We evaluated cognitive functioning in two homogeneous groups of schizophrenic patients with different durations and severities of illness. Early age at onset has been associated with worse performance on some cognitive measures
(6). Accordingly, we predicted that 1) male patients would demonstrate greater impairment than female patients, and 2) no sex differences in cognitive functioning would emerge after control for age at onset.
METHOD
Cohort 1. Inpatients consecutively admitted to an acute research unit for first-episode schizophrenia in Stony Brook, N.Y. (N=58; 41 men, 17 women), gave written informed consent for participation, as previously detailed
(7). All patients met DSM-III-R criteria for chronic schizophrenia at 2-year follow-up. The mean age for men was 25.8 years (SD=6.2), and for women, 30.4 (SD=8.0); the mean ages at onset of psychotic symptoms were 24.2 (SD=5.6) and 29.8 years (SD=7.8), respectively.
Cohort 2. Chronic inpatients from Napa State Hospital (N=74; 51 men, 23 women) with a DSM-III-R diagnosis of schizophrenia gave written informed consent for participation (previously detailed
[6]). The mean age for men was 35.1 years (SD=8.3), and for women, 40.3 (SD=9.5); the mean ages at onset were 16.6 (SD=4.2) and 20.3 years (SD=4.9), respectively. Thus, this cohort had been ill for an average of 18.9 years (SD=7.9).
Patient groups were rated with the Brief Psychiatric Rating Scale (BPRS)
(8) within 2 weeks of testing. Negative symptom and positive symptom scales were constructed as described previously
(6). There was a statistically significant group-by-sex interaction for positive symptoms (F=5.6, df=1, 118, p<0.02); post hoc Tukey tests indicated that chronically ill men had higher scores than women (p<0.03). There were no significant differences in chlorpromazine or benztropine equivalents between sexes in either cohort.
A normal comparison group (N=74; 56 men, 18 women; mean ages=32.1 [SD=9.6] and 24.2 years [SD=4.9], respectively) was recruited from the community near cohort 1, gave written informed consent, and was screened with structured psychiatric interviews
(9).
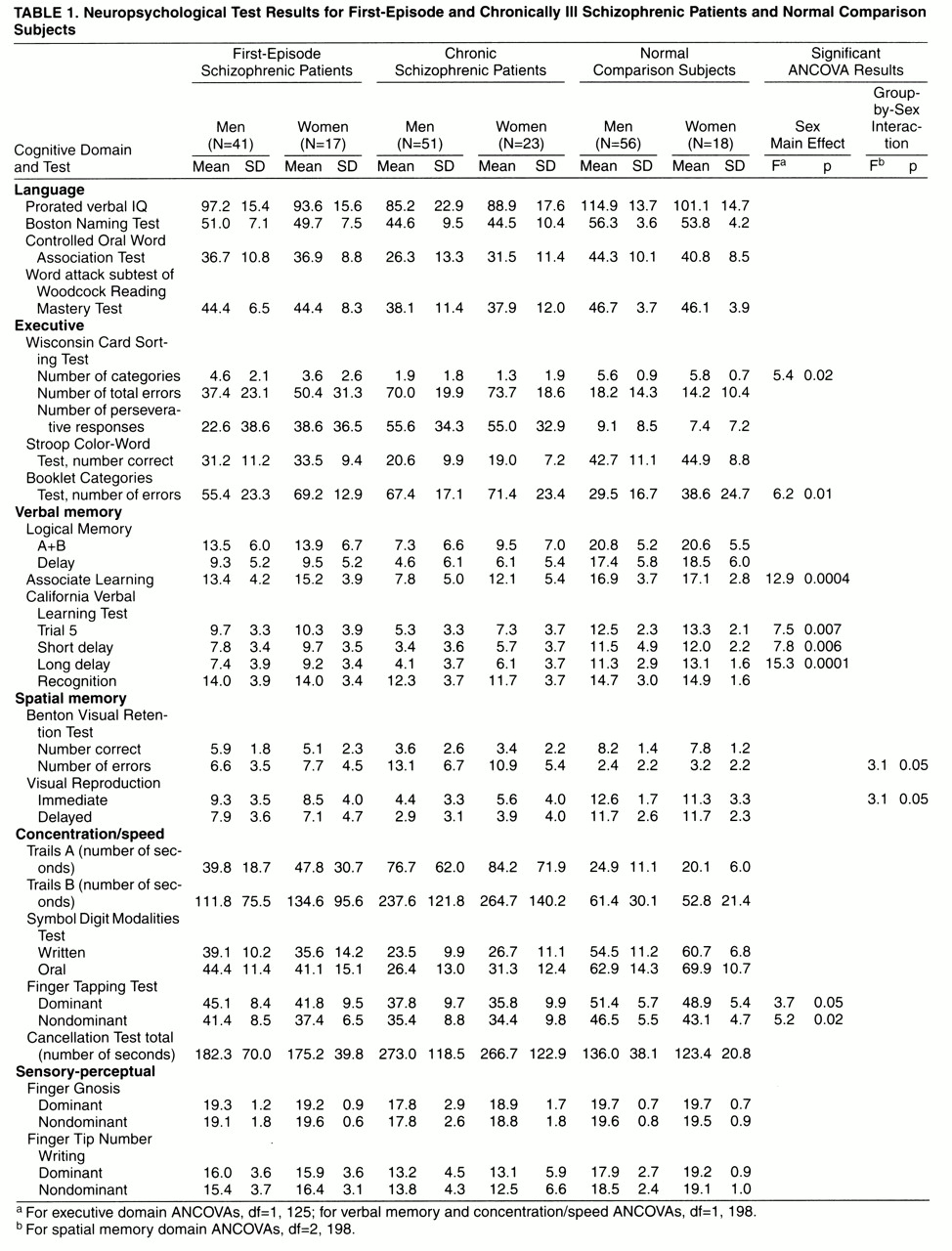
A battery of tests measuring different cognitive domains was administered to all three groups
(9). In order to control for differences between patient and comparison groups on demographic variables known to influence test performance, we performed group-by-sex multivariate analyses of covariance (MANCOVAs) on dependent measures from six cognitive domains, using age and the Reading score from Wide-Range Achievement Test—Revised (WRAT-R) as covariates. WRAT-R Reading score has been shown to be the best measure of premorbid intellectual functioning in psychotic disorders
(10). All tests contributing to each domain are listed in
table 1. Analyses were repeated with age at onset as a third covariate. When the overall MANCOVA was statistically significant, univariate tests (analyses of variance) were performed.
RESULTS
