Older adults commonly experience depressive symptoms (
1,
2) with serious health consequences (
3–
6), although they underutilize mental health treatment (
7,
8). In attempts to explain this underutilization, theoretical frameworks have become increasingly complex, and the network-episode model (NEM) (
9–
11) has been recommended to guide this research (
12). The NEM emphasizes the dynamic nature of entry and exits in service systems over time and the influence of individuals' social context on service use, in addition to demographic, need, and attitudinal influences on the individual (
13). The purpose of this study was to examine individual and social covariates of mental health treatment utilization (prescription medication and psychotherapy) in a six-month longitudinal study with older adults who had depressive symptoms. Although the NEM also includes formal service system characteristics (such as colocation of services), their inclusion was beyond this study's scope.
At the individual level, several demographic variables are associated with older adults' lower treatment utilization, including older age, male gender, racial-ethnic minority status, and lower education (
14). Several practical barriers have been identified, including finances (
14–
16). Need (in regard to diagnosis, symptom severity, and disability) emerges as another important factor (
17–
20). Unfortunately, older adults with psychiatric disorders are less likely than younger adults to perceive a need for care (
19,
21); approximately half of these older adults do not perceive such need (
21,
22). Stressful life events may heighten older adults' perception of need and increase their use of treatment to address the stressors (
23,
24). Related to attitudes, older adults' prior experiences with mental health services and their intentions about initiating treatment also likely influence utilization, such that individuals with prior experience and intention to seek treatment are more likely to use it (
9–
11).
In regard to social context, research on social networks has yielded contradictory findings, most likely because of a focus on network structure (such as size of network) as opposed to messages individuals perceive from their social network (
9). For example, an older person's perceptions of negative views from society regarding mental illness (that is, stigma) (
25) are thought to serve as a barrier to initiation and continuation of services (
26,
27). Advice from persons in the individual's social network may increase use of general medical service by up to fivefold (
28), although advice was associated with lower mental health treatment utilization for older adults in one study (
29). That study did not assess the content of advice, although another study suggested that older adults may receive less advice than middle-aged adults encouraging them to use mental health services (
30).
Prior research has examined subsets of these factors, but experts have called for more complex, longitudinal designs to capture the dynamic process (
9,
13). Most NEM studies have been cross-sectional or retrospective (
31–
37), and the optimal length of prospective study for identifying service use changes is unknown. One previous longitudinal study based on the NEM assessed service use by older adults with depression for six months after discharge from a psychiatric hospitalization. Using monthly time increments, the authors identified several utilization patterns based on types and number of services delivered (
38).
The aims of this study were to describe mental health treatment utilization patterns over a six-month period and identify factors associated with utilization. The study was guided by the NEM for older adults with a range of mild to severe depressive symptoms. It was hypothesized that personal characteristics (demographic variables age, sex, race-ethnicity, education, and income; need-based indicators, such as diagnosis, symptom severity, disability, perceived need for treatment, and stressful life events; prior treatment experience; and intention to seek treatment) and social context variables (stigma and advice) would be associated with treatment use (psychotropic medication or counseling) over the six-month period.
Methods
Sample
Participants were 144 community-dwelling older adults with depressive symptoms (
Table 1). They were recruited from the Florida BRITE (Brief Intervention and Treatment for Elders) Program (
39), a statewide program providing outreach, screening, and brief interventions for substance misuse (alcohol, illicit drugs, and medications). BRITE providers do not offer treatment for depression, but they screen for depression and suicide risk as possible signs of undetected substance use. For cases with positive depression screens (≥5 on the Short Geriatric Depression Scale [S-GDS]) (
40) in the absence of substance misuse (three or more drinks per week, two or more drinks per day, or any illicit substance use), BRITE providers refer individuals to local mental health services. These individuals were recruited for this study at the five original BRITE sites (Broward, Duval, Hillsborough, Orange, and Pinellas Counties of Florida) and the University of South Florida research site with similar methods in both the community and medical settings (
39). Screening personnel were instructed to approach for this study all individuals found ineligible for BRITE services. Additional eligibility criteria for this study were age ≥65, ability to speak English, and a score ≥3 on a six-item cognitive screen (
41). Also, participants were excluded if they were receiving specialty mental health services (specifically, psychotropic medication from a psychiatrist or psychotherapy) to focus our examination on initiation of specialty services. Participants were included if they reported being prescribed antidepressants by primary care professionals, because this treatment was not considered specialty mental health treatment. Data were not collected by BRITE screening personnel in regard to who refused the screening, who was ineligible, or who refused participation.
