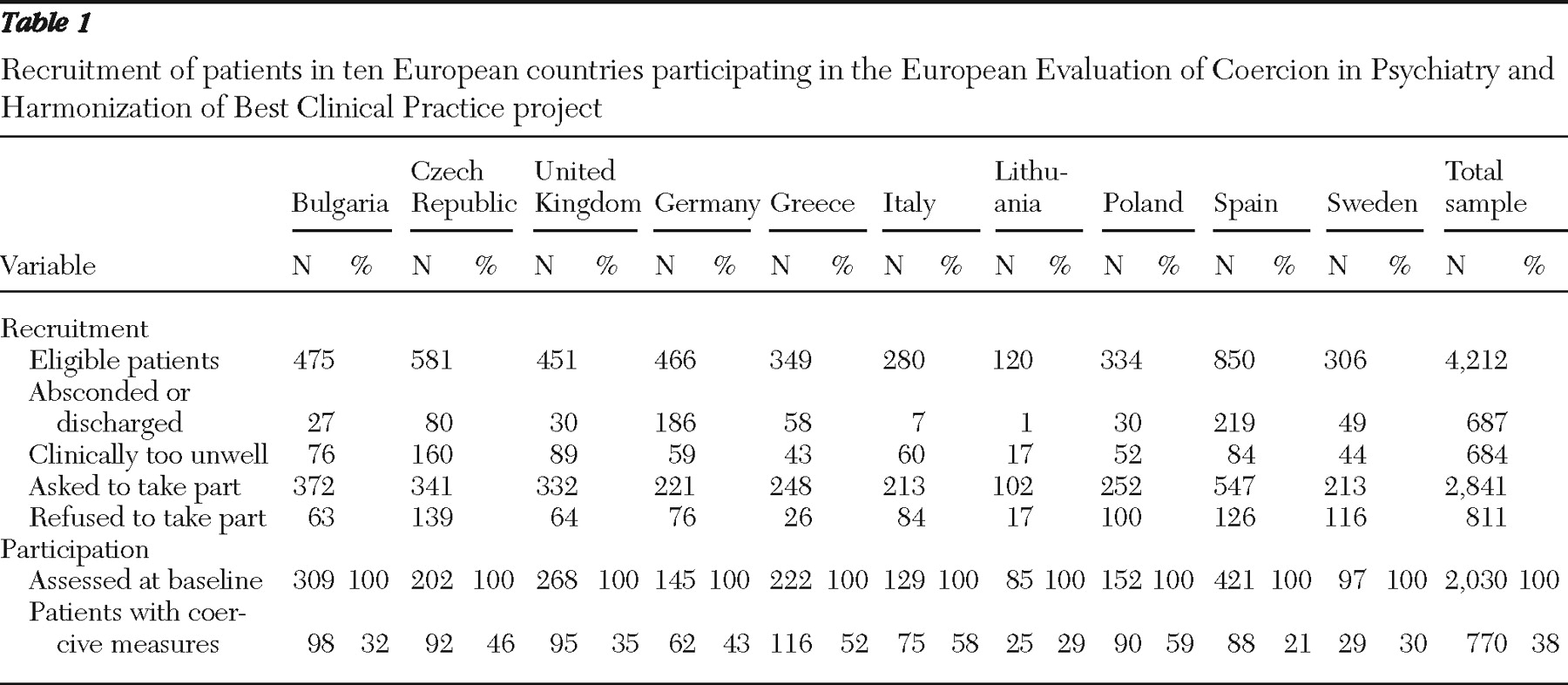
Table 1 summarizes the recruitment of patients for the study and the rates of coercion in the various countries. As shown in
Table 1, data were analyzed for 2,030 detained patients. We recorded 1,462 incidents of coercive measures that were applied to 770 patients (38% of the whole sample) during the first four weeks of the index hospitalization. There was great variability between countries (21% of detainees in Spain and 59% in Poland).
