Little is known about the course of substance use disorders when they occur with mental illness (
1). In a recent review of the literature on course and outcome of substance use in severely mentally ill adults, Drake et al. (
2) concluded that the rate of remission of substance use disorder for persons with severe mental illness is broadly similar to that for the general population, i.e., only a few patients achieve stable remission. A 7-year naturalistic study of 148 persons with severe mental illness (
1) showed that the prevalence of active substance use disorders changed little from baseline to follow-up and that individuals with baseline diagnoses of abuse rather than dependence were more likely to have achieved remission after 7 years. Treatment studies have yielded inconsistent results, but the authors of a review of 13 studies of treatment for dually diagnosed patients concluded that overall substance abuse was only minimally reduced (
3).
Related to the course of substance abuse in dually diagnosed individuals is the extent to which the adverse consequences of substance use can be reversed with sobriety. Ries et al. (
4) compared current substance abusers, past abusers, and nonabusers among 104 hospitalized patients. They found a continuum of symptoms and resource use; patients with current substance use disorders had the most severe symptoms and used the most treatment resources, patients with past substance use disorders were in the middle, and patients without substance use disorders had the least severe symptoms and least resource use. Kovasznay (
5) compared similar groups of patients and found that the mean number of hospitalizations differed significantly between patients with current substance abuse and nonabusers; patients with past substance abuse fell in between. Other investigators (
6,
7) have found few clinical differences between past substance abusers and nonabusers.
These studies suggest that remission of substance abuse does occur in persons with serious mental illness and that the adverse consequences of substance abuse may attenuate over time. However, these conclusions are speculative in the absence of prospective studies of persons with mental illness and substance use disorders that evaluate diverse outcomes. In this study we took advantage of a database of consecutively admitted psychiatric inpatients with severe mental illness who were systematically evaluated at admission and 1-year follow-up. We compared the nature of substance use patterns and remission in persons with current substance use disorders and those with past substance use disorders. We also compared these groups on clinical and demographic characteristics and assessed the association of substance abuse status (none versus current versus past) with functioning, quality of life, and service utilization at baseline and follow-up.
METHOD
Procedure
All patients admitted to two inner-city psychiatric hospitals, one state operated and the other university operated, were screened between May 1988 and November 1990. These two hospitals are the principal psychiatric facilities serving an urban catchment area of approximately 160,000. The inclusion criteria for all the subjects in the study were as follows: age 18 to 65 years, current residence in the catchment area, ability to speak English, not currently being a ward of the criminal justice system, and competency to give informed consent. All patients were screened within 1 week after admission. After complete description of the study, all subjects provided written informed consent. Information was protected by a Federal Certificate of Confidentiality.
A total of 435 patients admitted to the two psychiatric hospitals during the 30-month recruitment period entered the study. The overall consent rate was 71%. The participants did not differ from the nonparticipants on gender, race, and age; however, the nonparticipants had higher rates of schizophrenia and other psychoses than did the participants. The subjects were contacted again 1 year after their baseline interviews.
Measures
The Structured Clinical Interview for DSM-III-R—Patient Version (SCID-P) (
8) was used to assess current and lifetime DSM-III-R axis I diagnoses. The interrater reliability (kappa) for the SCID-P principal diagnosis was 0.81. The SCID-P also provided information on the percentage of time over the last 5 years for which the patients reported symptoms of substance use disorder. As discussed extensively elsewhere (
9), the SCID-P was modified in this study to distinguish patients thought to have an independent mental disorder not due to substance abuse from those with a mental disorder due to substance abuse. This study included only the individuals with current mental disorders that were definitely
not due to current substance use disorders.
The Addiction Severity Index (
10) is a structured interview assessing the severity of problems related to alcohol and/or drug abuse in seven areas. It also yields detailed information on the course of substance use during the last 30 days. The reliabilities (intraclass correlations) for the Addiction Severity Index composite scores ranged from 0.87 to 0.99.