Fourteen participants enrolled in the study dropped out over the study period (seven were no longer interested, three died during the course of the study, three became ill, and one left for unknown reasons), four of whom were not included in the final sample because they contributed data only at baseline. After completely describing the study, we obtained written informed consent from participants.
Measures
Demographic information.
Participants reported their age, gender, race and ethnicity, years of education, marital status, living arrangements, annual household income (based on the 2008 federal poverty level for comparison with other research and policies), insurance status, and perceived health status.
Structured Clinical Interview for DSM-IV Diagnosis Axis I (SCID).
Current major depressive episode and dysthymia were assessed with the SCID (
42). To minimize participant burden, other modules of the SCID were not administered. Diagnoses were determined by team consensus (interviewer, project coordinator, and principal investigator, who is a licensed psychologist).
S-GDS.
The S-GDS (
40) includes 15 yes-no items and has very good validity and reliability. Scores range from 0 to 15, with higher scores representing more severe depressive symptoms. Scores of 5–9 suggest mild to moderate depression, and scores ≥10 suggest severe depression.
World Health Organization Disability Assessment Schedule-II (WHODAS-II).
The WHODAS-II (
43) is a cross-cultural measure to assess disability across six domains: communication, getting around, self-care, getting along with people, life activities, and participation in society. It has good reliability and validity, and possible scores range from 0 to 100, with higher scores indicating greater disability. The 12-item version was used.
Geriatric Adverse Life Events Scale (GALES).
The GALES (
24) was developed and validated to assess stressful life events for older adults and includes 26 events (including retirement, new illness, and death of spouse). At baseline, questions were asked about events over the past year. For each event, follow-up questions assessed degree of stress (not at all, somewhat, or very) and impact on mood (much better, better, the same, worse, or much worse). Scores on the former could range from 0 to 78, with higher scores indicating more stress; scores on the latter could range from 0 to 130, with higher scores indicating worse mood.
Perceived current problem and need for treatment.
Participants were asked, “Are you currently experiencing an emotional or mental problem?” If they responded yes, they were asked, “Do you feel like you need help for this problem currently?”
Professionals seen in the past year.
Participants were presented a list of professionals (psychologist, therapist, or counselor; social worker or case manager; psychiatrist; other physician; nurse; faith leader; or other) and asked, “In the past, did you ever talk to any of these professionals about feelings of stress or sadness?” Follow-up questions were asked about timing of visits with these professionals. Yes-no responses were coded yes if the participant reported talking with one or more of these professionals within the past 12 months.
Current psychotropic medication.
Participants were asked whether they were “currently taking any medication prescribed by a doctor for depression, stress, nerves, moods, or anything similar.” This information was recorded to capture current medication use from nonspecialty physicians (such as a primary care provider). Participants were categorized as taking an antidepressant at baseline if they reported use of medications approved for depression (
44,
45).
Intention to begin new mental health service.
Participants were asked, “In the next month, do you plan to begin any new professional service to help deal with sadness, depression, or stress?”
Discrimination-Devaluation Scale (DDS).
The DDS (
46) assesses stigma, asking participants' perceptions of “most people's” attitudes about mental health problems. It includes 12 items, rated on a 6-point Likert scale (from 1, strongly agree, to 6, strongly disagree). Six items are reverse-scored, and total scores can range from 12 to 72, with higher scores representing greater stigma.
Advice to use or not use mental health services.
Participants were asked, “In the past month, has anyone given you advice to use any professional service to deal with sadness, depression, stress, or any other mental or emotional problem?” Participants were then asked about receipt of advice to “not use” services. Each of these items received a yes-no response.
Covariates at follow-up.
