Studies comparing the outcome of psychotic depression (depression with delusions or hallucinations or both) with that of nonpsychotic depression have produced conflicting results. Some studies have found that patients with psychotic depression have lower rates of recovery (
1–
3), more chronic symptoms (
3,
4), higher rates of relapse and recurrence (
5), and more frequent hospital admissions (
3–
6), whereas others have reported that the two groups do not differ in these outcomes (
7–
9). Several methodological factors limit the interpretation of these findings. First, since these were all naturalistic studies, adequacy of treatment, which has an important bearing on outcome, was not ensured. Second, studies evaluating relapse, recurrence, and rehospitalization included individuals whose depression had not remitted from the index episode. In studies in which subjects with psychotic depression had lower rates of remission, this could have biased the long-term outcome in favor of nonpsychotic depression, since incomplete resolution of an episode of depression is associated with an increased risk of relapse or recurrence (
10). Third, individuals with psychotic depression usually have more severe symptoms than those with nonpsychotic depression (
11). Greater severity of depression may independently predict worse response to treatment (
12,
13) and greater frequency of relapse and recurrence (
14). However, none of these studies controlled for the effect of severity of depression on outcome.
There have been few outcome studies specific to elderly patients with psychotic depression (
2,
6). The purpose of this research, therefore, was to further evaluate the long-term outcome of psychotic depression in late life. Patients with psychotic and nonpsychotic depression were compared on the frequency of relapse and recurrence and the cumulative probability of surviving 2 years without these events. We chose 2 years as the period of follow-up because this appears to be the time of greatest risk for relapse and recurrence following remission of an episode of depression in old age (
15). So as not to confound rates of relapse and recurrence, only individuals whose depression had remitted with acute treatment were entered into the follow-up study.
METHOD
Patient Selection
The study group was derived from subjects consecutively referred to the Geriatric Affective Disorders Program of The Toronto Hospital. Most referrals to this program are from family physicians or other primary care services. Men and women aged 60 years or older who met DSM-III-R criteria for unipolar major depression and had a score of 16 or more on the 17-item Hamilton Depression Rating Scale (
16) after at least 7 days without psychotropic medication were eligible for the study. Exclusion criteria were any other concurrent axis I diagnosis; a lifetime history of DSM-III-R-defined schizophrenia, schizoaffective disorder, paranoid disorder, or dementia; any neurological disorder affecting the central nervous system; acute, uncontrolled medical illness at the time of recruitment, although patients with stable chronic medical conditions could be included; or any condition that contraindicated the use of any of the study medications. Patients who had delusions or hallucinations or both (as defined by the Structured Clinical Interview for DSM-III-R [SCID] [17]) at index assessment were diagnosed as having a psychotic depression. After a complete description of the study to the patients, written informed consent was obtained.
Before treatment, patients underwent a psychiatric interview that employed the SCID, a physical assessment, routine blood work, and ECG. The Mini-Mental State (
18) was used to quantify cognitive function; however, a diagnosis of dementia, which was used to exclude patients from the study, was based on a comprehensive history and cognitive evaluation. In particular, no patient had cognitive impairment before the index episode of depression. Concurrent chronic medical problems were rated on the physical illness rating scale of Burvill et al. (
19).