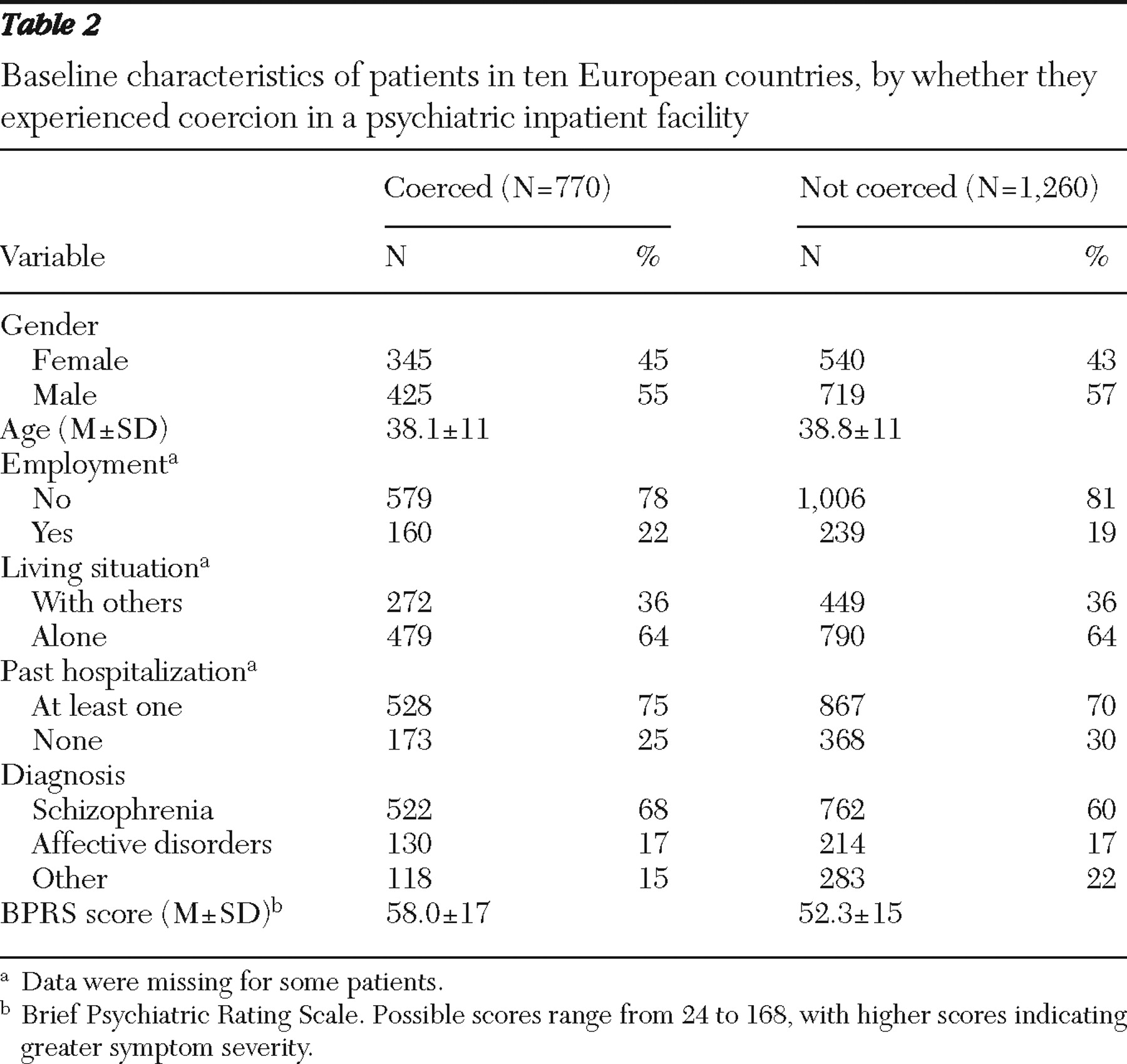
The baseline characteristics of the study sample are summarized in
Table 2 . We compared baseline characteristics of the two groups of patients: those who experienced coercive measures (N=770) and those who did not (N=1,260). We found no significant differences regarding gender, age, employment, and living situation. However, in the group with coercive measures, there was a greater proportion of patients with a diagnosis of schizophrenia (68% versus 60%) (p=.004) and the BPRS (time 1) score was significantly higher (58 versus 52) (p<.001). (Possible BPRS scores range from 24 to 168, with higher scores indicating greater symptom severity. Each single item on the BPRS ranges from 1, not present, to 7, extremely severe.)