Covariates assessed at baseline that could change were repeated at each follow-up interview. Therefore, we repeated the S-GDS, GALES (time frame of past month), and the items concerning advice to use or not use mental health services.
Mental health treatment utilization in the past month.
At each follow-up, the interviewer read the same list of professionals presented at baseline and asked “Since last month, have you talked to any of these professionals about feelings of stress or sadness?” Follow-up questions asked about type, location, and frequency of treatment. Counseling was recorded if the person reported receiving psychotherapy, counseling, or talk therapy, regardless of number of sessions or professional type. They also were asked, “Since last month, were you taking any medication prescribed by a doctor or other health professional for depression, stress, nerves, moods, or anything similar?” Three variables for each follow-up period were derived to indicate receipt of counseling, antidepressant medication, or any formal treatment (counseling or antidepressant prescription).
Procedures
All procedures were approved by the University of South Florida Institutional Review Board. The baseline interview was conducted in person, and the six monthly follow-up interviews were conducted by telephone. All interviews were audiorecorded unless the participant refused. Each follow-up was considered on time if it was completed within a one-week window around the due date and was considered late if completed by two weeks after the due date. Sensitivity analyses comparing on-time and late interviews revealed no differences, so late interviews were included in all analyses. If a participant missed an interview, the interviewer contacted the participant for the remaining follow-up interviews unless the participant explicitly withdrew from the study. To minimize the amount of missing data resulting from missed interviews, the interviewer asked at the next follow-up only the treatment utilization questions for all monthly blocks since the last completed interview. Using a standard script, interviewers offered mental health referrals. [The script is available as an online supplement to this article at
ps.psychiatryonline.org.] All participants received referral information at baseline, and most received similar referrals at each follow-up; thus referrals were not analyzed. Data collection took place from December 2007 to August 2009.
Interviewers were counselors in the BRITE Program or trained research interviewers at the university. Supervised by the principal investigator, the project coordinator reviewed all baseline interviews, each interviewer's first seven follow-up interviews, and additional follow-up interviews as needed, resolving issues with the interviewer.
Data analysis
For aim 1, which was to identify patterns of treatment utilization, descriptive statistics were investigated for all variables. Utilization patterns were examined separately by symptom severity, although inferential statistics were not generated, given the small sample size. Participants were considered more likely to be in need of mental health treatment if they met criteria for major depressive episode or reported severe symptoms (S-GDS score ≥10), compared with those without a current major depressive episode and with an S-GDS score in the mild to moderate range (5–9 points). To assess covariates of treatment utilization over the six-month follow-up period (aim 2), logistic generalized estimation equations (GEEs) with robust standard errors were used with both time-constant and time-varying variables. We investigated unstructured, independent, exchangeable, and first-order autoregressive longitudinal correlational structures, using the quasi-likelihood criterion.
For the 42 individuals with one or more missing interviews, 21 missed the last follow-up. The treatment use questions were answered for the prior months in 17 interviews. No recall bias was noted based on GEE sensitivity analyses treating these data as missing, so these data were retained. Participants with one or more missing interviews did not differ on sociodemographic variables compared with those without missing interviews (p>.05), but they were more likely to have a current major depressive episode (39% versus 23%;
χ2=4.72, df=1, p=.03) and higher S-GDS (M=9.22±2.67 versus M=7.98±2.64; t=−2.53, df=142, p=.01) at baseline. All models were tested with Stata, version 11.1 (
47).
