Depression is a common mental disorder in the general population. The most recent estimate from the National Comorbidity Survey
(1) indicates that the 1-year prevalence of unipolar major depression and dysthymia among community residents 15 to 54 years old is 10.3%, or about 27 million Americans today. In addition, it is estimated that 11.0% of community residents who do not meet the strict criteria for either unipolar major depression or dysthymia have substantial depressive symptoms
(2). Estimates of treatment costs for depressive disorders range between $12.4 billion
(3) and $19.2 billion
(4) per year in 1990 dollars.
Treatment costs, however, are only a small portion of the total cost of depression to society; the consensus reached by a national panel is that depression is seriously undertreated, resulting in large economic costs to society
(5). Conservative estimates of costs due to mortality and morbidity (disability and lost productivity)
(6–
11) range from $11.2 billion
(4) to $31.3 billion
(3) in 1990 dollars, not to mention costs to family caregivers
(12,
13), lost leisure time
(14), and the pain and suffering endured by depressed individuals and their families
(15).
The Agency for Health Care Policy and Research
(2,
16) developed guidelines that synthesize recommendations for treatment of major depression from an extensive efficacy literature. Researchers concluded that 50%–60% of patients report marked improvement in symptoms in response to pharmacotherapy or psychotherapy
(17–
19). A 1995 study
(20) demonstrated that, compared with treatment in the general medical sector, treatment for depression in the mental health specialty sector improves functional outcomes while increasing the total costs of care. The authors concluded that depression treatment currently provided by the general medical sector is not cost-effective because of its poorer outcomes, even though treatment costs are lower. However, efforts to contain rising health care costs make providing a greater proportion of mental health services in the general medical sector very attractive, particularly in a managed care environment.
Because effective treatment for depression improves function
(21), it may also reduce the associated costs of morbidity. In reviewing 10 published treatment studies of depression, Mintz et al.
(11) concluded that “generally, work outcomes were good when treatment was systematically effective.” Broadhead et al.
(6) also demonstrated that the severity of depression is significantly related to lost workdays. In the current study, we examined the relationship between changes in earnings associated with lost workdays and costs of depression treatment in the mental health sector compared with treatment in the general medical sector in a community-based sample of depressed individuals seeking routine care. Lost workdays produce conservative estimates of lost productivity because this measure does not include reduced productivity while at work.
Although our analyses were performed from a societal perspective, the results have obvious implications for both employers and employees. If employers bear the costs of lost workdays, any net savings of employment earnings in the mental health sector imply that employers should encourage their employees to seek treatment for depression in the mental health sector even if it means that the employers pay more for treatment costs. If workers themselves bear the costs of lost workdays (because they are self-employed or do not have paid sick leave), net savings imply that they should seek treatment for depression in the mental health sector even when they have to pay more for the total treatment costs.
METHOD
Data Collection
A detailed description of the data collection procedure was presented in an earlier publication
(22). Briefly, using a stratified sample design to oversample rural subjects, 11,078 individuals from 15,721 randomly selected households in Arkansas with listed or unlisted telephone numbers completed a validated eight-item screening instrument
(23) for current depression. Nine hundred ninety-eight of these individuals (9.0%) screened positive for depressive disorder or substantial depressive symptoms. Subjects who screened positive were excluded from the study if 1) they exhibited acute suicidal ideation (N=14); 2) they reported that their depressed mood began following the loss of a loved one (N=288); 3) the subject was subsequently diagnosed as having lifetime mania (N=54); or 4) the subject denied all depressive symptoms in the extended baseline interview (N=8). Of the remaining 634 eligible individuals, 470 (74.1%) agreed to participate in the longitudinal study. After the study was completely described to each of the subjects, their written informed consent was obtained.