Treatment Phases
Treatment consisted of two phases. The purpose of the first phase was to achieve remission of the index episode of depression. Patients with nonpsychotic depression were treated with nortriptyline, which was increased to a dose of 75 mg/day by the end of the first week. Plasma nortriptyline levels were determined at the end of the second week of treatment, and, if necessary, the dose was adjusted to achieve levels of 150–500 nmol/liter. Patients remained on a regimen of nortriptyline for 6 weeks from the time of its initiation. If patients failed to respond (response was defined as a Hamilton depression scale score of 10 or lower) by the end of the sixth week of treatment, they were then treated with 2 weeks of adjunctive lithium carbonate; a 12-hour postdose lithium plasma level of 0.5–1.0 mmol/liter was achieved by the end of the first week of augmentation. The recommended treatment for patients with psychotic depression was ECT, which was administered with a brief-pulse, constant-current device (MECTA SR-1). Patients were initially treated with fixed high-dose (375–500 millicoulombs), nondominant unilateral ECT three times a week. If there was no improvement (on the basis of the judgment of the study psychiatrist) in depressive symptoms after five treatments, electrode position was changed to bilateral. In the psychotic group, response was defined as a Hamilton depression score of 10 or lower and the absence of delusions and hallucinations, at which point ECT was discontinued. However, if, by the end of 12 treatments, patients had not responded and had failed to show ongoing improvement between treatments 10 and 12, ECT was discontinued at that point. If ECT-induced cognitive impairment severely interfered with the patient's functioning, the frequency of treatments was reduced to twice per week. Psychotically depressed patients who declined ECT were treated with 6 weeks of nortriptyline and perphenazine, followed, if necessitated by nonresponse, by 2 weeks of lithium augmentation. The dosing and duration of nortriptyline and adjunctive lithium were the same as those for patients without psychosis. Perphenazine was started at a dose of 4 mg/day and could be increased by 4–8-mg increments, up to every 4 days, depending on clinical response and side effects.
Patients whose depression remitted with treatment (the start of remission was defined as the point of response followed by at least 2 consecutive weeks of Hamilton depression scores of 10 or lower and, in the case of psychotic subjects, the absence of delusions and hallucinations) entered the 2-year follow-up phase. It should be noted that maintenance treatment was not restricted to patients with a prior history of depression. This decision was based on evidence that patients who experience a first episode of depression after the age of 60 years are also at high risk of recurrence of depression (
15). Patients continued to take the same dose of medication that led to response. Nortriptyline and lithium were continued throughout the study. However, in order to minimize the risk of tardive dyskinesia, perphenazine was withdrawn (by tapering the dose over a 4-week period) 16 weeks after the start of remission. For patients who responded to ECT, nortriptyline was titrated up to a therapeutic dose within 2 weeks after ECT was stopped. Patients who responded to ECT were not prescribed prophylactic antipsychotic medication or lithium. During this 2-year phase of the study, patients were followed on a monthly basis for clinical assessment of their mental state, medication side effects, and compliance with treatment. Plasma nortriptyline and, when applicable, lithium levels were determined on a periodic basis and were maintained in the range of 150–500 nmol/liter and 0.5–1.0 mmol/liter, respectively.
The outcome events of primary interest were relapse and recurrence of depression. Relapse was defined as the reemergence of depressive symptoms within 16 weeks of remission of the index episode of depression. Recurrence was defined as a new episode of depression occurring after at least 16 consecutive weeks without a relapse. Relapse and recurrence were diagnosed when the patient met symptomatic criteria for DSM-III-R major depression for at least 1 week and had a Hamilton depression score of 16 or above. Reemergence of psychotic symptoms was not required for the diagnosis of relapse or recurrence. If a patient required a change of treatment as a result of a relapse or recurrence, the change was made only after it was determined that she or he met the study's criteria for these events.
Statistical Analysis
Comparison of characteristics between groups was performed by t tests for continuous variables and chi-square analysis (or Fisher's exact test, when appropriate) for categorical variables. Long-term outcome was analyzed in two ways. First, the frequency of relapse and recurrence was compared by chi-square analysis or Fisher's exact test. Stepwise logistic regression analysis was then used to examine whether psychosis had an impact on the frequency of relapse or recurrence independent of other clinical variables. Second, survival methods (the Cox proportional hazards model and the Kaplan-Meier product limit method) were used to estimate the probability of a patient remaining well without relapse or recurrence during the 2-year follow-up. For all analyses, statistical significance was set at p≤0.05 (two-tailed tests).
RESULTS
Patient and Treatment Characteristics
Of the 283 patients initially evaluated, 126 (25 psychotic and 101 nonpsychotic) met entry criteria and entered the first phase of treatment. Of the psychotic group, 17 patients underwent ECT, and 15 (88.2%) responded (eight to unilateral ECT alone and seven to unilateral crossed over to bilateral ECT; mean number of treatments=9.7, SD=3.4). Eight psychotic patients opted for pharmacotherapy, and four (50%) responded (two to nortriptyline and perphenazine and two to these medications plus lithium). Thus, 19 (76.0%) of 25 psychotic patients responded to treatment of the index episode. Sixty-eight (67.3%) of the nonpsychotic group responded to treatment (61 to nortriptyline alone and seven to nortriptyline and lithium). In addition to having Hamilton depression scores of 10 or below, all responders had a 50% or greater reduction in baseline Hamilton depression scores. Psychotic and nonpsychotic groups did not significantly differ in the rate of attrition during treatment of the index episode (4.0% and 17.8%, respectively) (p=0.12, Fisher's exact test).