Results
Sample characteristics at baseline
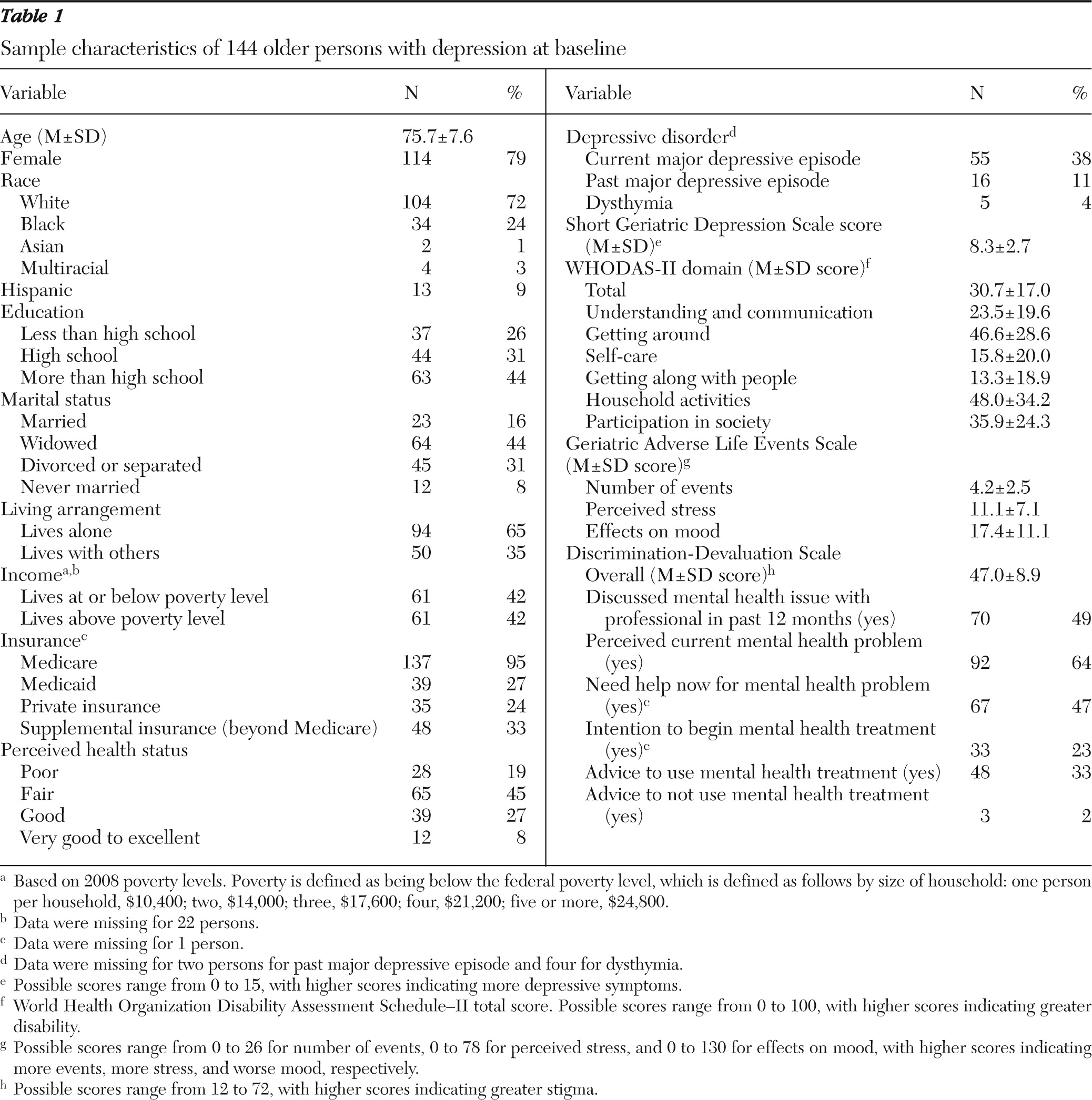
As shown in
Table 1, the mean age of participants was 75.7 years old. The largest proportions of the sample were female, white or black, had at least a high school education, were unmarried, lived alone, and perceived themselves to be in fair health. Thirty-eight percent of participants reported symptoms consistent with a current major depressive episode, with the mean S-GDS score in the mild to moderately depressed range (mean score of 8.3).
Aim 1: identify treatment utilization patterns
Approximately half of the sample received no formal treatment during the study period (N=70, 48%). Of those who received no treatment at baseline, more initiated new treatment earlier (by follow-up 1 or 2; N=35 of 117, 30%) than later (by follow-up 3 or later; N=12 of 117, 10%).
