Disaster workers are at risk of both acute and chronic posttraumatic stress disorder (PTSD)
(1). Perhaps the most difficult aspect of disaster work is exposure to violent death and dead bodies
(2,
3) . Several early studies
(4,
5) documented the highly stressful nature of working with the dead following a disaster. Two empirical investigations of emergency services personnel responding to the 1989 Loma Prieta earthquake
(6,
7) suggested that approximately 9% of the workers showed psychiatric symptoms at the level of those of an outpatient population. A study of body handlers
(8) found that 11% had PTSD 3 months after their disaster work. Troops deployed in Operation Desert Storm who performed graves registration duties had increased posttraumatic stress symptoms
(9–
11) ; nearly one-half had current PTSD
(11). Even professionals working with the dead have increased rates of posttraumatic stress symptoms
(12) .
Disaster workers report that identification with the dead and their families is particularly stressful, including feelings of “It could have been me,” “It could have been my spouse,” or “It could have been my friend”
(3,
13). Identification is a cognitive mechanism that has traditionally been seen as anxiety- and distress-reducing, as well as a normative aspect of cognitive development as children identify with their parents. However, identification may also be a risk factor for illness, serving as a cognitive mechanism by which symptoms are formed
(14).
Identification has long been a focus of attention in the study of the psychiatric effects of disasters and traumatic events; however, it has not been empirically investigated. Identification with deceased victims is not unique to disaster workers. Identification with the deceased was described in bereaved victims of the Coconut Grove fire in Boston
(15) and in community members after the crash of a commercial airliner in 1978
(16). Bereaved victims manifested traits and mannerisms of the deceased and imagined what their own last thoughts, feelings, and experiences would have been in the same situation. Such thoughts and feelings are different from previously described dissociative experiences in that they do not include any disturbance in time, person, or place (i.e., dissociation) and are not intrusive thoughts about the disaster, since the individuals were never involved in the disaster. Identification is a more complex cognition than intrusive thoughts and includes voluntary and involuntary active imagining.
Studies also suggest an increase in physical health problems and health care utilization associated with exposure to traumatic events and disaster
(6,
17,
18). Higher rates of somatization and physical complaints have been found in disaster workers working with the dead
(8) and Operation Desert Storm troops performing graves registration duties
(11).
The present study extended our initial findings of exposure to traumatic death as a specific risk factor for PTSD by examining identification with the deceased as a mechanism for the development of acute and chronic PTSD, posttraumatic symptoms including somatization, and health care utilization. The subjects were volunteer disaster workers who participated in the body recovery and identification of sailors left dead after a gun turret explosion on the USS Iowa naval ship. These individuals were followed longitudinally during the year after the explosion and assessed 1, 4, and 13 months after the disaster.
On April 19, 1989, north of Puerto Rico, on the USS Iowa, gun turret 2 exploded. In the gun turret the crew had carried out their work surrounded by 17 inches of steel. The steel protection, designed to keep potential enemy fire out, entombed the men caught in the mishap. Of the 1,500 sailors on board, all 47 in the gun turret died. The bodies of the dead sailors were taken to Dover Air Force Base, Delaware, for identification, autopsy, and placement in caskets. Approximately 98 individuals from the Dover Air Force Base community quickly volunteered to assist the 28 professionals in the mortuary. These disaster workers were highly motivated and committed to their work, feeling that the victims were fellow members of the military. A total of 71 individuals actually assisted in the mortuary. Before the arrival of the bodies, all disaster workers received a briefing and orientation. The disaster workers moved the bodies through the identification process on gurneys and assisted in the autopsies, embalming, placement in caskets, and sorting of personal effects and in administrative duties. Most of the bodies were intact, with many still in their clothing; however, some were damaged beyond recognition. Nearly all of the disaster workers spent many hours surrounded by the dead, going home in the evening and returning to the mortuary the next day. The bodies were identified over a 3-day period, and the volunteers returned to their usual work after some time off. The research team was present throughout the 3-day period.