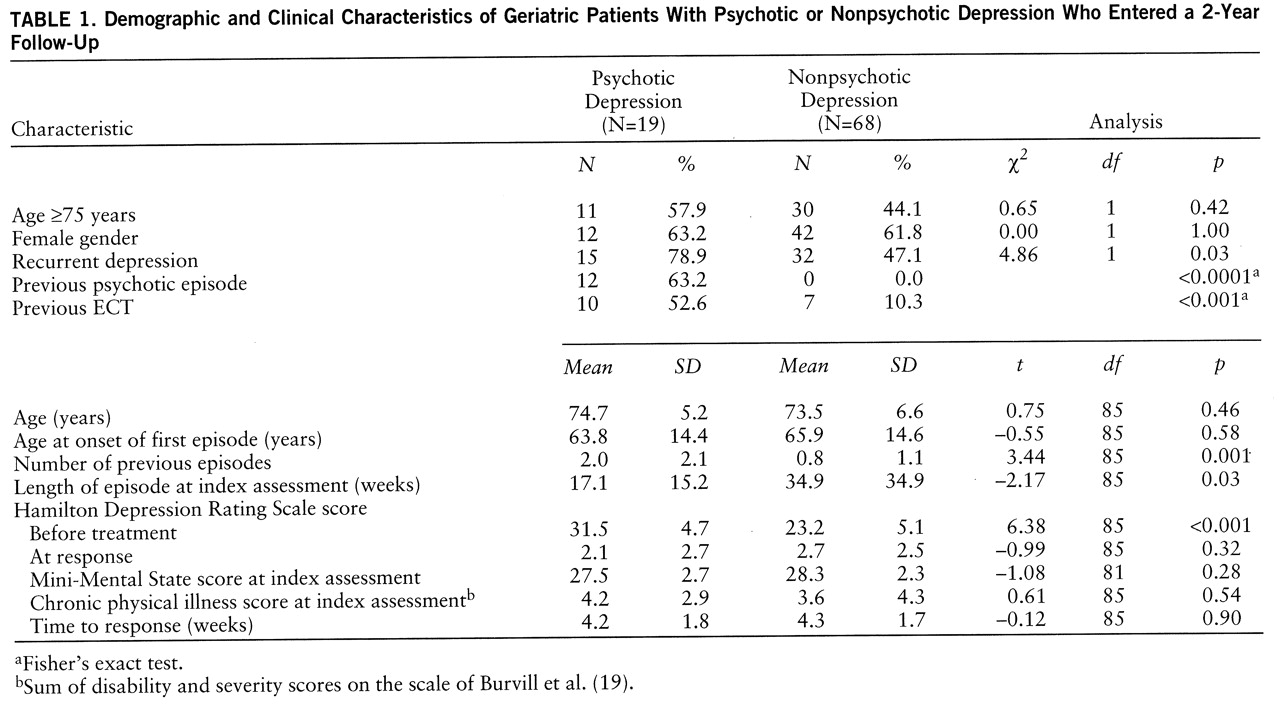
Table 1 describes the demographic and clinical characteristics of the 87 patients who entered the 2-year follow-up phase. Patients with psychotic depression had a higher mean Hamilton depression score at index assessment (p<0.001) and were more likely to have had a past history of depression (p=0.03), more depressive episodes (p=0.001), and previous treatment with ECT (p<0.001, Fisher's exact test). Patients without psychotic features had a longer depressive episode at index assessment (p=0.03). At the time of index assessment all 19 psychotic subjects had delusions, and two (10.5%) of them also had hallucinations.