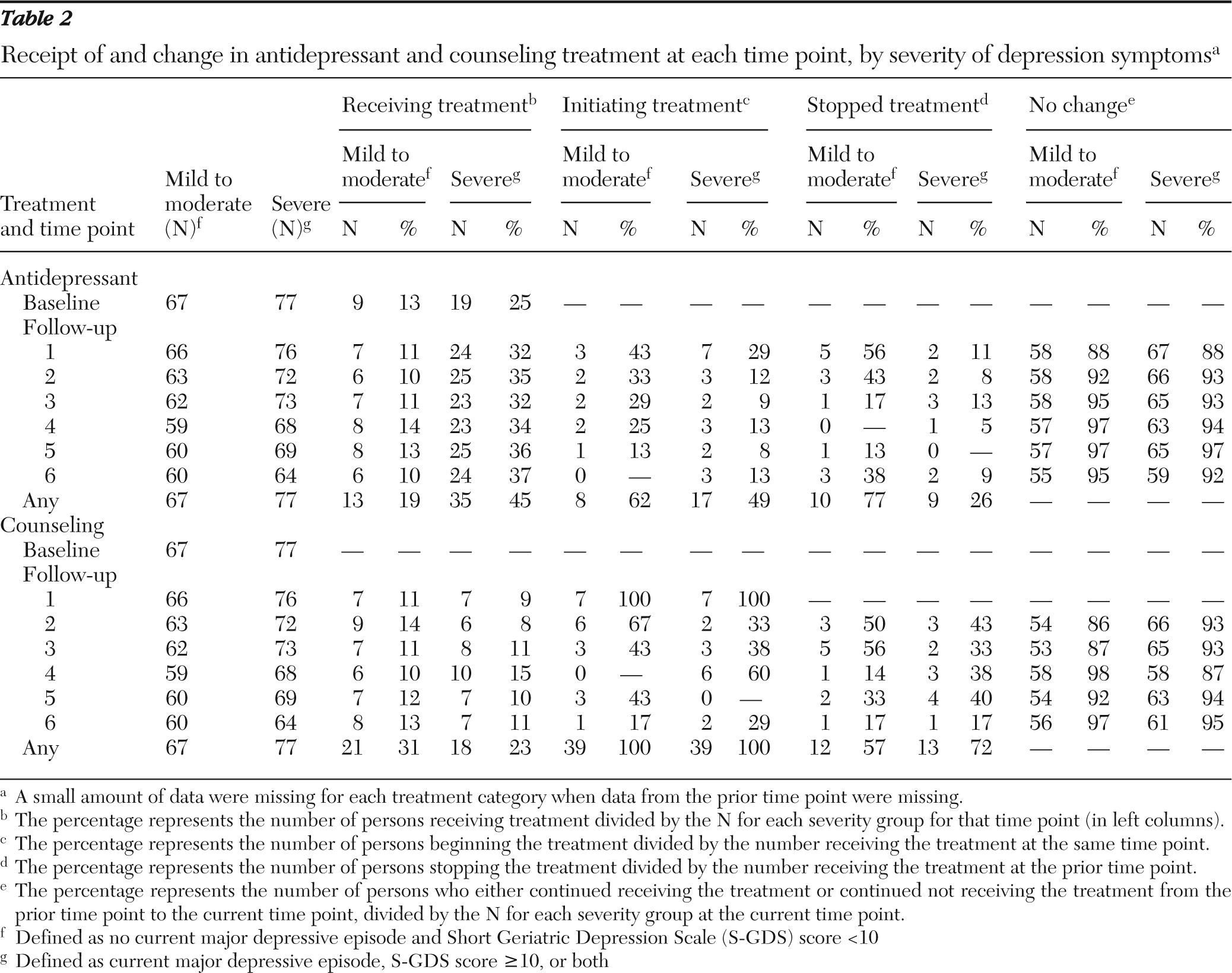
Details regarding use of antidepressants and counseling by severity of depression are presented in
Table 2. More participants with severe symptoms received antidepressants (25%–37%) than those with milder symptoms (10%–14%), although more with milder symptoms started (62% versus 49%) or stopped antidepressants (77% versus 26%) at least once. Fewer individuals received counseling overall, with no clear patterns by symptom severity.
