A 1999 landmark report by the Institute of Medicine on the quality of care in general hospitals found high rates of patient injuries and preventable deaths associated with medical errors (
1 ). Since that report, quality management of hospital care environments has become a high national priority, with a large emerging research base showing that organizational factors—such as institutional policies, nurse staffing, and other processes—may inadvertently contribute to worse outcomes and medical errors (
2 ). This research was specific to the medical-surgical sector of general hospitals, and there are comparatively few studies of adverse events for inpatient psychiatric care settings even though inpatient psychiatric services are provided in most general hospitals (
3 ). In our study, organizational features of the general hospital inpatient psychiatric care environment were examined in relation to adverse event outcomes.
In the medical-surgical sector of general hospitals, an understanding of quality and safety has guided the development of important interventions to prevent errors and lower the incidence of adverse events (
1,
2,
4 ). Yet similar progress has not been achieved in the psychiatric sector in these same hospitals. Over the past 15 years, research on medical-surgical hospital environments shows that worse environmental conditions in inpatient care correlate with higher patient mortality, more patient complications, lower job satisfaction among nurses, expression of greater emotional exhaustion by nurses, and higher rates of nurse turnover (
5,
6 ). Concurrently, an Institute of Medicine study titled
Keeping Patients Safe: Transforming the Work Environment of Nurses concluded that there was ample evidence that deficient hospital care environments create patient safety hazards (
2 ).
Research on adverse events in psychiatric inpatient care is limited to a few single-hospital or single-health system studies of medication errors (
7,
8,
9 ). These studies show high rates of medication errors. Grasso and colleagues (
7 ) retrospectively examined the rate of medication errors in a state psychiatric facility during 1,448 patient days from a randomly selected sample of discharged patients. Their study detected 2,194 medication errors, an error rate that is similar to rates reported for general medical care units. One recent survey revealed that among the various inpatient units within a large hospital, the highest rate of adverse drug events occurred within the inpatient psychiatric unit (
7,
10,
11 ). Rothschild and colleagues (
12 ) found that whereas nonpsychotropic drugs accounted for only 4% of nonpreventable adverse drug events in a psychiatric hospital setting, these medications were associated with nearly one-third of all preventable adverse drug errors, indicating that psychiatric providers may commit more medical errors when managing comorbid nonpsychiatric disorders, such as diabetes or cardiovascular disorders. Inpatient psychiatric care settings need to be evaluated.
The care environment is conceptualized in our research as the organizational features that facilitate or undermine the professional practice of nurses (
13 ). (Throughout this article, reference to "nurse" means "registered nurse.") Organizational features include nurse staffing, quality of care programs, manager skills, and relationships among doctors and nurses (
13 ). The development of these particular organizational features grew from studying hospitals known for excellence in nursing care and retention of nurses during a major nurse shortage in the early 1980s. The results are influenced by theoretical perspectives from the sociology of organizations and professions (
14,
15 ).
We theorized that both the human resources available (quantity and quality of staff) and the social and political organization of the work environment (the care environment) influence the occurrence of adverse events for patient and nurse outcomes. These two aspects of organization, staffing, and environment were hypothesized to have a dynamic relationship and represent the process of care. For example, improved professional environments may attract nurses more easily (increasing the quantity of staff), may retain nursing staff (increasing stability), or may attract or retain more qualified staff (that is, more highly educated nurses). More nurses, better-qualified nurses, and a more favorable environment all contribute to better nursing care processes or, broadly speaking, processes of care. A better process of care, in turn, may lead to fewer treatment errors and adverse events.
The study reported here examined the extent to which organizational factors of the inpatient psychiatric care environment are associated with psychiatric nurse reports of adverse events in general hospitals. We hypothesized that more highly rated organizational factors would be associated with lower psychiatric nurse reports of the occurrence of adverse events—wrong medication or doses, patient falls with injuries, complaints from patients and families, work-related staff injuries, and verbal abuse directed toward nurses. If such organizational factors are linked to adverse events, these study findings could contribute to a high-priority national agenda for generating evidence-based practice and forwarding a quality and safety agenda for inpatient psychiatric care in general hospitals.