At the time of starting follow-up, psychotic and nonpsychotic groups, respectively, had mean nortriptyline doses of 69.7 mg/day (SD=21.4) and 70.1 mg/day (SD=20.1). The groups did not significantly differ on mean plasma nortriptyline levels at this stage of treatment (mean=336.1 nmol/liter, SD=116.4, versus mean=325.9, SD=113.5), at 12-month follow-up (mean=321.9, SD=96.7, versus mean=316.4, SD=98.6), at 24-month follow-up (mean=317.2, SD=80.0, versus mean=319.7, SD=106.8), or at the point of relapse or recurrence (mean=341.4, SD=87.5, versus mean=313.5, SD=119.6). The four psychotic subjects who responded to combined medications were taking a mean dose of 20.0 mg/day (SD=8.9) of perphenazine at the start of follow-up.
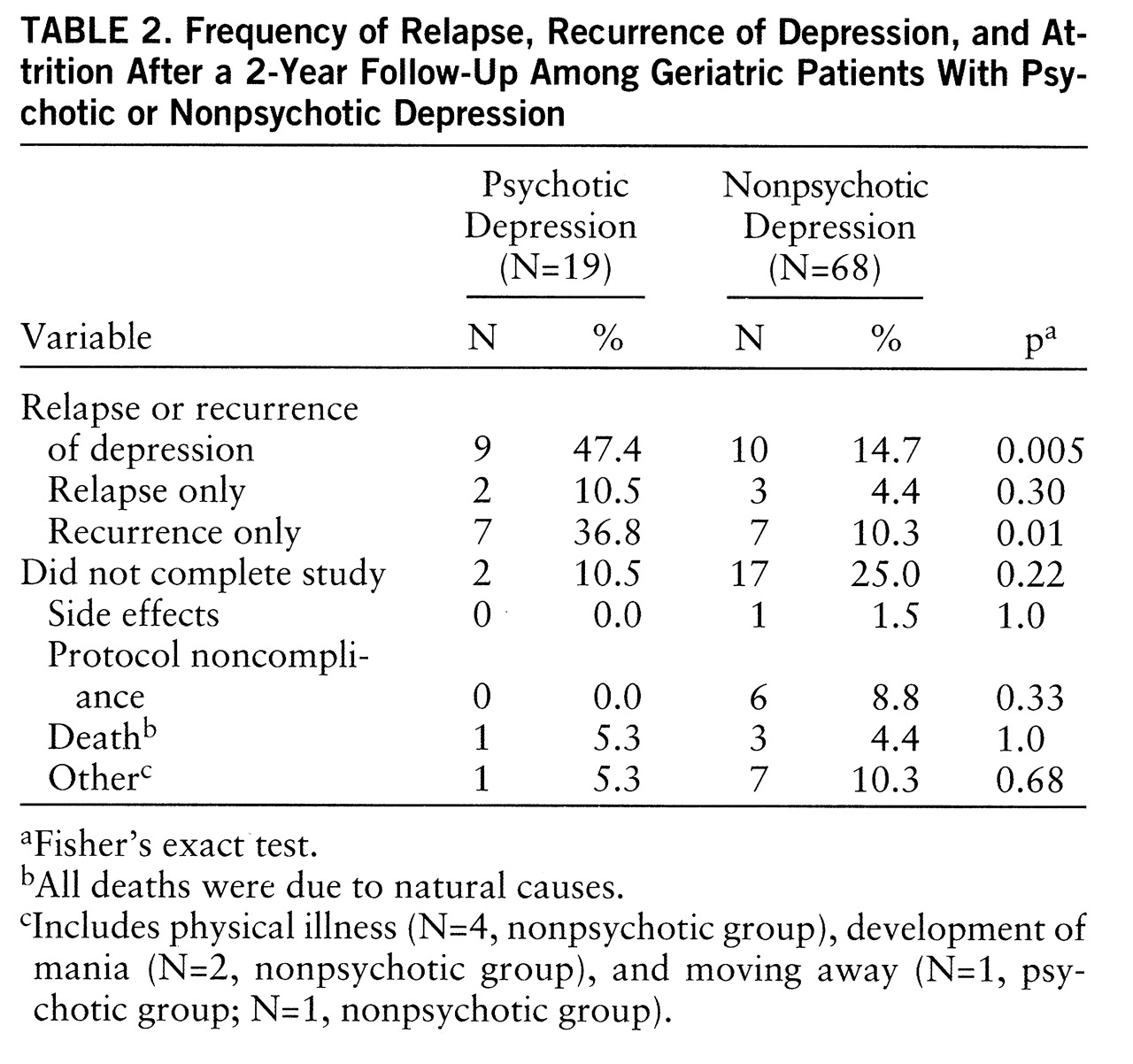
Frequency of Relapse and Recurrence of Depression
Table 2 indicates the number and percent of patients in each group who had a relapse or recurrence of depression (for brevity, these individuals will be collectively referred to as relapsers) or who left the study by the end of 2 years of follow-up. No incident cases of dementia were detected during the follow-up period. The psychotic group was more likely to have had either a relapse or a recurrence (p=0.005, Fisher's exact test; odds ratio=5.2, 95% confidence interval=1.7–16.0) or a recurrence only (p=0.01, Fisher's exact test; odds ratio=5.1, 95% confidence interval=1.5–17.2) than was the nonpsychotic group. Psychotic and nonpsychotic groups did not significantly differ in the proportion of relapsers who were aged 75 years and older (55.6% and 40.0% of relapsers, respectively). Since psychotic and nonpsychotic groups differed on baseline Hamilton depression scores, the number of previous episodes of depression, and duration of the index episode, a stepwise logistic regression analysis was performed across the cohort to assess whether patient group predicted the frequency of relapse or recurrence independent of these variables. Psychosis grouping was the only variable significantly associated with this outcome (χ