The data were collected in three stages: an extended baseline interview and 6-month and 12-month follow-up interviews. The extended baseline interviews were conducted in the subjects’ homes and the follow-up interviews over the telephone. During the baseline interview, the depression section of the National Institute of Mental Health Diagnostic Interview Schedule
(24) was used to diagnose lifetime and current major depression and dysthymia. Subjects who did not meet criteria for a depressive disorder but who were categorized as having substantial symptoms of depression constituted a group with levels of functional impairment comparable to those of the group meeting criteria
(25).
To collect information on utilization or charges, subjects were asked to provide consent for release of information from all providers (hospitals, physicians, psychologists, social workers, counselors, nurse practitioners, physician assistants, chiropractors, hospitals, emergency rooms, clinics, and pharmacies) and third-party payers of health care costs during the previous 6 months at the 6- and 12-month interviews. Both health care providers and third-party payers were contacted to obtain all essential medical records and billing/reimbursement records. These records were also used to identify additional health care providers seen but not initially identified by the subject. Medical and billing records from these additional providers were then obtained. This process, although labor-intensive, has been used in several successful projects
(26,
27) to collect utilization and expenditure data in a community population.
The follow-up rate was 97.8% (N=455) at 6 months (excluding five subjects who died before the 6-month follow-up) and 98.5% (N=456) at 12 months (excluding two subjects who died between the 6- and 12-month interviews). We obtained complete insurance and medical records for 435 subjects, 171 of whom received treatment for depression during the 12-month period of the study. These are the subjects we are concentrating on for purpose of the analysis described in this paper.
Definition of Dependent Variables
Costs of (savings in) lost earnings
Treatment for depression, if effective, is expected to produce benefits to patients and society, including an improvement in functioning that results in a reduction in lost workdays
(11). Although there are other categories of economic benefits resulting from treatment, we limited our analyses to the changes in lost earnings. The central question from society’s perspective is whether the savings in lost earnings for subjects with depression that result from treatment in the mental health sector are sufficiently large to compensate for the increased cost of treatment in this sector compared with the general medical sector.
Costs of treatment for depression
Charges were used as a proxy for treatment costs. From society’s perspective, the total costs of depression treatment should include all resources used by the provider in providing services and all costs incurred by the patient in obtaining the services. They should include the costs of provider services, as well as costs of patient time (travel time, waiting time, and treatment time) and transportation. In our base-case scenario, we included only provider costs (charges) as costs of treatment because we did not have data on patient time and transportation costs. However, we subsequently performed a sensitivity analysis by including estimated patient time costs.
We recognize that cost-shifting produces a discrepancy between costs and charges for a given service
(28). For example, providers usually bill Medicaid for what its fixed schedule reimburses, since providers participating in Medicaid agree to accept the fixed reimbursement as payment in full. Medicaid reimbursements are usually low; therefore, charges (usually equal to the reimbursements) are likely to bias the costs of service downward. On the other hand, providers usually bill private insurers at a higher level; such charges are likely to bias the costs of services upward. We elected to approximate costs by using charges in our community sample, where subjects were covered by different types of insurance—Medicaid, Medicare, private insurance, or no insurance. We assumed that the downward bias from using charges as a proxy for costs in one group of subjects (e.g., Medicaid) would be partially offset by the upward bias in another group of subjects (e.g., private insurance).
Determination of Costs
Costs of lost earnings
Subjects were asked about the number of workdays lost for the 4 weeks before baseline, 6-month, and 12-month follow-up interviews; interim estimates were linearly extrapolated. Accumulated changes in lost workdays during the first and second 6-month periods were summed to derive the annual change in lost workdays. A negative value indicates that the total number of lost workdays decreased during the 12 months after baseline. If a subject changed employment status from employed to unemployed (or vice versa) between two interviews, we assumed that all the days were lost workdays in the 4-week period before the interview during which the subject was unemployed. For example, if a subject was employed at baseline but unemployed at 6-month follow-up, then the lost workdays for the 4 weeks prior to the 6-month follow-up were assumed to be 20 (5 days a week for 4 weeks). To calculate the changes in lost earnings due to changes in lost workdays, the number of lost workdays was multiplied by 8 (hours) and then by the subject’s hourly wage rate. For subjects with missing wage rates, the mean wage rate for the subject’s age, sex, and occupation from the Statistical Abstract of the United States
(29) was used. Since the mean earnings in Arkansas were 77.3% of the national average in 1993 ($19,008 versus $24,575 annually)
(29), we weighted the national wage rates by 77.3% for our subjects.