The Quality of Life Interview (
11) is a 45-minute structured patient interview assessing the quality of life in eight areas: living situation, family relations, social relations, leisure activities, work, finances, safety and legal problems, and health. Interrater reliabilities for the life satisfaction domains ranged from 0.67 to 0.95. The Quality of Life Interview also provided information about the use of specific psychiatric, alcohol, and drug treatment services during the follow-up period.
After the baseline hospitalization, a record review form was used to review each patient's medical records to abstract data on a wide variety of clinical and treatment variables, including the results of urine toxicology screens done at admission.
Data Analysis
Chi-square tests of association were conducted to assess group differences among the patients with current substance use disorders, those with past substance use disorders, and those with no substance use disorders in categorical demographic, clinical, and service use variables. Analysis of variance (ANOVA) was used to assess group differences among the patients with current, past, and no substance use disorders in continuous clinical status variables. Results for overall ANOVAs and all other tests were considered to be significant for p values of less than 0.01. The ANOVAs were followed by Tukey's honestly significant difference adjustment for multiple comparisons. Kruskal-Wallis tests were used to assess differences between the substance-abusing groups in numbers of days, months, and years of substance use before the assessments and in number of previous treatments. A nonparametric test was used because of positively skewed data. All tests were two-tailed.
Attrition
Approximately 66% of the patients were reinterviewed. The proportions of patients lost to follow-up were similar across substance use groups: current, 35% past, 33% none, 34%. Follow-up assessments were completed for 71 patients with current substance use disorder at baseline, 47 patients with past substance use disorder, and 59 patients without substance use disorder. The patients lost to follow-up did not differ from those who completed the second interview in demographic characteristics or in baseline clinical status. The results of the analyses of baseline data did not differ when the patients lost to follow-up were excluded.
RESULTS
Study Group
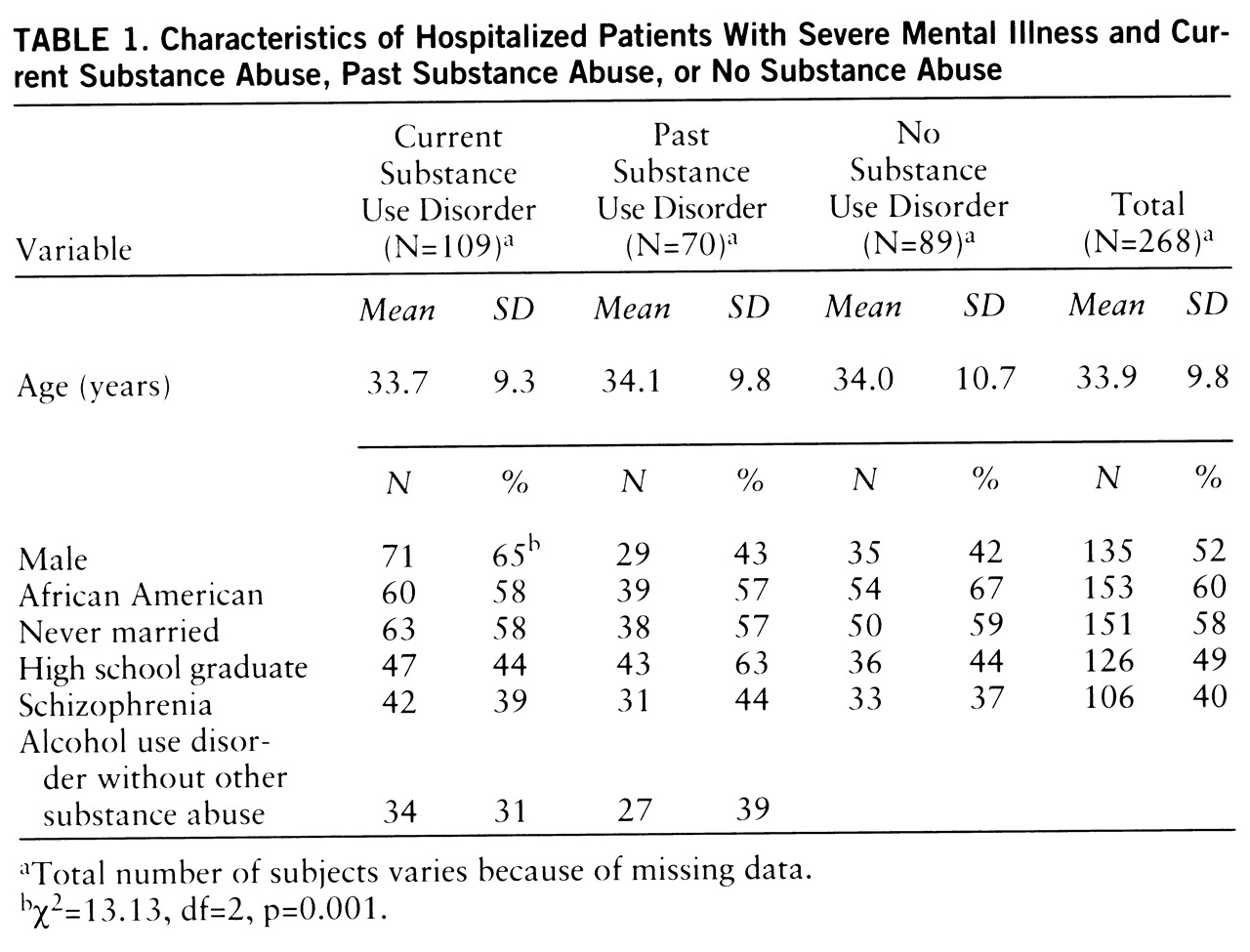
A total of 268 patients with primary DSM-III-R axis I diagnoses other than substance use disorder were classified into three groups. There were 109 individuals diagnosed with current comorbid substance use disorders, 70 individuals with past comorbid substance use disorders, and 89 individuals with no substance use diagnosis. Toxicology screens performed for 46 past abusers showed only two patients (4%) with positive tests, one for marijuana and another for cocaine. The past abusers were more likely to be women (
table 1).
Baseline
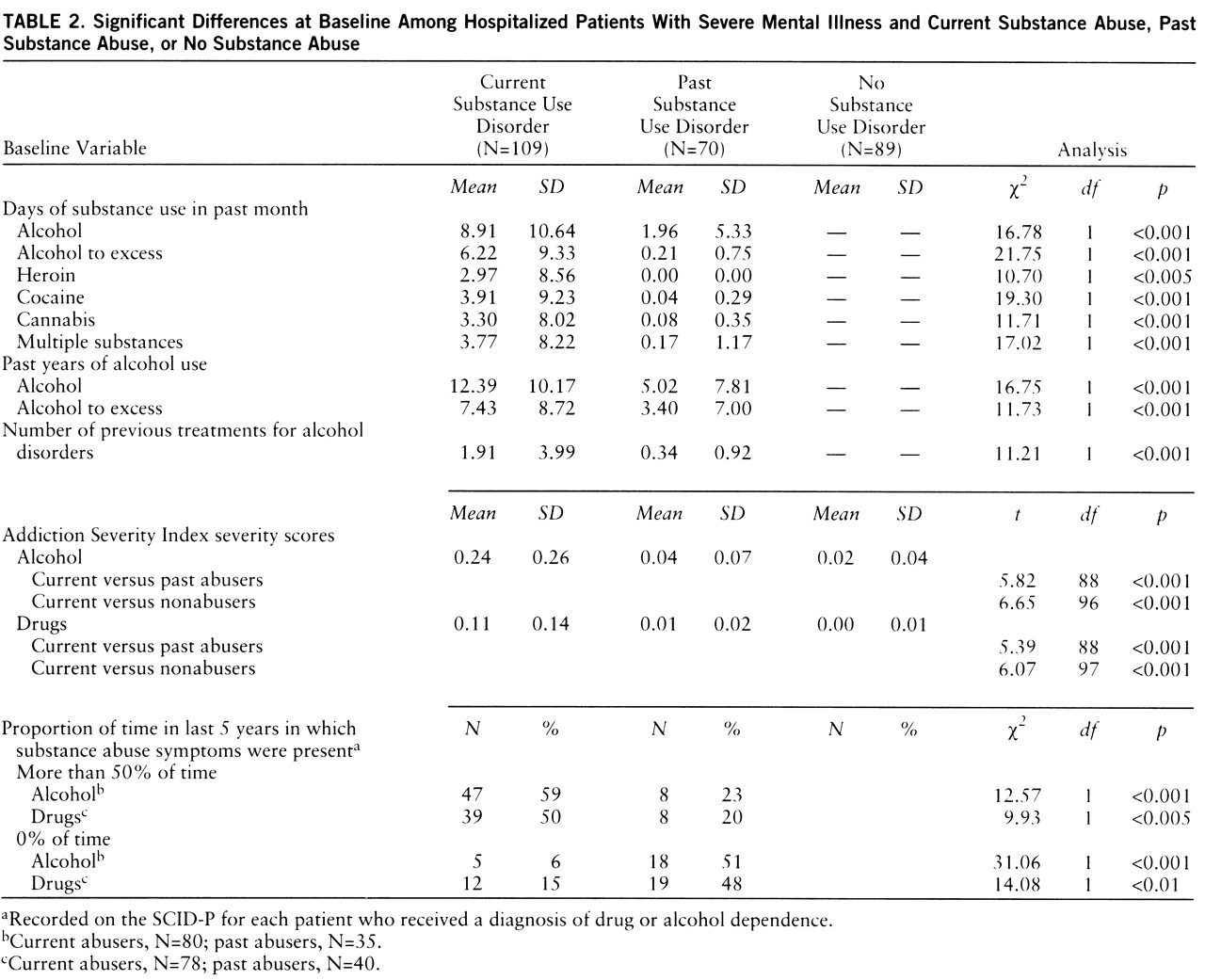
The baseline assessments (