Methods
Using a cross-sectional design, we linked psychiatric nurse survey data and hospital data to examine associations between organizational factors and adverse event outcomes. We performed a secondary analysis of 1999 nurse survey data obtained from a large random sample of registered nurses from the Commonwealth of Pennsylvania (
16 ). Nurse respondents were instructed to write in the name of their employing hospital on the survey. The hospital name was linked with the American Hospital Association (AHA) survey data for information about the hospital (
17 ). The psychiatric nurses' responses were then aggregated to the hospital level to create measures of the care environment and staffing in each hospital. The nurse survey posed questions about the quality of the patient care, organizational factors that facilitated or undermined nursing practice, and the presence of adverse events. Approval of the study's work with human subjects was obtained from the University of Pennsylvania Institutional Review Board.
Nurse sample
Psychiatric nurses (N=353) were identified from a large nurse survey conducted in 1999. The nurse survey was mailed to nearly 80,000 nurses from Pennsylvania. Names and addresses of the nurses were obtained from state licensure lists.Nurse respondents were asked to write the name of their hospital on the survey. The nurse survey response rate was 52%, with over 43,000 nurses responding (
16 ). In social service research, a 50% response rate for mailed surveys is usually acceptable unless there are concerns about meaningful response bias (
18 ). Principally we were concerned with the hospital nonresponse bias because our analyses were performed at the hospital level. By asking nurses to write in the name of their hospital, we virtually eliminated the nonresponse bias at the hospital level because hospitals could not opt out of the study.
The subset sample of 353 psychiatric registered nurses declared on the nurse survey that they were permanently assigned to the direct care of psychiatric patients. We kept responses from only the psychiatric registered nurses affiliated with hospitals defined as non-federally funded acute care hospitals; we thus examined general hospitals exclusively. Because the original survey did not selectively survey psychiatric nurses, we examined the representation of our psychiatric nurse sample using the 2000 National Sample Survey of Registered Nurses (NSSRN) (
19 ). The NSSRN is a randomized national sample survey of the registered nurse workforce obtained every four years since 1978 and is the most widely used source of information about registered nurses in the United States. Demographic characteristics (including age, sex, and nursing education level) of the 353 psychiatric nurse respondents in our study were not significantly different from the NSSRN hospital-based psychiatric nurses in Pennsylvania.
Hospital sample
Using the 1999 AHA annual survey, we selected general hospitals with a minimum of six licensed psychiatric beds. The AHA defines general hospitals as non-federally funded, short-term (or acute care) general hospitals (
17 ). Sixty-seven general hospitals were matched with the 353 employed psychiatric nurses. Hospitals meeting inclusion criteria represented 74% of all general hospitals with licensed psychiatric beds in Pennsylvania in 1999. The mean±SD number of psychiatric registered nurses per hospital was 5.3±2.8, ranging from a minimum of three to a maximum of 16 nurses. The AHA annual survey was used to describe the hospital sample bed size, teaching status, and technology status.
Explanatory variables
Nurse demographic and work characteristics. Psychiatric registered nurses were described by age, gender, years of experience as a nurse, years of experience at the current hospital, and years of experience on their unit. Nurses also identified their highest level of nursing education.
Hospital characteristics. Hospital characteristics were derived from the AHA annual survey. Teaching status was defined as either hospitals without any postgraduate medical residents or fellows (non-teaching hospital), or hospitals with postgraduate medical residents or fellows (teaching hospital). Many health services research studies use this variable to adjust for remuneration for the residents and the clinical advantage of access to more physicians. Hospital bed size was stratified as ≤100 beds, 101–249 beds, and ≥250 beds. High-technology hospitals were facilities that provide services for open-heart surgery, organ transplantation, or both, indicating more sophisticated resources.
Organizational factors of the care environment were measured according to the Practice Environment Scale-Nursing Work Index (PES-NWI) (
15 ). The PES-NWI consists of 31 items and five subscales. It uses a Likert-type scale (1, disagree; 2, somewhat disagree; 3, somewhat agree; and 4, agree). We used four PES-NWI subscales in this study, including nurse participation in hospital affairs, foundations for quality of care, manager skill at leadership, and nurse-physician relationship.
Psychometric testing has established that the PES-NWI has a stable factor structure, high internal consistency, and adequate reliability when aggregated to yield organization-level measures (
15,
20 ). Published internal consistency coefficients (Cronbach's alphas) for the subscales range from .71 to .84. Intraclass correlation coefficients, reflecting the stability of organization-level scores across repeat samples for the subscales, range from .86 to .96 (
15 ).