There were statistically significant group effects for all cognitive domains (p<0.0001), indicating that schizophrenic patients performed worse than the comparison group. There were also overall main effects for sex in executive (F=2.8, df=5, 194, p<0.02), verbal memory (F=3.4, df=7, 192, p<0.002), spatial memory (F=3.6, df=4, 195, p<0.008), and concentration/speed (F=2.0, df=7, 192, p<0.05) domains. Men performed better than women in all domains except verbal memory, where women performed significantly better.
There were statistically significant group-by-sex interactions for spatial memory (F=2.1, df=8, 390, p<0.03) and sensory-perceptual (F=2.0, df=8, 390, p<0.05) domains. Univariate tests revealed statistically significant interactions for number of errors on the Benton Visual Retention Test (F=3.1, df=2, 198, p<0.05) and immediate score on Visual Reproduction (F=3.1, df=2, 198, p<0.05). Post hoc analyses indicated that chronically ill men were more impaired than women on the Benton Visual Retention Test (Tukey’s honestly significant difference, p<0.02). For the sensory-perceptual interaction, none of the univariate analyses of covariance (ANCOVAs) was statistically significant.
When MANCOVAs were repeated with age at onset added as a covariate, both spatial memory (F=2.6, df=4, 122, p<0.04) and sensory-perceptual (F=2.4, df=4, 122, p<0.05) MANCOVAs remained statistically significant. However, only the univariate test for the Benton Visual Retention Test reached statistical significance (F=5.5, df=1, 125, p<0.02), with chronically ill schizophrenic men having significantly more errors on the test than chronically ill women (Tukey’s honestly significant difference, p<0.03).
Because male chronic schizophrenic patients demonstrated significantly greater positive symptoms than women and because some BPRS positive and negative symptom scales correlated with spatial memory tests, ANCOVA analyses were repeated with positive and negative symptoms added as covariates for each spatial memory variable. There were no significant differences between the sexes on these ANCOVAs.
DISCUSSION
Contrary to our prediction, chronically ill schizophrenic men were more impaired than women on measures of spatial memory after control for differences in age at onset. However, those differences were eliminated after symptom differences between men and women were taken into account. Thus, we found no sex differences in cognitive functioning in two groups of schizophrenic patients, a first-episode cohort and a severely ill group, after taking into consideration normally occurring sex-related differences in cognitive abilities, age at onset, and symptom expression. Consistent with the literature on general sex differences in cognitive abilities
(11), men performed better than women on measures of spatial memory, spatial problem-solving ability, and pure motor speed, while women were superior to men on verbal memory.
Controlling for differences due to sex-related symptomatic expressions of the illness biases the results against finding a sex difference in cognition. However, if differences in cognition between male and female schizophrenic patients are due to differences in symptoms themselves or time at onset, then cognitive sex differences in schizophrenia may reflect symptom variation and onset differences between the sexes. Identifying causes for differences on these measures may elucidate the neurodevelopmental and pathophysiological underpinnings of schizophrenia.