table 2) showed that during the past month the patients with current substance use disorders had used the following substances on more days than had the patients with past substance use disorders: alcohol, alcohol to excess, heroin, cocaine, cannabis, and multiple substances. The patients with current substance abuse had higher scores on the Addiction Severity Index measures of alcohol and drug problems than did the past abusers and nonabusers (
table 2).
The patients with current substance use disorders were significantly
more likely to report having experienced alcohol or drug disorder symptoms more than 50% of the time during the 5 years before the baseline assessment, and they were
less likely to report having had alcohol or drug disorder symptoms 0% of the time (
table 2). The current abusers reported significantly more lifetime total years of alcohol use and of alcohol use to intoxication (
table 2). The current abusers had also received significantly more treatments for alcohol use than had the past abusers (
table 2).
With regard to measures other than those directly involving substance abuse, the patients with past substance use disorders had greater severity of family problems, as shown by the Addiction Severity Index, than did the nonabusers (past abusers: mean score=0.33, SD=0.25; nonabusers: mean=0.16, SD=0.21) (t=3.39, df=89, p<0.01). The current substance abusers had significantly greater severity of legal problems, as shown by scores on the Addiction Severity Index (mean=0.11, SD=0.20), than did the past abusers (mean=0.02, SD=0.06) or the nonabusers (mean=0.02, SD=0.07) (current versus past: t=3.42, df=106, p<0.005; current versus none: t=3.61, df=116, p<0.005).