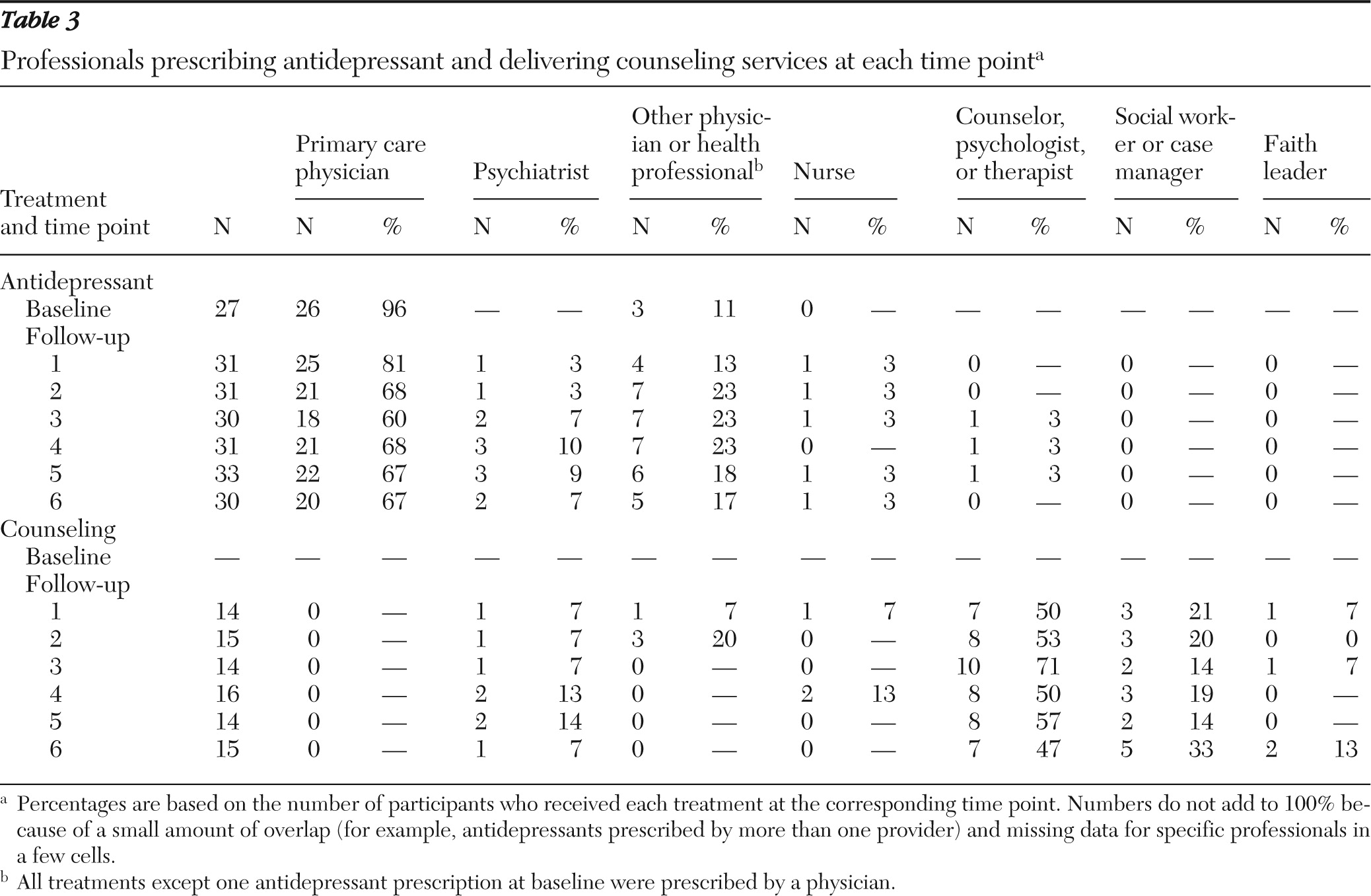
Table 3 displays information regarding professionals reported as prescribing antidepressant medications or delivering counseling. The most common treatment across all time points was antidepressant medication prescribed by primary care physicians. Counseling was delivered most frequently by a psychologist or therapist or by a social worker or case manager.