Costs of treatment for depression
To calculate the costs of depression treatment as accurately as possible, a reliable methodology was developed to abstract charge data from medical and billing/reimbursement records. These records include records from providers (hospitals, physicians, etc.), insurance companies, and pharmacists. One of us (M.Z.) conducted a 1-week training session for abstractors using a detailed protocol he developed for abstracting utilization/charge data from these records. During the training session, the abstractors and M.Z. compared the results of abstracting they completed independently on 10 selected subjects, analyzed reasons for discrepant coding decisions, established new rules as needed, and incorporated all rules into the final written protocol. Two research assistants abstracted the provider, insurance/reimbursement, and pharmacy records according to this final protocol. The research assistants achieved and maintained a high degree of interrater reliability (>0.90).
When medical and insurance records indicated depression as the sole diagnosis, all charges associated with the hospitalization or visit were attributed to depression treatment except for procedures unrelated to depression (e.g., chest X-rays, Pap smears, allergy injections). When depression treatment was provided during hospitalizations wherein patients primarily received care for physical problems, two psychiatrists independently reviewed the medical and billing records to allocate the proportion of charges relevant to depression. When the two psychiatrists disagreed about the amount of charges attributable to the treatment of depression, we deferred to the higher estimate. When depression treatment was provided during outpatient visits during which the patient received care for physical problems, we allocated 50% of the charges for the visit (excluding procedures) to depression treatment in our base-case scenario. The remaining charges (including procedures) were allocated to care for physical problems. A similar procedure was used to allocate charges when the visit addressed multiple psychiatric problems that included depression.
We performed sensitivity analyses in alternative scenarios by varying the percentage allocation. For pharmacy costs, we designated all costs of antidepressant medications as costs for depression treatment. The overall costs of depression treatment were the sum of costs of inpatient depression treatment, outpatient depression treatment, and antidepressant medications. All health care costs were converted into 1994 fourth-quarter values by using the medical component of the consumer price index
(29).
Definitions of Other Major Variables
Treatment sector was measured by a dummy variable indicating whether a subject received depression treatment from mental health specialists. This variable was equal to 1 if a subject received depression treatment from any mental health specialist and equal to 0 if the subject received depression treatment only from general medical providers.
Physical comorbidity was measured by the number of chronic physical conditions reported by a subject at baseline. The 11 possible conditions were arthritis, asthma, cancer, diabetes, epilepsy, heart disease, chronic lung disease, gastrointestinal disorders, hypertension, renal failure, and stroke.
Comorbid psychiatric diagnoses, identified at baseline by the Quick Diagnostic Interview Schedule
(30), included lifetime and 1-year anxiety disorder, panic disorder, obsessive-compulsive disorder, alcohol dependence or abuse, drug dependence or abuse, schizophrenia or schizophreniform disorder, and posttraumatic stress disorder.
Severity of depression was measured by the acuity of DSM-III-R depressive symptoms, standardized to a scale of 0–100.
Sociodemographic variables included age, sex, education level, marital status, and minority status. Income was expressed as the ratio of family income to poverty line according to family size.
Analytical Model
We estimated the expected changes in lost earnings and, separately, the expected costs of depression treatment for subjects receiving treatment in the mental health sector compared with the general medical sector, controlling for sociodemographic variables, baseline physical and psychiatric comorbid disorders, and baseline severity of depression. To increase the representativeness of our subjects of the depressed adults we identified in the telephone survey and to adjust for the stratified sampling design, we weighted the sample by age, sex, education, and regional distribution.