Patient-to-nurse staffing ratio. A question on the nurse survey asks each nurse to report the total number of patients on the unit and the total number of registered nurses during the last shift. A ratio of patients to registered nurses was computed for each nurse and then aggregated to the hospital level. The predictive validity of this method of measuring hospital nurses' workloads has been established (
21 ).
Outcome variables
Psychiatric nurses' responses to the survey questions about the frequency of adverse events over the past year were used as the outcome variables. The main question was, "Over the past year, how often would you say that the adverse event involved you or your patients?" There were four answer options: never, rarely, occasionally, or frequently. The adverse events were wrong medication or dose, patient falls with injuries, complaints from patients or families, work-related injuries to staff, and verbal abuse directed toward nurses. For analysis, the responses were grouped as never to rarely or occasionally to frequently—henceforth referred to as rare versus frequent adverse events.
Procedures and data analysis
Data for the PES-NWI subscales were initially assessed for missing data. Missing items occurred in no more than 2% of the cases. The strategy for handling missing data was to use the complete case data to predict missing item values and then to use the prediction equations to generate the actual item-specific value for individuals who were missing a response to an item (
22 ). Descriptive estimates were generated for all psychiatric nurse respondents, hospitals, and outcomes. The nurse staffing variable was log-transformed because it formed a skewed distribution. Homoscedasticity was evaluated via Levine's tests, and normality was assessed with Shapiro-Wilk tests. Multicollinearity was determined before variables were entered in analytic models (
23 ).