2=8.31, df=1, p=0.004).
Within the psychotic group, eight (53.3%) of 15 subjects who responded to ECT became ill (one relapse, seven recurrences), compared to one (25.0%) of the four patients who responded to medication (one relapse during treatment with nortriptyline and perphenazine) (p=0.58, Fisher's exact test). Rates of relapse/recurrence following ECT have been found to be increased in patients who were previously unresponsive to adequate pharmacotherapy (
20). Therefore, we examined whether ECT-relapsers and nonrelapsers differed in the treatments they had received for the index episode before entering the study. None of these individuals had been treated with combined antidepressant-antipsychotic medication or ECT; two (25.0%) of eight relapsers and two (28.6%) of seven nonrelapsers had received 4 weeks or more of a tricyclic antidepressant at 75 mg/day or more.
Survival Analyses
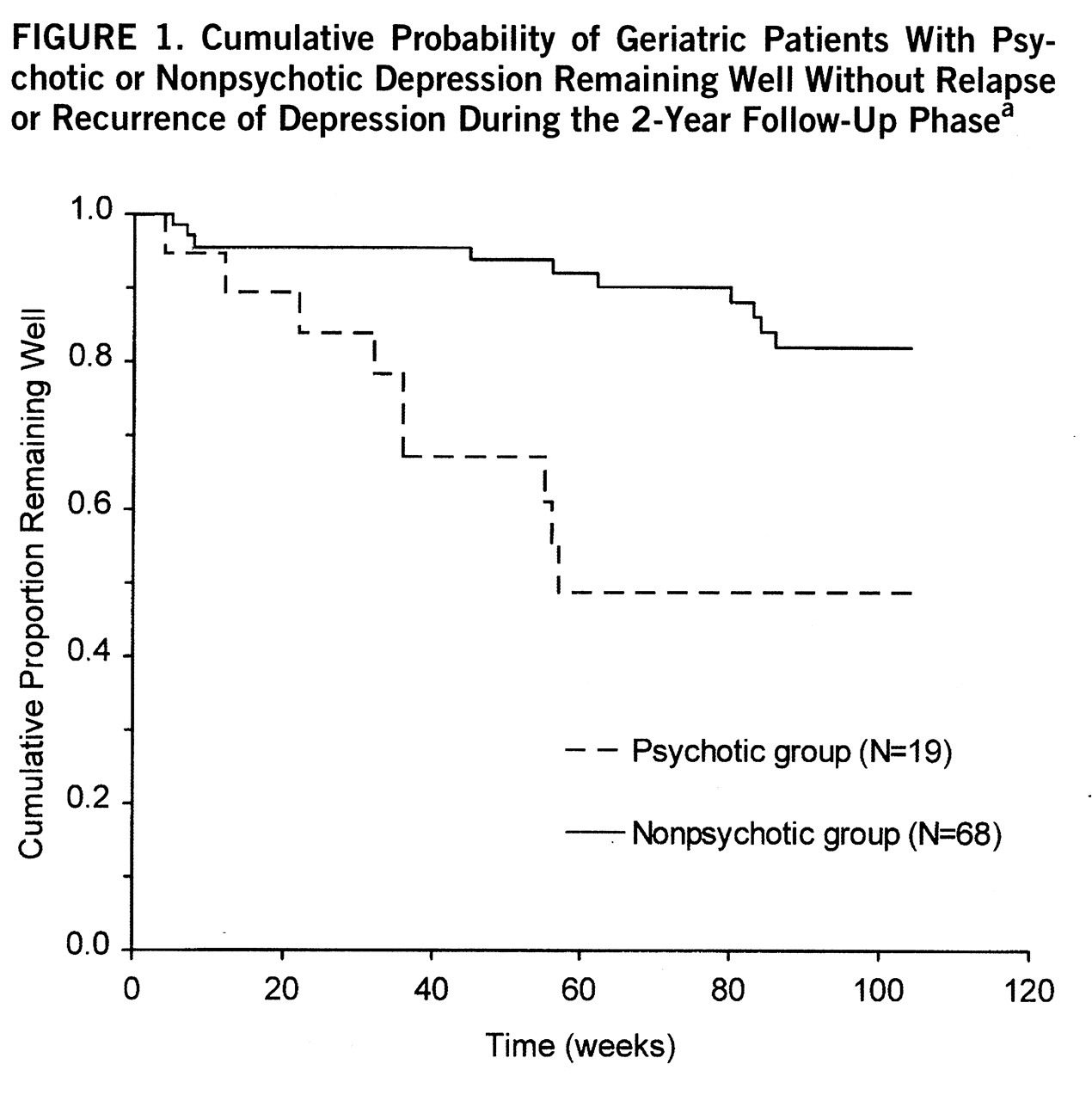
Figure 1 presents the Kaplan-Meier survival curves for psychotic and nonpsychotic groups. The cumulative probability of remaining well without relapse or recurrence was 0.488 for the psychotic group and 0.821 for the nonpsychotic group (p=0.001). The mean survival times for psychotic and nonpsychotic groups were 68.9 weeks (SE=8.7) (95% confidence interval=51.9–85.9) and 95.4 weeks (SE=2.9) (95% confidence interval=89.8–100.9), respectively.
A Cox proportional hazards analysis was performed to examine the effect of covariates on outcome as defined by time to first relapse or recurrence. In addition to psychosis grouping, the following demographic and clinical variables were entered into the model: age, age at onset of the first episode of depression, sex, number of previous episodes, duration of the index episode at the time of assessment, time to respond to treatment of the index episode, Hamilton depression score at index assessment, the sum of severity and disability scores on the chronic physical illness rating scale at index