We estimated changes in lost earnings by using ordinary least squares. The dependent variable was the changes in lost earnings. The dummy variable indicating sector of depression treatment was included as a regressor. The estimated coefficient on this dummy variable indicated the effect on the changes in lost earnings. In addition, a group of covariates were used as control variables in the regression. They included sociodemographic variables (age, sex, education, marital status, and race), baseline physical and psychiatric comorbid disorders, and baseline severity of depression. Using this same model, we also estimated the costs of depression treatment for subjects receiving treatment for depression in the mental health sector compared with those receiving treatment in the general medical sector. In this estimation, cost of depression treatment was the dependent variable.
After we obtained the estimated coefficients from the two regressions, we subtracted the expected costs of depression treatment from the expected changes in lost earnings to derive the difference, the net economic savings between receiving treatment in one sector as opposed to another sector.
RESULTS
Among the 171 subjects, 56 (33%) received depression treatment in the mental health sector; the remaining 115 received depression treatment in the general medical sector. Of the 56 subjects receiving treatment in the mental health sector, 41 (73%) also received depression treatment in the general medical sector.
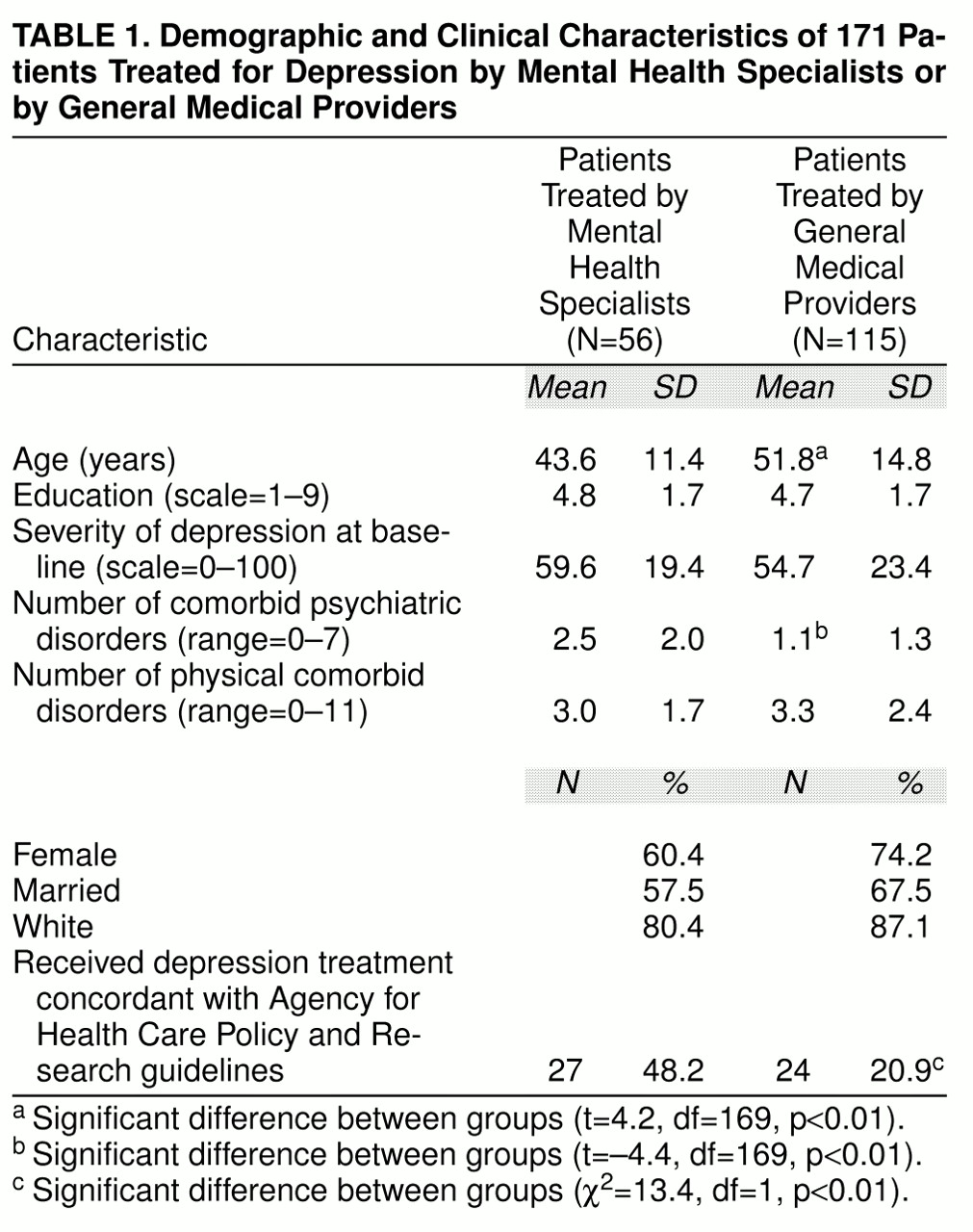
