Over the last 15 years, women have changed the face of homelessness. Families now constitute 36.5% of the homeless population
(1). Studies have documented elevated rates of mental illness and substance use disorders among homeless women in relation to the general population, but estimates are inconsistent
(2–5), in part, because of methodological differences
(6, 7). These studies of homeless women rarely distinguish between women accompanied by children (“mothers”) and those who are alone (“solitary”). Although the majority of both groups have children, many solitary women have lost their children because of mental disorders.
Homeless solitary women have higher rates of schizophrenia, bipolar disorder, and substance use disorders than homeless mothers do
(7). Zima et al. found that 72% of homeless mothers had a probable lifetime substance use disorder, mental disorder, or both
(5). In contrast, the National Longitudinal Alcohol Epidemiologic Survey reported that the percentage of welfare recipients with substance use disorders was similar to the percentage in the general population
(8). In general, homeless mothers have higher rates of major depression
(4, 5) and substance use disorders
(3–5) than the general population.
Dual diagnoses (i.e., mental illness and substance abuse) and the presence of two or more lifetime conditions have also received increased attention. Among homeless solitary women, approximately half have a dual diagnosis. For participants in the National Comorbidity Survey, 52% had no mental disorders over their life spans, while 21% had one lifetime disorder and the remaining 27% had two or more lifetime disorders
(9).
To address the lack of research on homeless and low-income mothers, in this article, we used the Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP)
(10) to determine lifetime and current prevalence of DSM-III-R axis I disorders among 220 homeless and 216 low-income housed mothers. We also compared prevalence rates among these low-income mothers to the rates among women from the general population, aged 15–40, in the National Comorbidity Survey.
METHOD
Sampling and data collection procedures have previously been described
(11, 12). We employed an unmatched case-control design. We enrolled homeless single mothers (N=220) from all nine emergency shelters in Worcester, Mass., and a comparison group of single mothers (N=216) receiving public assistance (Aid to Families With Dependent Children) who had never been homeless. The age, income, and number of children of our combined group were similar to the data for low-income women in other U.S. cities. However, reflecting Worcester’s population, our group had more Puerto Rican and fewer African American women than are found in many other midsize cities.
We obtained written informed consent from all mothers in our group. We collected data over three to four sessions (6–7 hours). The SCID-NP
(10) assessed mood, anxiety, somatization, and substance use disorders according to DSM-III-R criteria. We also asked questions from the SCID-NP that screen for psychosis. When the results were positive, the patient version of the SCID determined the specific disorder. The interviewers, extensively trained in the administration of the SCID-NP, interviewed both subgroups.
We compared, to the extent possible, the prevalence rates of disorders in our sample with comparable DSM-III-R rates for all women in the National Comorbidity Survey
(9). The National Comorbidity Survey interviewed a stratified, multistage sample of 8,098 individuals aged 15–54 years but excluded homeless persons. The National Comorbidity Survey used a modified version of the Composite International Diagnostic Interview, which is designed to be used by trained interviewers who are not clinicians. Overall reported prevalence rates from the National Comorbidity Survey were weighted to adjust for household size, nonresponse, and poststratification. Various diagnoses (e.g., certain substance use disorders, posttraumatic stress disorder [PTSD]) made in the National Comorbidity Survey were not available for secondary analyses, which limited our ability to make comparisons for these particular disorders as well as for summary diagnoses that spanned diagnostic categories. We limited the National Comorbidity Survey subjects to women aged 15–40 years and achieved approximate comparability between the two study groups at each quartile of their respective age distributions. We analyzed data by using t tests for continuous variables and chi-square tests for discrete variables. Statistical significance was tested with alpha set at 0.05 (two-tailed).
RESULTS
Characteristics of Homeless and Housed Mothers and Participants in the National Comorbidity Survey
The approximate mean age of the Worcester group and the National Comorbidity Survey sample was 27 years (range=15–58). More than half the homeless and housed subjects were Hispanic and African American, whereas 71% of National Comorbidity Survey participants were white. Less than 6% of the low-income women were married compared to 50% of the National Comorbidity Survey women. The median annual income of the National Comorbidity Survey participants was approximately $36,000, with 73% earning more than $15,000. In contrast, the median incomes of the homeless ($8,500) and housed ($8,500) mothers were well below the poverty level. More than 40% of the National Comorbidity Survey group had 13 or more years of education compared to 11% for the homeless and 18% for the housed women.