Unadjusted and adjusted general linear regression models were used to examine the extent to which the PES-NWI subscales and staffing influenced the occurrence of wrong medication or dose, patient falls with injuries, complaints from patients or families, work-related injuries to staff, and verbal abuse directed toward nurses. PES-NWI subscales and staffing were modeled continuously at the hospital level. Adjusted models included nurse-level characteristics of bachelor's of science in nursing (yes or no) and years of experience and hospital-level characteristics of bed capacity (≤100 beds, 101–249 beds, and ≥250 beds), teaching status (teaching or nonteaching), and use of advanced technology (yes or no). Clustering of psychiatric nurses within hospitals was accounted for with Huber-White (robust) procedures to adjust the standard errors of the estimated parameters (
24 ). The Hosmer-Lemeshow statistic was used to assess the model fit (
25 ).
Results
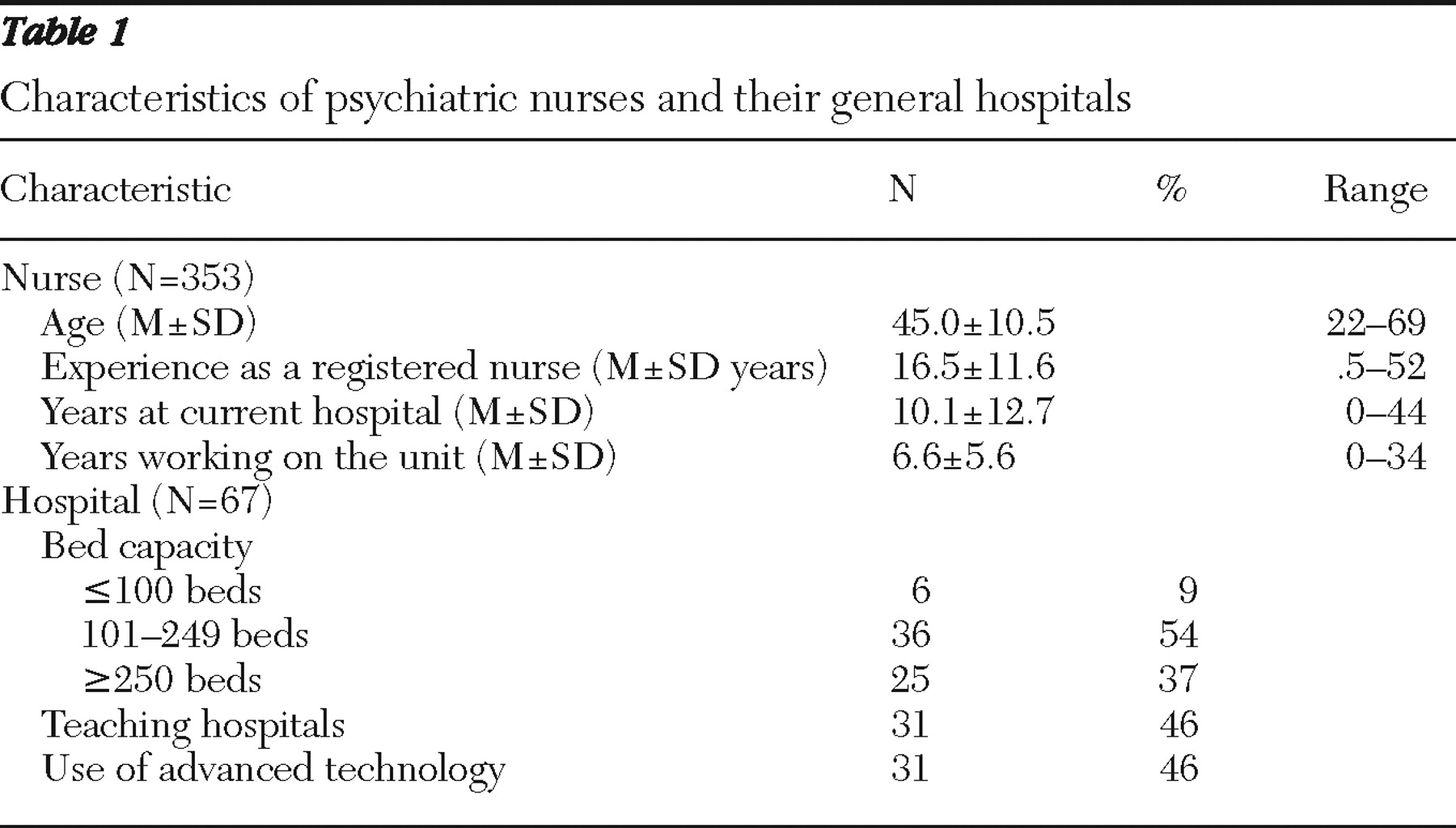
Table 1 shows that the psychiatric nurses were experienced and familiar with their work environments. They worked on average 10 years at their hospitals and seven years on their current unit. More than half of the hospitals had 101–249 beds. Forty-six percent of the hospitals were categorized as both teaching and high-technology hospitals.
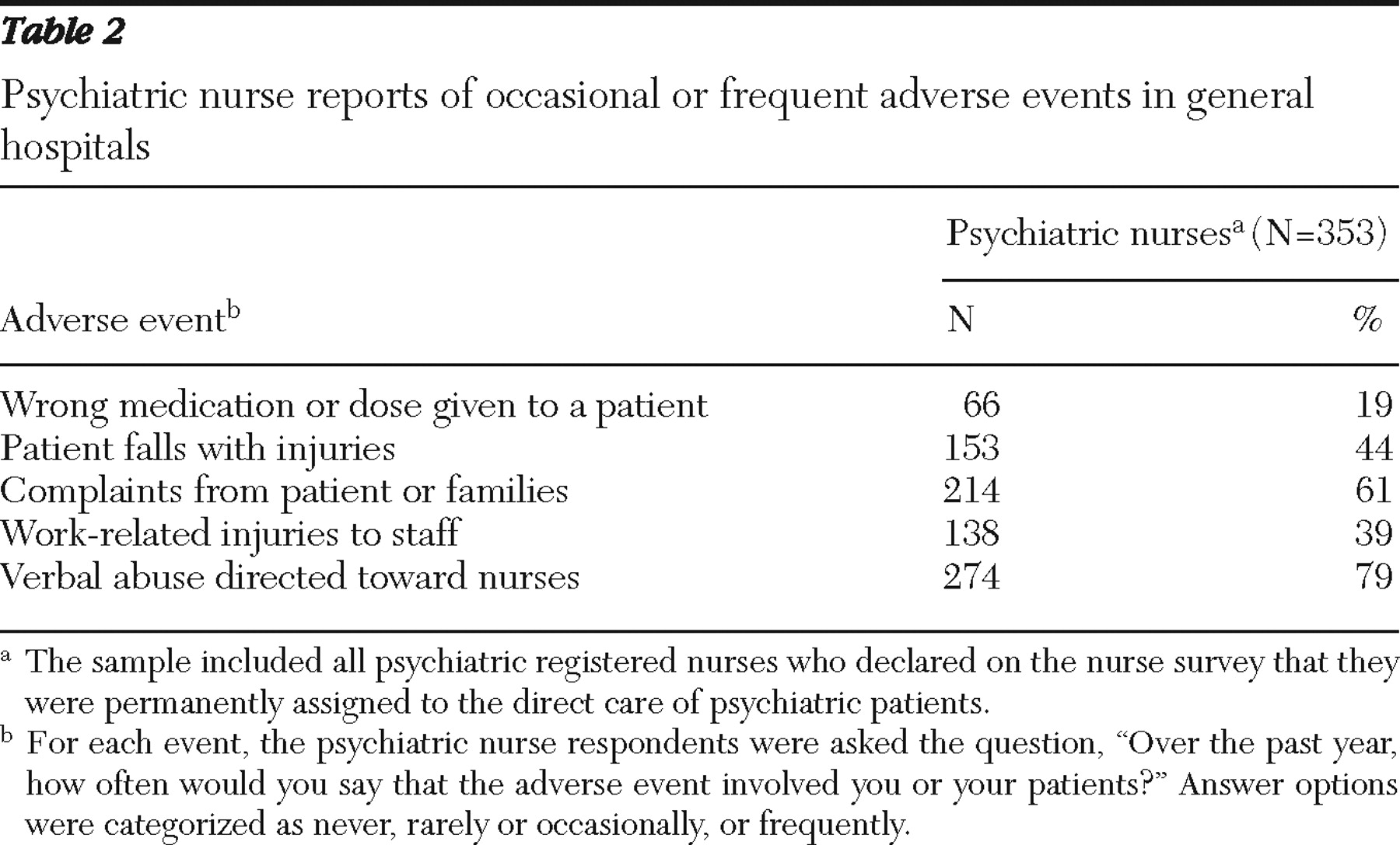
Table 2 shows the number and percentage of psychiatric nurses reporting frequent occurrence of adverse events in general hospitals. Verbal abuse directed toward nurses (79%), complaints from patients or families (61%), patient falls with injuries (44%), and work-related staffing injuries (39%) were the adverse events that occurred most frequently.
Table 3 shows that organizational factors, such as better management skill, were strongly and significantly associated with fewer reports of patient falls. Better manager skill level, nurse-physician relationship, and staffing were all highly significant and associated with fewer work-related injuries. Although statistically significant (p=.019) in the unadjusted models, verbal abuse directed toward nurses became only marginally significant (p=.053) when nurse and hospital characteristics were added in the adjusted models. The patient-to-nurse staffing ratio was 7.09±3.50 patients to 1 registered nurse. The patient-to-nurse staffing ratio was strongly and significantly related to work-related injuries to staff in both the unadjusted and adjusted models.