METHOD
Approximately 2 weeks after the mortuary work, we contacted the 71 volunteers who had worked in the mortuary. After the study was described, the volunteers who agreed to participate (N=54; 76% response rate) gave written informed consent and completed assessments. Those who agreed to participate in the study did not differ from those who did not. The median date for completion of the time 1 assessment was 1 month after the disaster. Of the 54 time 1 participants, 41 participated at time 2 (76% response rate), for which the median completion date was 4 months after the disaster. At time 3, 44 (81%) of the 54 participated, and the median completion date was 13 months after the disaster.
The majority of the subjects (91%, N=49) were male, and the mean age was 29 years (range=19–48 years). The majority were white (83%), were married (83%), were enlisted members of the U.S. Air Force (96%), and had at least some college education (83%). Approximately 48% of the subjects had previous disaster work experience. Individuals participating at 1, 4, and 13 months did not differ significantly on any demographic variables.
Measures
Identification with the dead.
Identification with the dead was assessed at 1 month with five items: “It could have been me;” “One of the victims reminded me of a close friend or relative;” “It could have been my spouse;” “It could have been my son;” and “It could have been my father.” Subjects scored each identification item on a 4-point scale ranging from 1 (not at all) to 4 (very much). Items were then recoded into dichotomous responses: no (not at all) and yes. The items for spouse, son, and father showed high internal consistency (Kuder-Richardson coefficient=0.82), and in chi-square analyses the three items were significantly associated (all p values <0.0001). Therefore, these three items were combined into one variable, identification–family (scored yes if any one item was scored yes). Thus, we examined three types of identification: identification–self, identification–friend, and identification–family. At 1 month, each subject was coded as an identifier (scored yes) or nonidentifier (scored no) separately for each of the three identification types.
The Impact of Event Scale (19).
This widely used 15-item self-report scale was used at the three assessment times to measure intrusive and avoidant posttraumatic symptoms. Standard scoring was used, with items scored on a 4-point scale, rescaled, and summed to yield scores for intrusive and avoidant symptoms and total symptoms. Horowitz et al.
(19) found a correlation of 0.42 between the intrusion and avoidance subscales; however, the subscales did not measure identical constructs. Several studies
(20,
21) found that the subscales discriminated across populations and detected change over time. In our study, intrusive and avoidant symptoms were measured retrospectively; however, the time interval was relatively brief (approximately 1.5 to 2 months after the disaster).
The SCL-90-R (22).
This scale was used at all three assessment times to determine other symptoms. This self-report checklist inquires about symptoms during the preceding week. It is composed of 90 items that are scored on a 5-point scale (0=not at all, 1=a little bit, 2=moderately, 3=quite a bit, 4=extremely). The SCL-90-R provides a global index of symptoms reported and intensity-of-distress scores for nine subscales: somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, phobic anxiety, hostility, paranoid ideation, and psychoticism. Reliability coefficients for the subscales range from 0.84 to 0.90, and the subscales correlate fairly highly with MMPI scales measuring similar constructs. The SCL-90-R has proven useful in other research on disasters and has been administered to a variety of community samples. We examined only scores on the SCL-90-R global severity index and the subscales that might be affected by trauma: anxiety, depression, hostility, and somatization.
PTSD
We identified PTSD by means of the DSMPTSD-IV scale
(8,
23–
26). This scale uses the SCL-90-R, 12 supplemental items scored similar to those on the SCL-90-R, and the Impact of Event Scale to identify subjects who meet the DSM-IV criteria for PTSD symptom distribution. The DSMPTSD-IV scale has good sensitivity and specificity when compared with diagnoses from the Structured Clinical Interview for DSM-IV in community samples
(26,
27).
Health care utilization
Health care utilization was assessed separately for three time periods: up to 1 month after the trauma, 1–4 months afterward, and 4–13 months afterward. A yes/no response was given for the following three questions: Have you obtained any medical care during this time for 1) an annual physical? 2) physical problems? 3) emotional or family problems?