Homeless and housed women had an average of 2.2 children. Most were receiving support from Aid to Families With Dependent Children, and more than two-thirds had previously worked. Both groups were socially isolated. As previously reported, histories of childhood physical abuse, sexual abuse, or both and more recent partner violence were pervasive: nearly 88% of the homeless and 79% of the housed women had been violently victimized at some point in their lives
(11).
Lifetime and 1-Month Prevalence
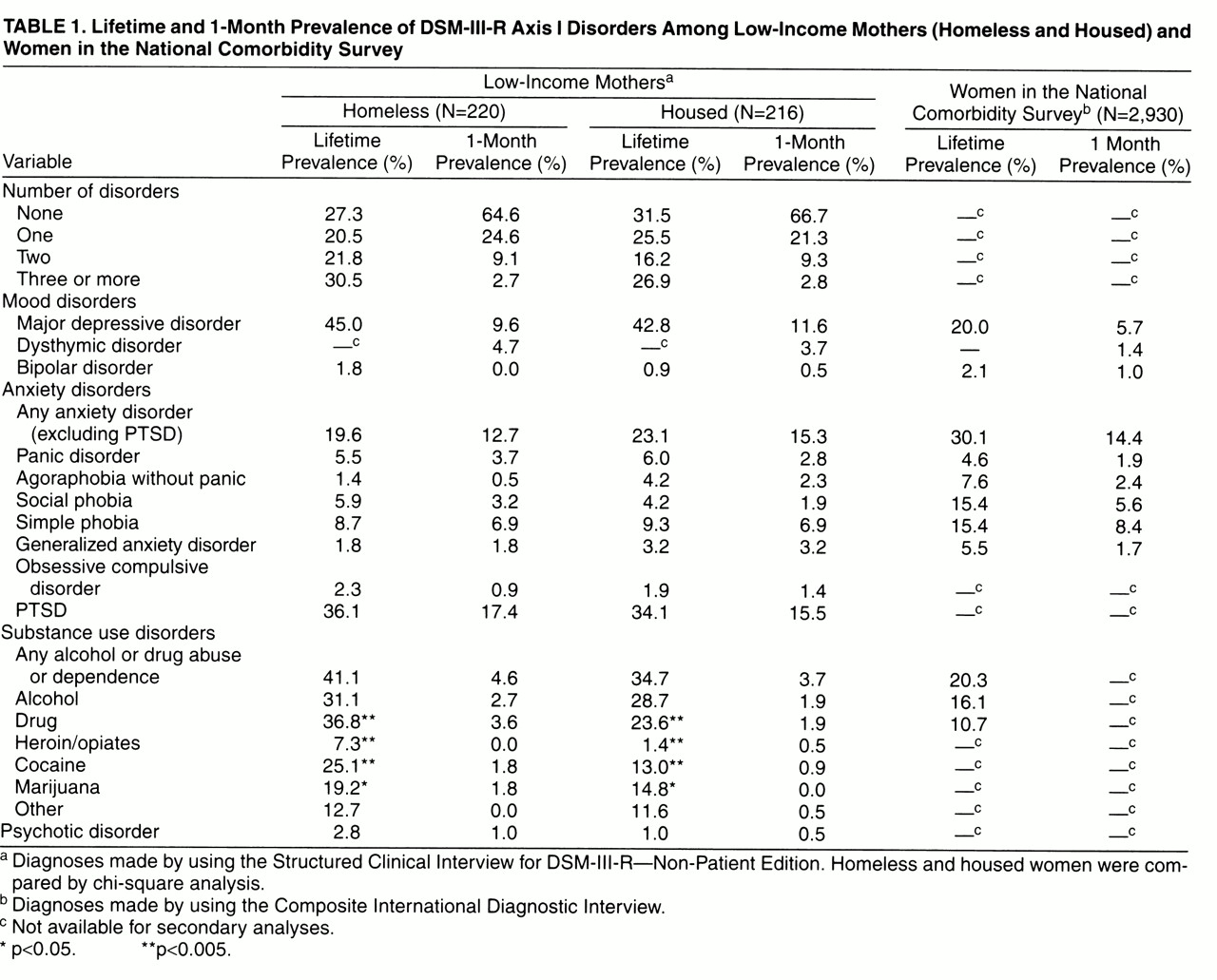
More than two-thirds of respondents had at least one lifetime diagnosis (see
table 1). The distribution of the diagnoses was similar among both groups. PTSD, major depression, and substance use disorders were disproportionate among low-income mothers when compared with National Comorbidity Survey respondents
(9, 13). Approximately 35% of low-income women had lifetime PTSD, a rate about three times that of women of all ages (not just women 15–40 years) in the National Comorbidity Survey
(13). The rate of major depression among low-income women was about twice that of women 15–40 years in the National Comorbidity Survey population. Of the anxiety disorders among low-income women, only panic was elevated when compared with data from the National Comorbidity Survey. Psychotic disorders were not overrepresented among our study participants. Lifetime prevalence of alcohol-related disorders among these low-income mothers, however, was almost twice as high and other forms of drug abuse were nearly three times as high as comparable disorders in the National Comorbidity Survey.