Discussion
Our study surveyed psychiatric nurses to report the occurrence of adverse events. Robust regression models clustered by hospitals analyzed the extent to which organizational factors of the inpatient psychiatric care environment were associated with adverse events.
Nearly two-thirds of the psychiatric nurses in our study reported frequent occurrences of complaints from patients and families (61%); they also reported patient falls with injuries (44%), staff work injuries (39%), and verbal abuse against nurses (79%). Fewer psychiatric nurses reported the occurrence of medication errors (19%) than indicated in prior research (
7,
8,
9,
10,
11,
12 ). Although it is plausible that some adverse events occur at higher rates in inpatient psychiatric settings, the dearth of evidence about the internal process in these settings makes it difficult to interpret these findings (
26 ). For example, these higher rates may also reflect unique characteristics of acute psychiatric illness. Quality parameters must be set to ensure accountability for effective use of inpatient psychiatric services and for quality improvement programs.
Almost half (44%) of the psychiatric nurses in our study reported the frequent occurrence of patient falls with injuries. To our knowledge, research about the relationship of patient falls to organizational factors of inpatient psychiatric care environments does not exist. The most obvious explanation of the occurrence of falls on psychiatric units is the side effects from medication. Antipsychotic and sedative agents are widely used on inpatient psychiatric units. Antipsychotic agents may cause orthostatic hypotension or sedation, increasing the risk of a fall (
27 ). Also widely used, benzodiazepine agents cause sedation, which also may increase the risk of falling. Coordination and motor dyscontrol are associated with use of the older antipsychotic agents. Thus falls by patients appear to be an undocumented adverse event and underestimated on inpatient psychiatric units. A better understanding of the risks and protective factors associated with inpatient falls during acute psychiatric illness are needed to design preventive evidence-based practices.