Data Analyses
Initial t tests and chi-square tests determined between-group differences (identifiers versus nonidentifiers) in demographic variables for each of the three types of identification (identification–self, identification–friend, and identification–family). We calculated mean Impact of Event Scale and SCL-90-R scores for each of the three types of identification at each time point (1, 4, and 13 months after the disaster). For each identification type we performed repeated measures multivariate analyses of variance (MANOVA) to determine any differences due to time, differences between groups, or group-by-time interactions. MANOVA was also used on multiple outcomes simultaneously, i.e., on the Impact of Event Scale intrusion and avoidance subscales and on the SCL-90-R subscales (anxiety, depression, hostility, and somatization). When appropriate, we then used MANOVA and t tests to examine the differences between the two groups on the various subscales at the various times. We did not explore time effects when there was no group effect or group-by-time interaction, since they were not relevant to this study. To control for experimentwise error, when we examined PTSD and health care utilization for each of the identification types, we first examined the association of identifiers and nonidentifiers across all three times—using only the data of the subjects who were present for all three assessments—with chi-square analysis. If there was a significant finding, we then proceeded to examine each assessment point. Significance level was set at p=0.05. SAS software
(28) was used for all statistical analyses.
RESULTS
Of the 54 disaster workers, 74% (N=40) were classified as identifier–self and 26% (N=14) as nonidentifier–self; 30% (N=16) as identifier–friend and 70% (N=38) as nonidentifier–friend; and 41% (N=22) as identifier–family and 59% (N=32) as nonidentifier–family.