Aim 2: identify covariates of treatment utilization
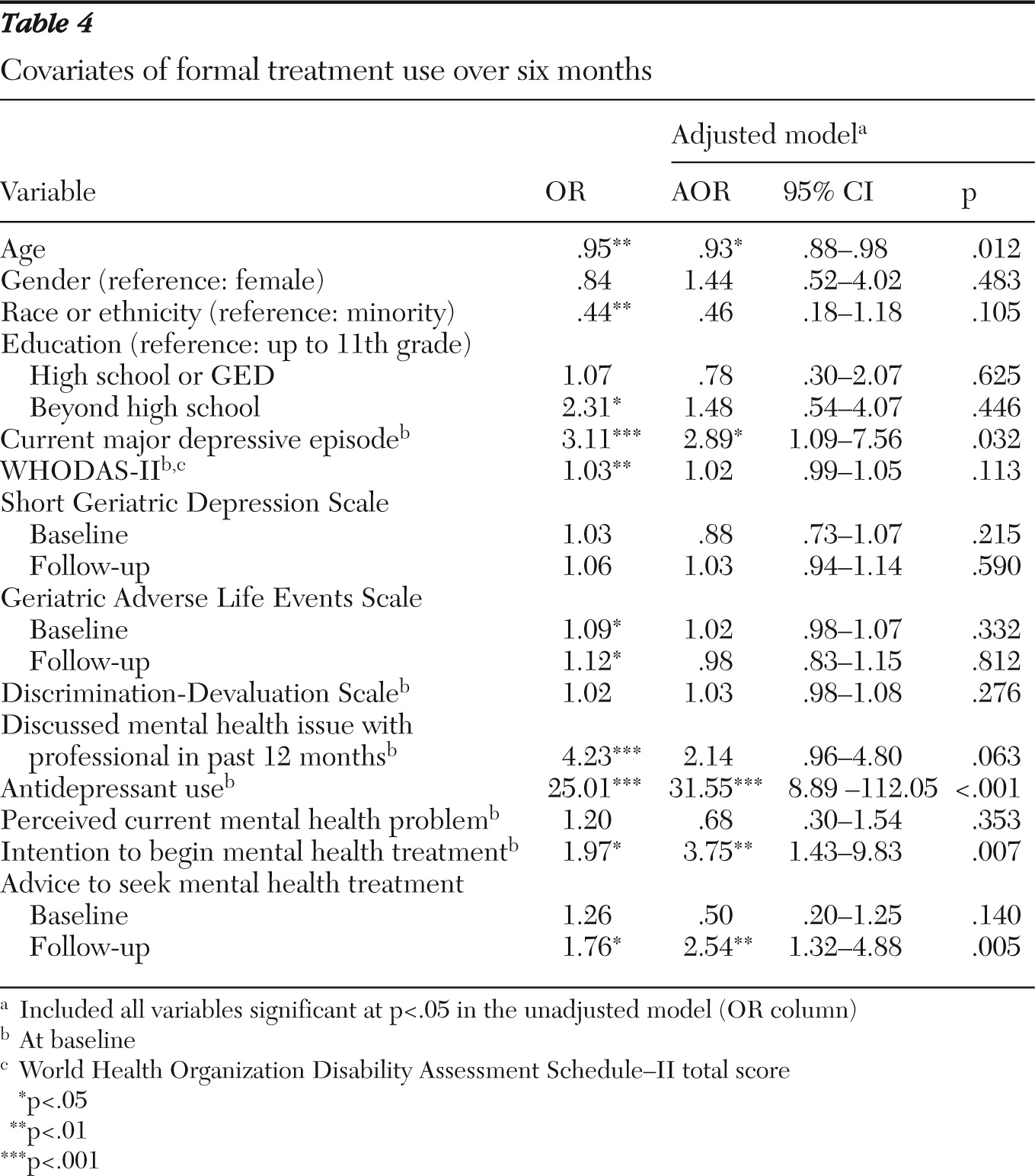
For the GEE analysis (
Table 4), the autoregressive correlational structure was used. After controlling for baseline antidepressant use, the analysis showed that younger age, baseline current major depressive episode, intention at baseline to seek treatment, and indication at follow-up of receipt of advice were significantly associated with increased odds of treatment utilization.