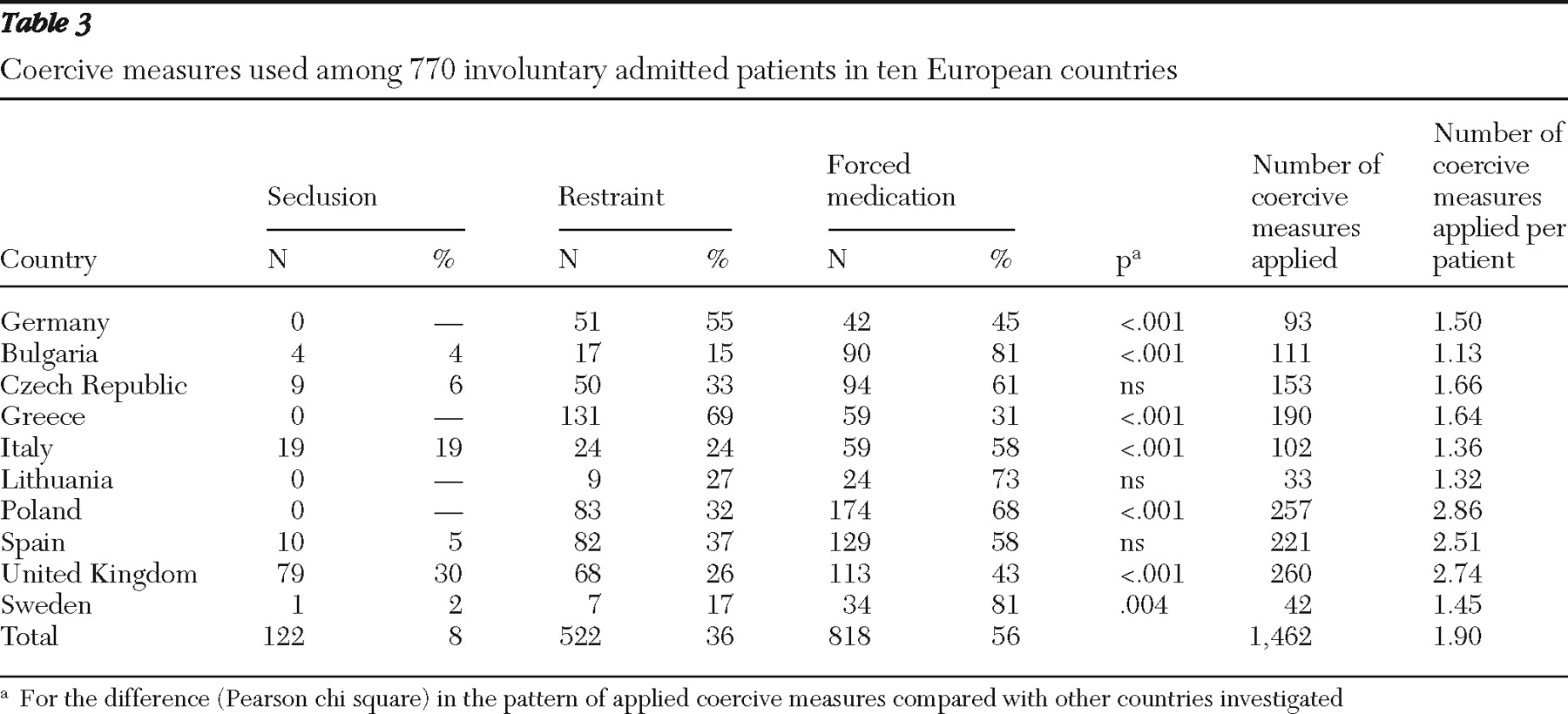
As shown in
Table 3, there was great variation in the frequency of various coercive measures used in the countries. The application of a single coercive measure per patient was the typical pattern in Germany, Bulgaria, Czech Republic, Greece, Italy, Lithuania, and Sweden; whereas in Poland, the United Kingdom, and Spain, two or more measures per patient were frequently applied. These differences between the two groups of countries in the number of coercive measures used per patient were statistically significant. The pattern of the frequency of individual coercive measures used also differed significantly when each country was compared with all other countries investigated. Forced medication was the most frequently used intervention (56%), followed by restraint (36%) and seclusion (8%). This "average" pattern was found in centers in the Czech Republic, Lithuania, and Spain. In centers in Bulgaria and Sweden, forced medication was applied more frequently than the average. Use of mechanical restraint exceeded the average in centers in Germany and Greece. Use of seclusion exceeded the average only in the United Kingdom and Italy.