With regard to current (i.e., 1-month) prevalence rates, almost two-thirds of homeless and housed mothers had no diagnosis, one-fourth had one, and 12% had two or more diagnoses. Current rates of homeless and housed mothers were similar. PTSD was most common. Major depression occurred approximately twice as often as in the National Comorbidity Survey.
Two or More Lifetime and Current Co-Occurring Disorders
Since we did not know the onset of all lifetime disorders, we distinguished between two or more lifetime disorders and two or more current co-occurring disorders. When we considered lifetime diagnoses, 31% of homeless and housed mothers had none, 23% had one, and 47% had two or more disorders over their life spans. Of those with at least one psychiatric condition, 67% had two or more lifetime diagnoses—a prevalence similar to that of the National Comorbidity Survey group
(9). Of women with two or more disorders, 89% had a substance use disorder, 85% had PTSD, 73% had depression, and 71% had an anxiety disorder. Ten percent of the Worcester group had two or more current co-occurring disorders. The most common co-occurring disorders were major depression, substance use disorders, anxiety, and PTSD. No significant differences existed between the homeless and housed groups.
DISCUSSION
This is the first study to date that documents the prevalence (lifetime and 1 month) of psychiatric and substance use disorders among homeless and low-income housed mothers and compares it to the prevalence of such disorders among women in the general population. More than two-thirds of the mothers in our study had a lifetime diagnosis of at least one axis I disorder, and almost half had two or more lifetime disorders. Contrary to reports citing mental disorders as a cause of homelessness, DSM-III-R diagnoses were not associated with current housing status among this group of low-income mothers with dependent children.
Unlike solitary homeless women, homeless mothers do not suffer disproportionately from schizophrenia
(7). However, lifetime rates of PTSD, major depression, and substance use disorders are overrepresented when compared with rates for the National Comorbidity Survey. With regard to lifetime history of mental disorder, approximately two-thirds of those with diagnoses had two or more lifetime disorders. The rate of two or more current disorders was far lower, with substance abuse most likely to be one of these current (and lifetime) conditions.
Violence has been recognized as a subtext of family homelessness
(11, 13). A high percentage (83%) of low-income women in Worcester had been physically or sexually assaulted during their life span
(10). Thus, it is not surprising that PTSD, substance use disorders, and major depression were disproportionately represented with lifetime rates of PTSD three times greater than in the general female population.
Various limitations must be considered. This study was conducted in one locale and can best be generalized to midsize American cities. We did not determine axis II diagnoses. Because of resource limitations, we did not assess interrater reliability among interviewers. Recall bias also is an issue in conducting lifetime assessments, but is almost always in the direction of underreporting. Current substance use may have been underdiagnosed since Worcester’s shelters do not accept women who are active users. While our study and the National Comorbidity Survey used identical diagnostic criteria, different assessment instruments were used in the two studies; the difference in instruments made comparison of results slightly more problematic than if the same diagnostic device had been used. Finally, not all National Comorbidity Survey variables were available to us for secondary analyses, limiting our ability to make comparisons for certain diagnoses and across diagnostic conditions.
Our findings support Belle’s argument that psychiatric disorders are more common among women in lower socioeconomic groups, largely because of the multiple stressors associated with poverty
(14). Pervasive violence in the context of poverty may account for many of the emotional disorders in our group, particularly the disproportionately high rates of PTSD. Only by acknowledging the bleak reality of poor women’s lives, especially the high rates of traumatization, can we improve their mental health and well-being.