table 1 presents the characteristics of the subjects who received care in the two sectors in bivariate analyses. Patients receiving treatment from mental health specialists were younger and had more comorbid psychiatric disorders. There were no significant differences in other control variables between these two groups of patients. However, almost half of the subjects who were treated in the mental health sector received depression treatment concordant with the guidelines developed by the Agency for Health Care Policy and Research, compared with only 21% of the subjects treated in the general medical sector. The ratio of family income to poverty line according to family size was 2.6 for the subjects treated by mental health specialists and 2.9 for those treated by general medical providers.
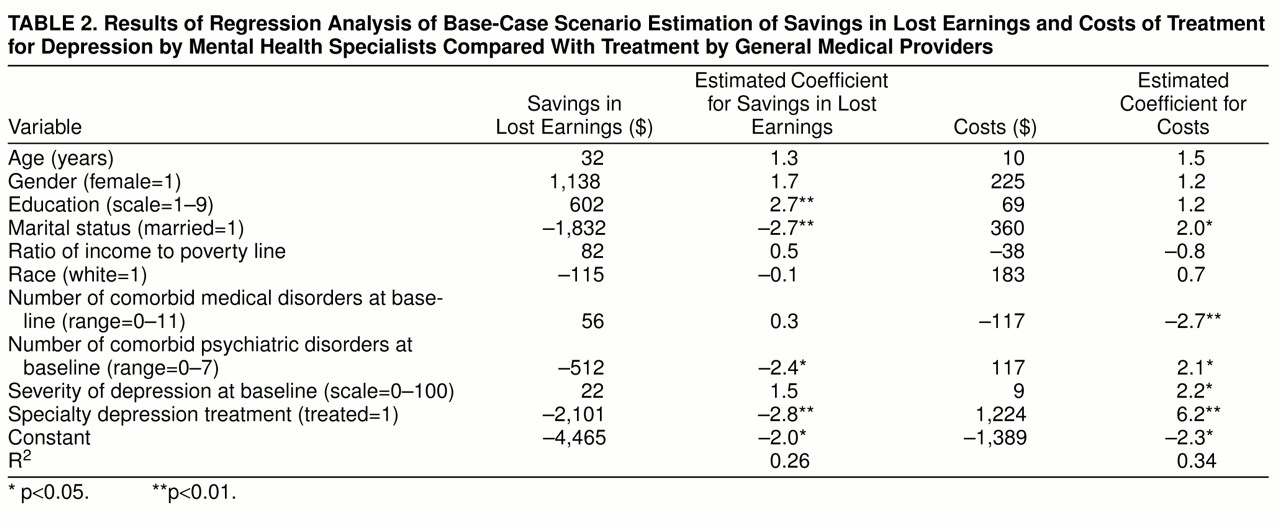
The regression results of estimating earnings and costs in the base-case scenario are presented in
table 2. The estimated coefficient of the earnings equation indicated that the lost earnings for the average patient receiving depression treatment in the mental health sector was $2,101 lower than that of the average patient receiving depression treatment in the general medical sector during the 12-month period. In the cost equation, the expected costs of treatment for the average patient receiving depression treatment in the mental health sector were $1,224 higher than that in the general medical sector. In other words, depression treatment in the mental health sector had an average annual net savings of $877 ($2,101–$1,224) over depression treatment in the general medical sector.