The most commonly used forced medication among patients with coercive measures was first-generation antipsychotics, especially haloperidol (in 229 cases) and zuclopenthixol (in 120 cases). Also, benzodiazepines were often used separately or in combination with antipsychotics (diazepam in 111 cases, clorazepate in 92 cases, and clonazepam in 82 cases).
The most frequent reasons for use of a coercive treatment (it was possible to name more than one reason) were aggression against others (N=866, 59%), threat to his or her health (N=398, 27%), autoaggression (N=326, 22%), aggression against property (N=352, 24%), prevention of escape (N=193, 13%), and inability to care for oneself (N=165, 11%).
Only in the center in the United Kingdom were nurses more likely than physicians to order coercive measures (N=154, 59%, versus N=103, 40%). In addition, the order was expressed in writing in most centers, although in the United Kingdom and Italy an orally expressed order was also sufficient: orders were given orally in 74 of 260 orders (28%) in the United Kingdom, and 49 of 102 orders (48%) in Italy (N=49, 48%). Almost all patients were informed about the reason (N=1,256, 98%) and the type of the coercive measure being used (N=1,225, 96%).
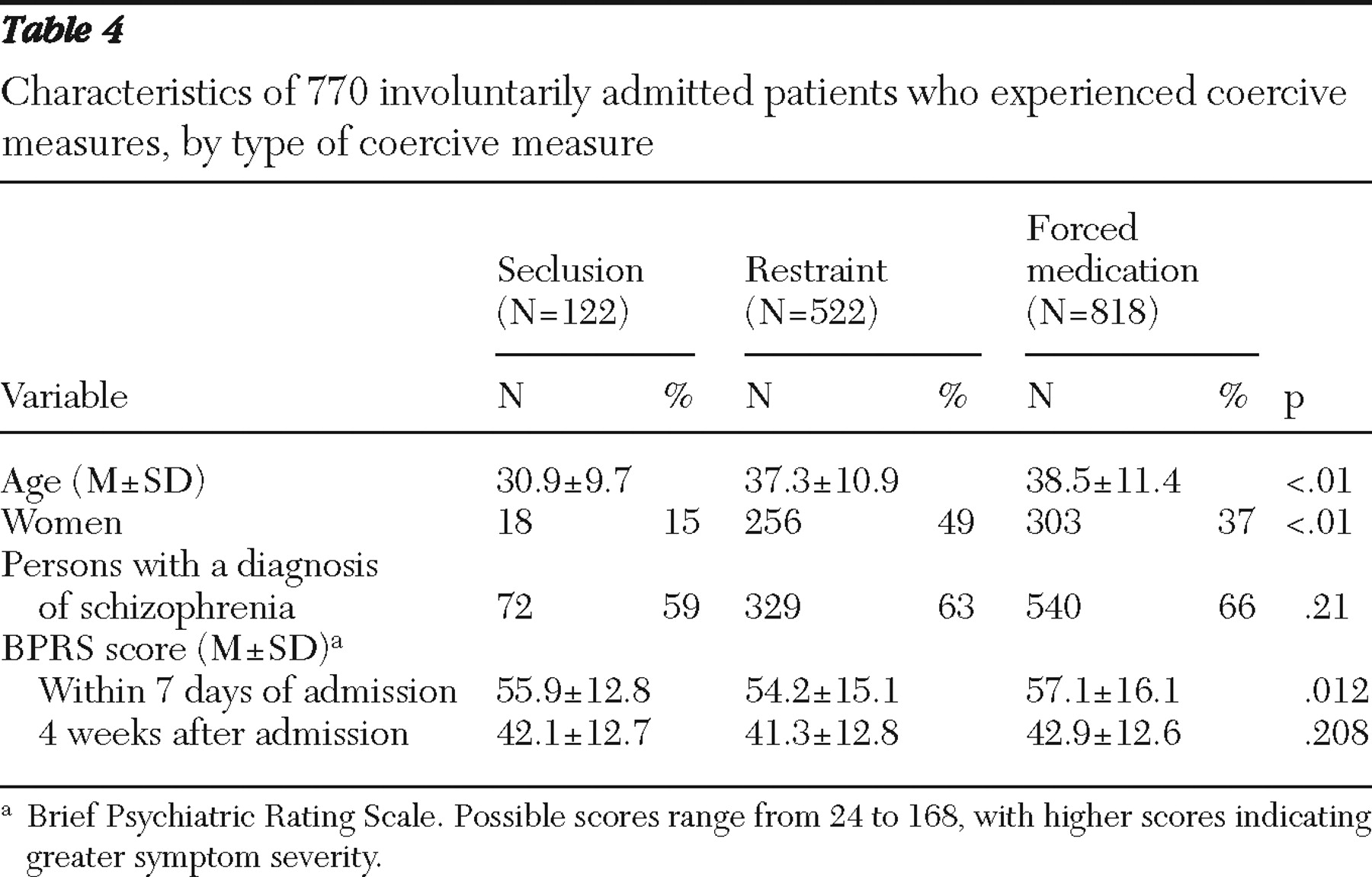
Characteristics of patients for whom the different types of coercive measures were used are summarized in
Table 4 . The statistical analysis found that age, gender, and BPRS score at time 1 were significantly different according to the type of coercive measure used. Seclusion was used more often among younger men. Forced medication was applied with older male patients who had more severe psychopathological symptoms. Restraint was used with equal frequency for both men and women.
In our previous article we described the technical characteristics of individual centers (
8 ). Vast differences were found in the number of psychiatric hospital beds per 100,000 (4.6 in Italy and 63.7 in Germany), the number of staff per bed (.4 in the Slovak Republic and 2.0 in Sweden and Italy), and the average number of beds per room (1.2 in Sweden and 8.0 in Lithuania). However, the study presented here did not find any significant correlations between coercive measures used and these technical characteristics.
Discussion