assessment, and life events (as determined by the Bedford Life Events and Difficulties Schedule modified for the elderly [21]) in the 6 months before finishing the study. Following stepwise backward elimination, psychosis grouping was the only variable that was significantly related to outcome (χ2=8.91, df=1, p=0.003).
DISCUSSION
The main finding of this study was that elderly patients with psychotic depression had a higher frequency of relapse/recurrence and a shorter time to these events than depressed patients without psychotic features. This was in spite of the fact that all patients' depression had remitted from the index episode and they were maintained on a regimen of full-dose nortriptyline throughout the period of follow-up. Patients with psychosis were more severely depressed at baseline and had more prior episodes of depression, but these factors did not account for the difference in outcome between the two groups.
Interpretation of this finding is limited by the study design. Patients without psychotic features were maintained on the treatment that they had responded to, whereas most of the patients in the psychotic group were switched from ECT to antidepressant medication at the time of response. Therefore, it is unclear to what extent the results reflect a difference in treatment rather than a difference in the natural history of the disorders. To answer this question, it would have been necessary to restrict the study to patients who had responded to pharmacotherapy. However, consistent with the observations of others (
22), we found that combined antidepressant-antipsychotic medications had limited efficacy in the treatment of psychotic depression in late life. In addition, many elderly patients with psychotic depression are at physical risk (for example, from not eating and drinking) and require ECT on an urgent, first-line basis. These factors would make it difficult to recruit a sufficient number of elderly subjects to a study that was confined to medication responders.