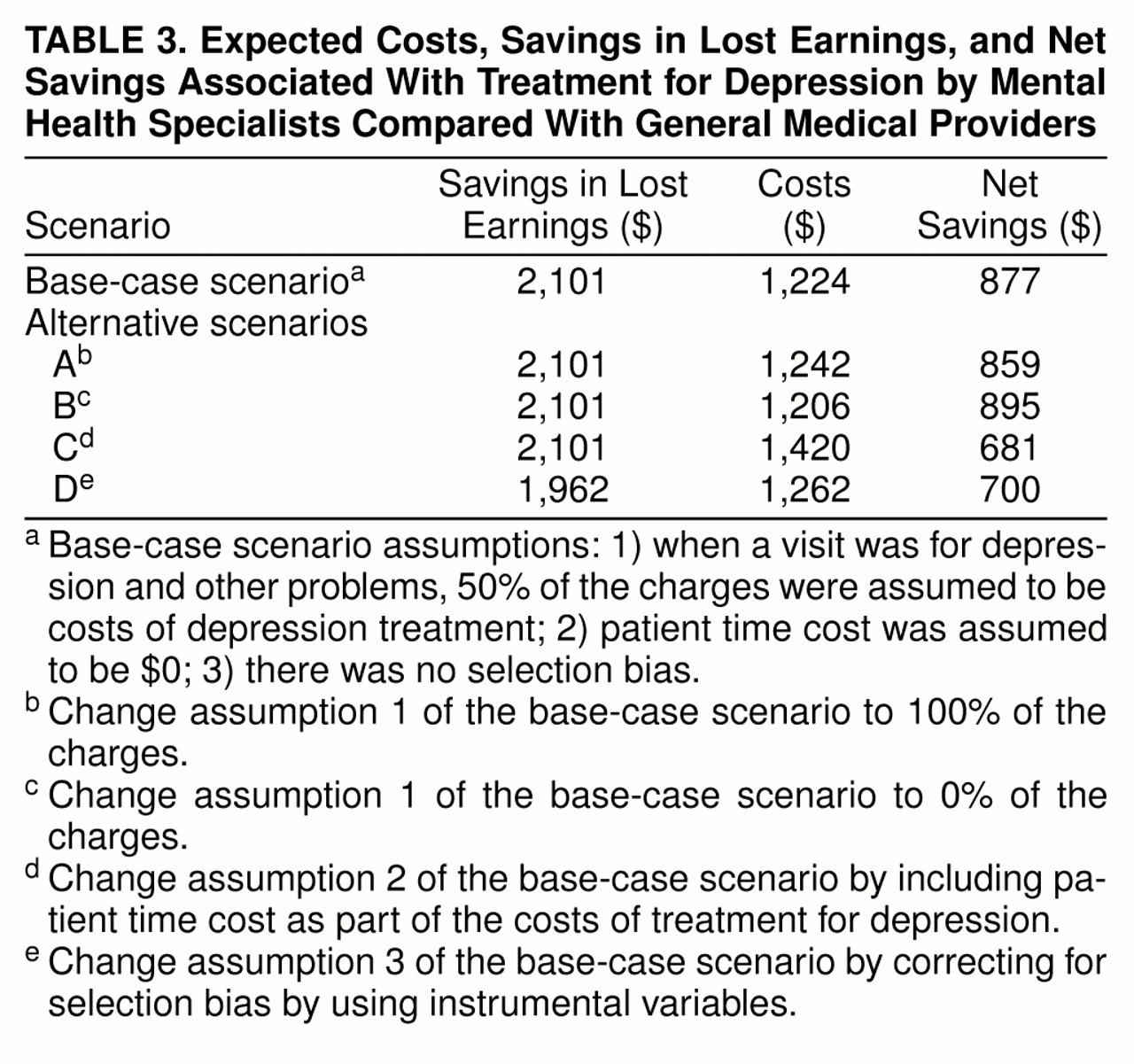
Realizing that our results on savings from depression treatment in the mental health sector were based on several assumptions that are difficult to validate, we performed sensitivity analyses in several alternative scenarios to examine the robustness of these results. The results in these alternative scenarios, along with that of the base-case scenario, are presented in
table 3.