This is the largest prospective study of the use of coercive measures among involuntarily admitted patients in Europe, and it is the first one to use the same methods across locations in several countries. It included centers in ten European countries with different legislation and practice concerning involuntary admissions (
10 ). It is known that involuntary legal status on admission is a predictor of "heavy use" of restrictive interventions (
11 ) and higher levels of restraint and seclusion (
12 ). Therefore, the frequency of coercive measure use in our sample of hospitalized patients was 38%, which was higher than the rates found in other studies of different groups of patients in various European countries—for example, 11% in Greece (
12 ) and 10% in Germany (
13 ).
It is quite important to find specific patient factors and health care factors that predict use of coercive measures, so that treatment programs can be adjusted to better help these groups of patients and thus reduce the number of involuntary admissions and compulsory treatments (
14 ). Several studies have examined the frequency of various types of restrictive measures and the preferences of staff and patients. In a Norwegian university psychiatric hospital (
15 ), a retrospective examination of hospital records showed that physical restraint was preferred with younger, male, and nonpsychotic patients. Pharmacological restraint was preferred with female patients and older patients with a nonorganic psychotic disorder. Seclusion was preferred with older male patients with an organic psychotic disorder. In a Netherlands hospital, 166 patients underwent one or more restrictive measures during hospitalization (
16 ). An equal number of patients preferred seclusion and forced medication, and the two measures were equal in perceived aversiveness and perceived efficacy. Women preferred medication over seclusion, while men preferred seclusion over forced medication. Older patients considered both seclusion and forced medication less effective than younger patients did (
16 ). In England, service users and staff strongly disapproved of net beds and mechanical restraint (
17 ). The three methods that received the most approval by the service user group were intermittent observation, time-out, and as-needed medication.