Identification–Self
Subjects who identified with the deceased as self did not differ demographically (age, race, marital status, military rank, and education) from those who did not identify with the deceased as self (nonidentifiers).
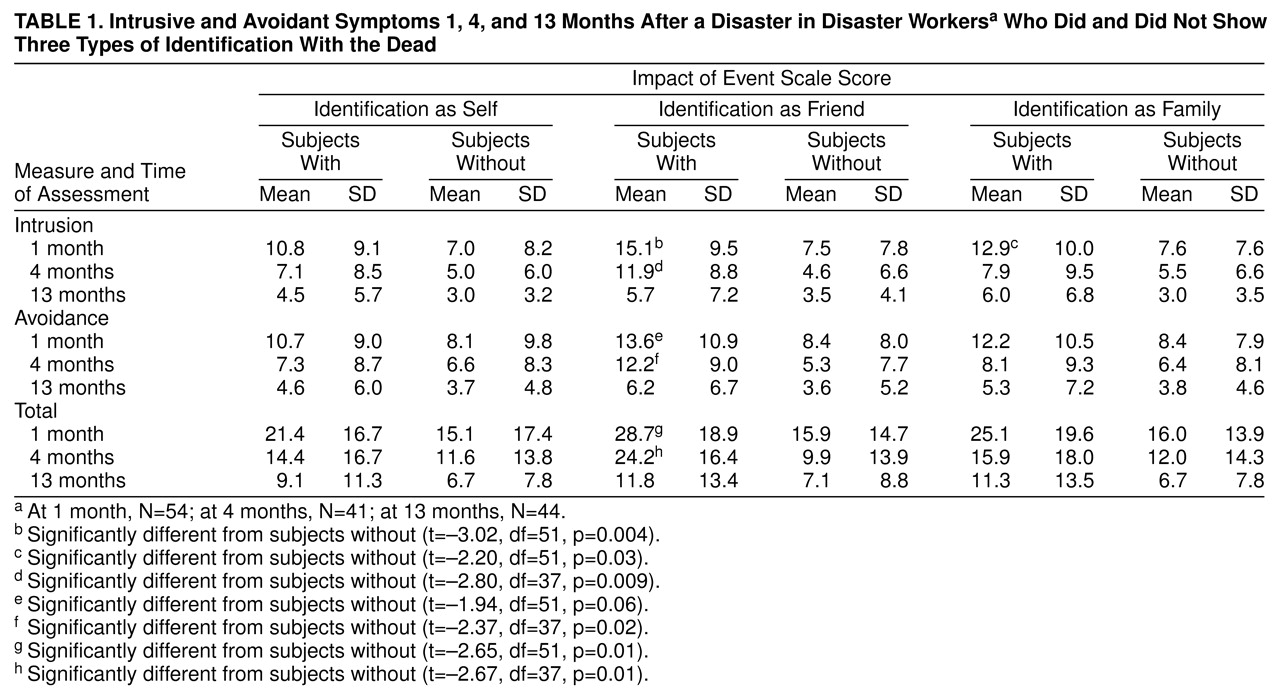
We examined differences in Impact of Event Scale total score between the subjects who did and did not identify with the deceased as self (identifier–self versus nonidentifier–self) with the use of repeated measures MANOVA (
table 1). No significant group or group-by-time effects were found, but there was a significant change over time (Wilks’s lambda=0.559; F=11.43, df=2, 29, p=0.0002). Using a repeated measures MANOVA to examine the intrusion and avoidance subscale scores, we found no significant group or group-by-time effects, but again there was a significant time effect (Wilks’s lambda=0.540; F=5.74, df=2, 27, p=0.002). Further examination using a repeated measures MANOVA showed significant change over time for both intrusion (Wilks’s lambda=0.627; F=8.64, df=2, 29, p=0.001) and avoidance (Wilks’s lambda=0.616; F=9.05, df=2, 29, p=0.0009) and again no group or group-by-time effects.
There was no significant association between PTSD and subjects who did and did not identify with the deceased as self.
Repeated measures MANOVA showed no significant group, time, or group-by-time effects for the global severity index of the SCL-90-R (
table 2). Similarly, repeated measures MANOVA showed no significant group, time, or group-by-time effects for the SCL-90-R subscales (anxiety, depression, hostility, and somatization).
There was no significant association between health care utilization and subjects who did and did not identify with the deceased as self.