In the base-case scenario, we allocated 50% of the charges for a visit as costs of treatment for depression when the visit was mainly for physical or other problems. This allocation was arbitrary; therefore, we performed an analysis by allocating 100% of the charges as costs of treatment for depression for those visits. The average annual net savings in this scenario (scenario A) was $859. We also performed an analysis using 0% as the allocation of depression treatment costs (scenario B), and the net savings for depression treatment provided by specialists was $895.
From the societal perspective as well as the patient’s perspective, the time spent by the patient in obtaining treatment (including travel time, waiting time, and time seeing the provider) should be considered as part of the costs of treatment. We performed an analysis including an estimated patient time cost in the treatment costs (scenario C). Specifically, for outpatient visits that were exclusively for depression we assumed the total time spent by the patient was 3 hours for each visit. We assumed, for these 3 hours, 1 hour for traveling to the physician’s office, 1 hour for traveling back home, and 1 hour for waiting and seeing the physician. For outpatient visits that were partially for depression, we assumed that 1.5 hours (half of the total 3 hours) of the patient’s time could be attributed to depression cost. For inpatient admissions, we assumed 8 hours/day during the hospital stay. Then the total number of hours was prorated by the ratio of depression charges to the total charges of the stay when the admission was only partially for depression. We then added this time cost to depression treatment costs already calculated in the base-case scenario and performed the cost regression. In this scenario, the average annual net savings for depression treatment in the mental health sector, compared with the general medical sector, was $681.
The decision to seek treatment for depression in the mental health sector may be affected by such observed characteristics as severity of depression and comorbidity, but it may also be affected by unobserved characteristics. It is possible that patients seeking depression treatment in the mental health sector are more motivated to improve; hence, the estimated treatment effect may be biased. In a controlled trial, differences in subject characteristics (observed or unobserved) between the treatment and control groups, and hence any bias produced thereby, are balanced by random assignment
(31). We used subject travel distances to providers as instrumental variables in a two-stage estimation to correct for the potential selection bias
(32). Detailed procedures applying the instrumental variables in this analysis are available on request. The results in this scenario (scenario D) indicated a $700 annual net savings for depression treatment in the mental health sector over treatment in the general medical sector.
DISCUSSION
Although much of the research to date has focused on ways to reduce the direct costs of treatment for psychiatric disorders and/or for physical problems exacerbated by psychiatric disorders (known as cost offset)
(26,
33,
34), the wisdom of focusing exclusively on treatment costs in evaluating the overall economic effects of depression treatment is questionable. In fact, we performed a regression analysis (not shown) examining this issue. We did not find a statistically significant difference in physical health care costs between subjects in our two treatment sectors after controlling for sociodemographic variables, baseline severity, and baseline physical and psychiatric comorbid disorders.
If reducing treatment costs is the sole objective when choosing one type of depression treatment over another, the obvious approach is to shift virtually all depression treatment from mental health specialists to generalists because the costs of treatment would be lower. However, only $1 out of every $4 of the total cost of depression is treatment cost
(3); other costs, including lost workdays, constitute $31.3 billion of the $43.7 billion that represents the total cost of depression
(3). In determining the economic value of depression treatment, it is necessary to include the changes in potential savings in morbidity costs, such as lost earnings, and other treatment outcomes.