For more than one-third of patients in our sample, at least one coercive measure was used during the period up to four weeks after involuntary hospitalization. A diagnosis of schizophrenia and higher scores on the BPRS were significantly correlated with receipt of coercive measures. We found significant variations in relative frequency and type of measure used in the ten countries. In most countries medication, especially first-generation antipsychotics or benzodiazepines, was used. Only in two countries included in the study (Germany and Greece) were mechanical restraints used more often than the average. Seclusion was used more than the average only in Italy and the United Kingdom. In many hospitals these special rooms for seclusion were not available.
There are several limitations regarding our findings. Overall, only about 50% of the eligible patients were interviewed. This rate may be seen as low in many other fields of health research, but it has been described as good for this type of study in acute settings with difficult-to-recruit patients (
18 ). For the comparison of recruited and nonrecruited patients, only minimal data were available for the United Kingdom, which did not suggest a selection bias on the assessed characteristics (
19 ).
We assessed between one and five hospitals in each country (
8 ). We know that the variance in use of coercive measures even between hospitals in the same country is high (
20 ). Therefore, our results cannot be generalized. However, they seem to be valid for the catchment areas that we were able to describe in detail (
8 ).
Data on use of coercive measures were based on available documentation and additional sources. The routines for documentation of coercive measures may differ between participating countries, and the number of unrecorded or unreported measures may also differ. However, all countries used a uniform and standardized protocol for data collection and thoroughly gathered all available information.
Over the past decade, especially in the United States, several programs minimizing the use of coercive measures during psychiatric treatment were launched, and these have been discussed in several publications (
21,
22,
23,
24,
25,
26 ). It was even found that reducing compulsory treatment decreased financial expenditures (
27 ). Scanlan's analysis (
28 ) of recent literature described seven key strategies for coercive measure reduction programs: change in policy or leadership, external review or debriefing, data use, training, consumer and family involvement, increase in staff-to-patient ratio or use of crisis response teams, and changes in program elements.
Similar trends are also evident in some European countries (
5 ). The EUNOMIA team is of the same opinion that during procedures for involuntary hospital admission and the admission itself, patients' rights should be recognized and interventions should adhere to the principle of the "least restrictive alternative" (
29 ). Avoidance of all coercive measures in clinical practice is an unrealistic goal for the time being. Coercive measures are used in many hospitals for acute patients (
30 ) and regulated through legislation. Therefore, acceptance of official national guidelines (
31 ) and even of European guidelines on regulating and using and use coercive measures (
10,
29 ) could be an appropriate step in maximizing the individual freedom of psychiatric patients during hospital treatment.
Conclusions
We evaluated a group of more than 2,000 detained patients in psychiatric facilities in ten European countries. For more than one-third of patients, coercive measures were applied during the first four weeks of involuntary treatment. The ten countries varied greatly in the frequency and type of coercive measure used. Age, gender, diagnosis, and severity of psychopathology played an important role in this regard. Overall, we did not find any statistically significant influences of the technical characteristics of countries (that is, number of psychiatric hospital beds per 100,000, number of staff per bed, and average number of beds per room). Nonetheless, the influence of an individual country was obvious. Therefore, we share the opinion of other authors (
32 )—that is, a country's sociocultural traditions, as well as its treatment customs in individual psychiatric facilities, play a decisive role in this very sensitive issue. However, this very important area of psychiatric care needs further study. Future research projects could identify the factors in legislation and clinical practice, including important staff-patient interactions (
33 ), that could lead to a more constructive cooperation of all parties involved. Currently, programs and practice guidelines that would rationalize and minimize the use of coercive measures in psychiatric facilities are needed.
Acknowledgments and disclosures
This study was funded by a grant from the European Commission (Quality of life and Management of Living Resources Programme, contract number QLG4-CT-2002-01036).
The authors report no competing interests.