Naturalistic studies of mixed-age patients suggest that psychotic depression does not necessarily have a poor prognosis and that treatment can affect outcome. These studies identified 12-month relapse rates of approximately 50% in patients taking maintenance pharmacotherapy following response to ECT (
23,
24), whereas patients who responded to combined antidepressant-antipsychotic medications and were then maintained on regimens of stable doses of both of these medications had 12-month relapse rates of 20% or less (
25,
26). Most of the patients given ECT in these studies had already failed to respond to adequate pharmacotherapy (and treatment resistance has been found to predict a high rate of relapse after ECT [20]), and so it is unclear to what extent the refractory nature of the depression, rather than a change of treatment at the time of response, accounted for their poor outcome. Similarly, we found that psychotic patients treated with ECT had twice the rate of relapse or recurrence of those who responded to pharmacotherapy, although the validity of this finding is limited by the small group size. However, in contrast to these other studies, none of our ECT-treated patients had been adequately treated for the index episode of depression before entering the study, and, therefore, treatment resistance does not explain the higher rate of relapse or recurrence in this group.
Could the outcome of ECT-treated psychotic patients have been improved with a different approach to continuation or maintenance treatment or both? From a theoretical point of view, continuation/maintenance ECT is an attractive option, since it does not require the cessation of a treatment that patients have responded to. There have been no randomized controlled trials comparing the efficacy of continuation or maintenance ECT with pharmacotherapy in either psychotic or nonpsychotic depression, but many anecdotal reports indicate that patients who have failed to remain well with pharmacotherapy can benefit from ongoing ECT (
27). However, from the point of view of resource availability and consumer acceptance, there are considerable barriers to
routinely continuing with ECT once patients have responded, and it is likely that continuation and maintenance ECT will remain second-line options for patients who do not remain well with medications.
We chose nortriptyline for post-ECT pharmacotherapy so that psychotic and nonpsychotic groups would be matched with respect to long-term treatment. Would a different class of antidepressant medication have offered better prophylaxis? Response rates of 75% or more have been reported for middle-age patients with psychotic depression treated with fluvoxamine alone or sertraline alone (
28,
29). This contrasts with an average rate of 34% for tricyclic monotherapy (
30). Lauritzen and colleagues (
31) recently found that paroxetine was superior to imipramine in preventing relapse following ECT, although that study did not examine whether the medication groups were comparable with respect to pre-ECT treatment resistance. These preliminary findings raise the possibility that psychotic depression may be more responsive to treatment with selective serotonin reuptake inhibitors than with tricyclic antidepressants.
In order to minimize side effects and avoid the risk of tardive dyskinesia, patients who responded to ECT were not prescribed antipsychotic medication as part of their maintenance regimen. However, it has been hypothesized that a combination of antidepressant and antipsychotic medications may improve long-term outcome (
32). There are no controlled data relating to this question, and the data from naturalistic studies are confounded by the treatment resistance issue. For example, 88% of patients relapsing in the study of Spiker et al. (
24) were taking combined maintenance medications, but 81% of these patients had already failed to respond to combined treatment before ECT. If combined treatment was found to be more effective than antidepressant monotherapy, it would be important to determine the optimal duration of antipsychotic treatment. Aronson et al. (
25) and Spiker et al. (
24) observed that in mixed-age patients, most relapses occurred within the first 4 months after the end of ECT. However, the refractory nature of the depression in these samples may have contributed to the preponderance of early relapses. Most of our ECT-treated patients had a recurrence, rather than a relapse, and new episodes of depression were fairly evenly distributed through the first year of treatment. This suggests that in elderly patients who have responded to ECT, antipsychotic medication may need to be continued well beyond the first few months of remission; however, this hypothesis is speculative and needs to be tested.
Given the open nature of this study and the relatively small number of patients with psychotic features, our findings must be considered preliminary. However, they do suggest the need for further research to determine whether alternative treatment strategies can improve the long-term outcome of psychotic depression in older individuals.