Our analyses indicate that depression treatment provided by specialists, although more expensive, more than pays for itself in terms of savings in lost earnings compared with treatment provided by generalists. Depression treatment provided by specialists was associated with a net annual savings of $877 in earnings in the base-case scenario. Our sensitivity analyses in the alternative scenarios indicate similar net economic savings. Our conclusions are conservative because we have not included the increased productivity from improved performance during days the depressed individual is at work, the cost of which is estimated to be greater than productivity loss from lost workdays
(3). We also have not included the increased productivity at home in our analyses.
We speculate that the net economic savings associated with depression treatment by specialists is probably due to their more extensive training and expertise in treating mental health problems. As shown in
table 1, among the 56 patients treated by mental health specialists, 27 (48%) received depression treatment concordant with the Agency for Health Care Policy and Research guidelines
(2,
16), compared with 24 (21%) of the 115 patients treated by general medical providers. This difference is statistically significant (
table 1). Although it costs less, routine treatment by generalists may not be effective enough to have an impact on patients’ functional capacity. This point is echoed by Sturm and Wells
(20), who concluded that, as it is currently practiced, depression treatment in the general medical sector is not cost-effective in reducing functional disability and, therefore, does not produce value to society, although the costs are low. If high-quality treatment for depression, such as that concordant with the Agency for Health Care Policy and Research guidelines, results in a greater improvement in patient outcomes, we expect greater economic savings as a result of further reductions in lost workdays and further gains in productivity. Future studies should be designed to examine the relationship between quality of treatment and these economic benefits.
Although our conclusions are strengthened by the study’s prospective design, high follow-up rates, and the extensive procedure we used to reconcile self-report and medical/insurance records to determine utilization, we also acknowledge several limitations.
First, because we recruited our subjects using a telephone survey, we eliminated the approximately 11% of the state’s residents who were without a household telephone. We were also less successful recruiting rural participants, which may introduce a bias that is difficult to estimate even with corrective weighting.
Second, because few subjects were covered by capitated insurance plans, we do not know whether these findings generalize to regions where capitation dominates.
Third, we included only savings in lost workdays as economic benefits; other important benefits such as savings in lost household productivity were not included in our analyses.
Fourth, the data on lost workdays were based on subjects’ self-report. We chose these self-report questions to enhance our ability to compare our study’s findings about lost workdays with the large economic and epidemiologic surveys in the field, such as the Medical Outcomes Study
(25) and the Epidemiologic Catchment Area study
(6). To our knowledge, no study has demonstrated the relationship between self-reported and actual lost workdays. Without actual data about lost workdays, we cannot ascertain whether self-report is state-dependent; one would expect that the magnitude of error in reporting lost workdays may be related to severity of depression. However, all of the patients in our sample were depressed and, as shown in
table 1, patients seeking depression treatment in the two sectors were not different in most of the variables, including depression severity. Therefore, it is not unreasonable to expect that the reporting errors are comparable between subjects seeking depression treatment in the two sectors.
Fifth, we are not certain if all the lost workdays were related to depression; other factors such as downsizing and seasonal employment may affect the number of lost workdays. Again, our purpose was to compare the lost workdays between subjects in the two sectors. If these other factors have the same effect on lost workdays for both groups of subjects, our conclusions should still hold.
Even with these limitations, the results from this study point to potential economic savings associated with depression treatment obtained from mental health specialists in routine care settings. To increase economic efficiency as well as to reduce the suffering of individuals with mental health problems such as depression, policies should be designed to encourage affected individuals to seek effective professional help. Clearly, the publicly funded initiatives to educate general medical physicians in providing effective depression treatment should return extensive economic benefits to patients, their families, their employers, and society as a whole
(2,
16,
35).