Follow-Up
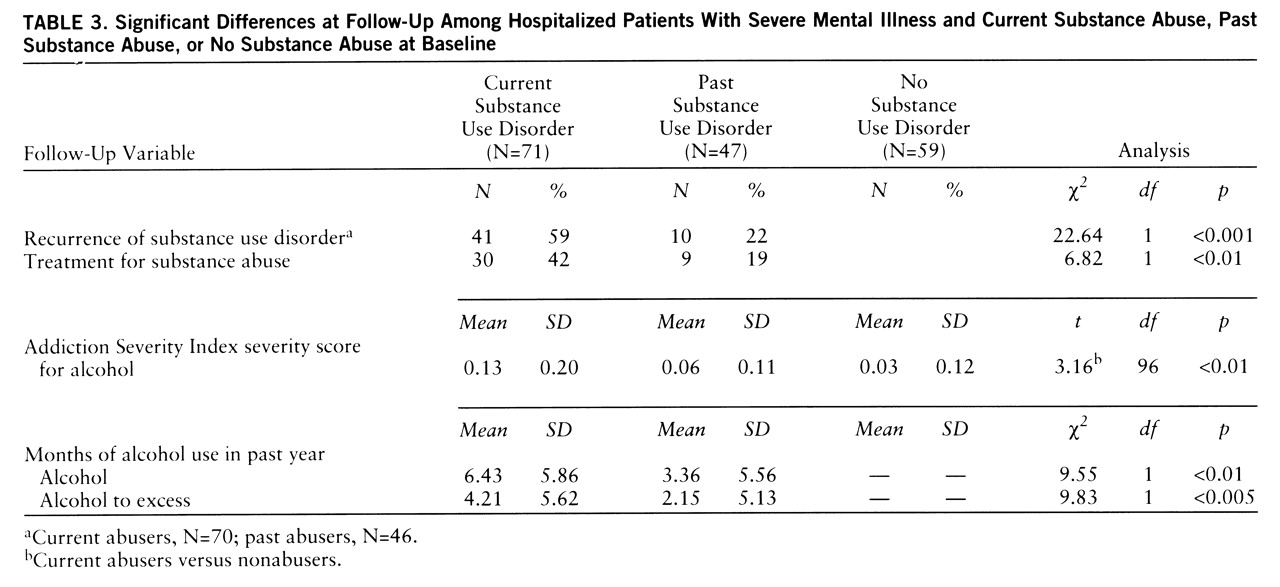
During the follow-up period the patients with current substance abuse at baseline were significantly more likely to experience a recurrence of substance use disorder, were more likely to use a substance abuse service, and had more months of alcohol use and alcohol use to excess than past substance abusers (
table 3). There were no significant differences in the use of psychiatric services. The current abusers also had significantly greater severity of alcohol problems than the nonabusers at follow-up (
table 3). When baseline status was controlled for, no differences emerged in the drug and alcohol composite scores from the Addiction Severity Index. No significant differences among the groups were found at follow-up in measures other than substance abuse.
DISCUSSION
This naturalistic study suggests that a substantial proportion of patients with severe mental illness and past substance use disorders have stable remissions of their substance use disorders. Evidence from patient self-report, toxicology screens, and clinical records at baseline and from 1-year follow-up patient interviews suggests that as many as 75% of patients whose self-reports are consistent with past diagnoses of substance use disorders may in fact be experiencing stable remission or recovery. If it is assumed that all of the patients who were lost to follow-up had suffered recurrences of their substance use disorders, a more conservative estimate of stable recovery from this study would be 50%, still impressive given the unfortunate vulnerability of these individuals to substance abuse. The lower rate of substance abuse during follow-up reported by persons in remission at baseline was accompanied by a lower rate of use of treatment services for substance abuse.
Men were more likely to be classified as current users than women. It is possible that women are more likely to achieve recovery than men. It is also possible that this observation is an artifact of the study setting; men with current substance use disorders may be more likely to develop substance-induced behavioral problems resulting in hospitalization. This finding may also be related to the possibility that women with substance use disorders are underrepresented in substance abuse treatment (
12).
The lack of differences in non-substance-abuse outcomes observed between nonabusers and both current and past abusers is surprising. It might be due to the fact that the inpatient sampling procedure resulted in selection of patients with a restricted range of functioning and high levels of symptoms and acute problems, obscuring any differences due to substance abuse. Also, the subjects in the study group tended to suffer from poverty and a host of other social problems, factors that may diminish the marginal effects of substance abuse on overall outcome.
This study has several important limitations. First, the study group was representative of an urban catchment area and may not resemble other groups of dually diagnosed patients in substance disorder symptoms or course. The patients reinterviewed at 1-year follow-up may not be representative of dually diagnosed patients, who are difficult to engage in assessment and treatment (
2). Finally, although collected by way of structured clinical interviews and review of medical charts, the data were largely gathered through self-report and were susceptible to selective responses by the patients. In spite of these limitations, we think these findings provide reason for some optimism regarding remission of substance abuse among persons with mental illness, even those who experience major problems with their mental illness leading to inpatient hospitalization.