Discussion
Related to aim 1, the main finding was that most older adults with depressive symptoms changed little in their use or nonuse of mental health treatment over a six-month period. Approximately half of participants received no formal treatment, and participants tended to start a new treatment early in the follow-up period or not at all. Compared with those with less severe symptoms, more participants with severe symptoms or a current major depressive episode received antidepressants, and they also appeared to use their treatment more consistently, starting or stopping antidepressants less often overall. Regarding aim 2, partially consistent with the hypotheses, participants were more likely in controlled analyses to use treatment during the follow-up period if they were younger, had a current major depressive episode at baseline, were receiving an antidepressant at baseline, intended at baseline to initiate treatment, and reported at follow-up receipt of advice to find mental health treatment.
This study extends prior cross-sectional research (
19,
48) by demonstrating relative stability over a six-month period. A strength of this study is that assessments were monthly, a frequency that can enhance recall accuracy. Longer study periods may be needed, however, to observe critical periods when older adults make changes in utilization.
The covariates of treatment use were not surprising, again extending prior studies and consistent with the NEM (
10), with key demographic (age), need (major depressive episode diagnosis), attitudes (intention), prior experience (antidepressant use), and social context (advice) as important factors (
14,
19,
48,
49). Stigma was not associated with treatment utilization, which could be due to its measurement, statistical power, the possibility that stigma was not as salient for this sample as it would be for a more severely depressed sample (
25), or the possibility that stigma is not as significant a barrier as previously suggested (
50). Consistent with the NEM, advice encouraging individuals to use treatment was associated with use. One positive finding was that almost no participants received advice discouraging use of treatment. Indirectly related to the social context, the observation that participants who initiated treatment tended to do so early in the study period suggests that something about joining the study may have triggered use, such as awareness of symptoms due to the screening or referrals.
Several limitations affect the generalizability of the findings. First is the lack of information regarding refusals to participate in the study. Additional selection biases may have occurred as a result of using community-based outreach recruitment methods, because we restricted the study to English-speaking individuals, and because the study included individuals who received antidepressants from primary care physicians instead of from only those who obtained prescriptions from psychiatrists and included participants with a range of depressive symptoms. Thus formal mental health treatment was not indicated in all cases, although their inclusion allowed us to explore associations of severity with treatment use. Although the finding was statistically inconclusive given the sample size, participants with less severe depressive symptoms started and stopped antidepressant medication more frequently than those with more severe symptoms. These patterns may reflect overuse or inconsistent use that is not likely to be therapeutic—a possibility that warrants further research. Reasons for utilization could elucidate these patterns; unfortunately data were not available regarding participants' perceived reasons for starting and stopping treatment.
Conclusions
Over a six-month period, most older adults with depressive symptoms in this study either continued their use of mental health treatment or did not use services or antidepressants at all. Age, prior treatment experience, current need, intention to initiate treatment, and receipt of advice emerged as the most critical covariates of treatment utilization. Strengths of this study included its comprehensive assessment of covariates of treatment utilization, which was accomplished with a longitudinal design and a complex theoretical framework. Future research will likely need to approach this complex, dynamic phenomenon of utilization patterns with mixed quantitative and qualitative methods. For example, quantitative studies such as this one that include a comprehensive number of covariates of treatment use may suggest factors that may be important influences on treatment utilization, such as advice from others. In-depth analysis of subsets of these factors is also needed to fully understand how they may influence utilization and how they may inform interventions. For example, this study's findings suggest the need for in-depth, qualitative assessment of factors such as intentions (that is, what is intended and specificity of plan), advice (from whom, how it is delivered, how it facilitates or hinders treatment seeking, and how advisors might be included to facilitate treatment), and open-ended questions regarding decisive factors that may be somewhat idiosyncratic.
Acknowledgments and disclosures
This study was funded by grant R03MH77598 from the National Institute of Mental Health. This study was conducted in collaboration with the Florida Brief Intervention and Treatment for Elders Program, which is supported by grant LD815 from the Substance Abuse and Mental Health Services Administration to the State of Florida Department of Elder Affairs.
The authors report no competing interests.