Our analysis revealed a significant relationship between organizational factors of the psychiatric care environment and adverse events. Better-skilled managers were associated with fewer injurious patient falls and with fewer work-related injuries to staff. We also found that fewer work-related injuries to staff were associated with better nurse-physician relationships and lower patient-to-nurse staffing ratios. Our findings correspond with a long-standing body of research that shows better nurse manager skills to be essential to the quality and safety of patient care (
13 ). Management and leadership are essential for excellent staff performance. The manager provides the human and material resources for care, communicates with upper-level managers, and supports nurse participation in decision making that affects patient care. For inpatient psychiatric care, the manager maintains equilibrium amidst complex and unpredictable inpatient psychiatric care environments. Patients are acutely ill, occupancy rates are high, and admissions and discharges of patients are complicated by shrinking availability of inpatient psychiatric beds and reductions in community mental health resources (
28 ).
To achieve safe and effective patient care, a manager makes critical decisions about admitting new patients while considering staffing and acuity of patients on the unit. A psychiatric nurse shortage has made this role all the more difficult because nurses are essential to the safe management of patients (
29 ). Managers must also negotiate complex and centralized bureaucracies in general hospitals where upper-level managers know little about the unique needs of psychiatric patients or the role of the staff providing the care.
Abundant research has addressed the prevalence and determinants of work-related staff injuries associated with inpatient psychiatric care (
30 ). These injuries are often related to patient factors, such as aggression, disinhibition, and irritability of mood, and to occupational factors, such as the quality and safety of the work environment. Although in many of these occupational injury studies there is reference to organizational factors, the environment often is not systematically measured. Our study suggests that organizational factors play a strong and significant role in the occurrence of work-related injury to staff. Specifically, a lack of skilled managers, poor nurse-physician relationships, and inadequate staffing were significantly associated with more frequent work-related injuries among staff. Prevention of work-related injuries should be a high priority for acute inpatient psychiatric care. Our evidence suggests that a focus on building skills among managers, fostering strong nurse-physician relationships, and staffing to adequate levels could strengthen the quality and safety of inpatient psychiatric work environments in general hospitals. However, further research is needed.
Results of this study may not be generalizable outside of the one state in which data were examined. However, the distribution of Pennsylvania general hospitals in the study compared well with national statistics on numbers of discharges, patient demographic data, and other hospital characteristics. There are study limitations, however. The response rate on the original study was relatively low (52%). However, the original sample was the entire list of registered nurses in the state of Pennsylvania. By sheer numbers, we believe we had an adequate sample of registered nurses. We do not have a response rate for psychiatric nurses because of the way the data were originally gathered. Again, this limitation introduces a response bias that can be corrected only in future studies.
It is important to note that this study was about inpatient psychiatric care in general hospitals and does not apply to other types of psychiatric settings. Self-reports from psychiatric nurses were the primary source of data for this study. Reliance on self-report raises concerns about systematic response distortions, method variance bias, and the reliability and validity of questionnaire scales, and causal relationships therefore cannot be established. Nonetheless, self-reports are widely used in organizational research; they offer a focus on perceptions as theoretically relevant and offer practical and conceptual advantages that cannot be replaced by other methods (
31 ). The organizational measures used in our study have been used in nearly 75 studies and shown to be reliable and valid. Although the study data are from 1999, this study provides one of the first impressions of the relationship between the inpatient psychiatric care environments in general hospitals and the occurrence of adverse events.
Conclusions
Progress in formal quality and safety improvement for inpatient psychiatric services has been extremely slow (
32 ). Not until 2008 were quality indicators implemented for inpatient psychiatric care by the Joint Commission (
33 ). Promising models of quality improvement are being utilized in general hospital psychiatric services. However, a dearth of such studies in the literature indicates the need for evidenced-based quality improvement models for inpatient psychiatric care. Findings from our study show adverse events to be prevalent in general hospital inpatient psychiatric care and contextual factors significantly associated specifically with the frequency of patient falls and work-related staff injuries. These findings are the tip of the iceberg of safety and quality challenges that remain a national priority. Advancing a quality and safety research agenda for inpatient psychiatric care in general hospitals will guide practice, improve care, and help ensure efficient and effective care. Complicated problems such as the provision of acute psychiatric hospital services require solutions that incorporate depth and breadth of understanding the complexities of acute mental illness as well as changes in prevailing attitudes and systems.
Acknowledgments and disclosures
This work was supported by grant R01-NR-004513, "Outcomes of Hospital Staffing," to Dr. Aiken, principal investigator.
The authors report no competing interests.