Identification–Friend
Subjects who identified with the deceased as a friend were younger (mean age=25.1 years, SD=4.38) than those who did not identify with the deceased as a friend (mean=30.5 years, SD=6.92) (t=2.87, df=53, p=0.006). Chi-square analysis indicated a marginal difference in rank between identifiers and nonidentifiers (χ2=5.37, df=2, p=0.07): 37.5% (N=6) of the identifiers ranked E1–E3, 50.0% (N=8) ranked E4–E5, and 12.5% (N=2) ranked E6 or above, as compared with 36 of the nonidentifiers: 11.1% (N=4); 61.1% (N=22); and 27.8% (N=10), respectively. There were no other demographic differences between the two groups.
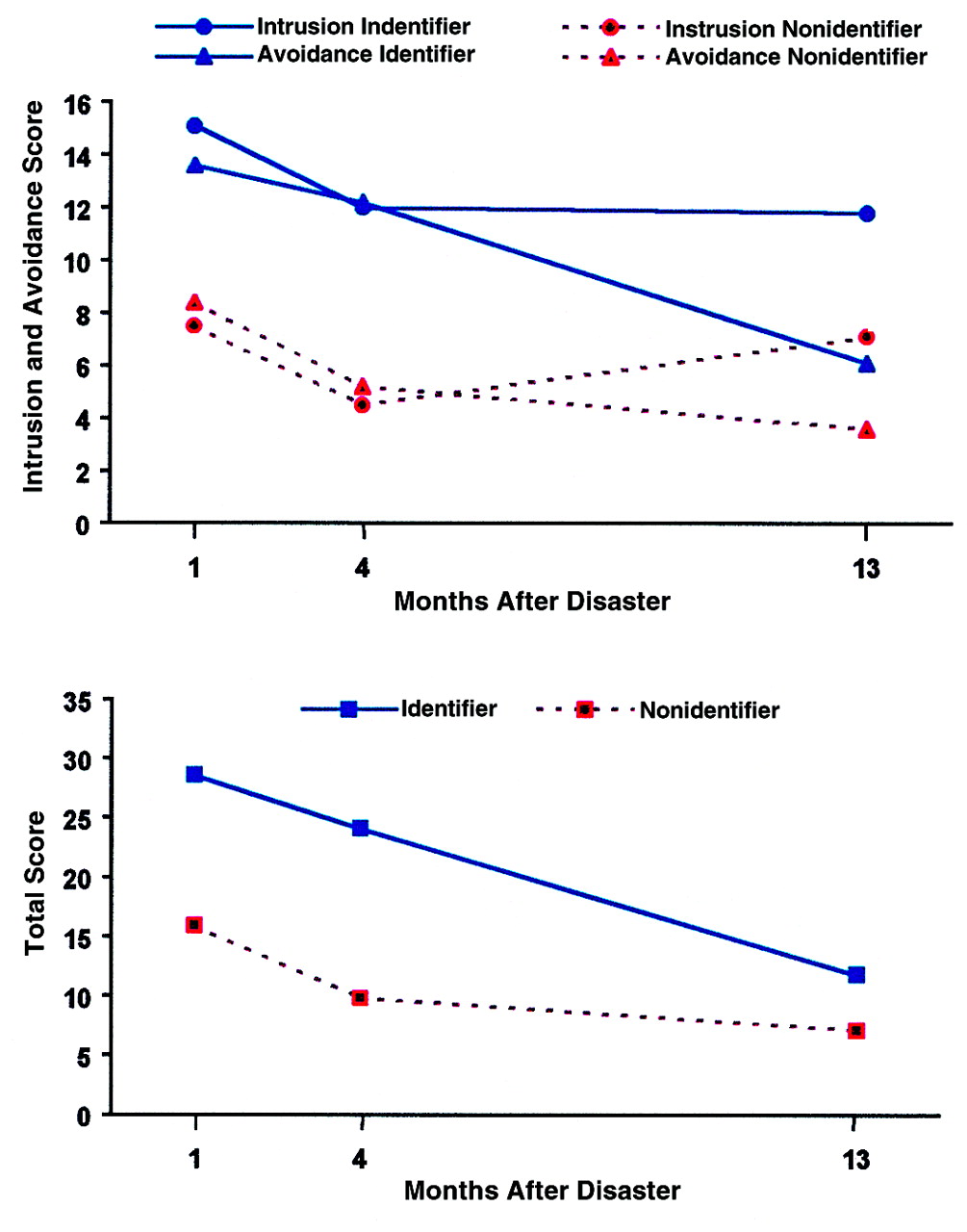
We examined differences in Impact of Event Scale total score between subjects who did and did not identify with the deceased as friend (identifier–friend versus nonidentifier–friend) by means of repeated measures MANOVA and found a significant group effect (Wilks’s lambda=0.696; F=6.34, df=2, 29, p=0.005), group-by-time effect (Wilks’s lambda=0.966; F=6.39, df=2, 29, p=0.005), and time effect (Wilks’s lambda=0.330; F=9.37, df=1, 30, p=0.005) (
figure 1). Those who identified with the deceased as a friend had higher total Impact of Event Scale scores 1 month after the disaster and 4 months after the disaster than did the nonidentifiers (
table 1).
A repeated measures MANOVA for Impact of Event Scale intrusion and avoidance scores revealed a significant group effect (Wilks’s lambda=0.762; F=5.40, df=2, 29, p=0.01), group-by-time effect (Wilks’s lambda=0.684; F=3.12, df=4, 27, p=0.03), and time effect (Wilks’s lambda=0.317; F=14.57, df=4, 27, p=0.0001) (
figure 1). For intrusion, repeated measures MANOVA revealed a significant group effect (Wilks’s lambda=0.945; F=11.13, df=1, 30, p=0.02), group-by-time effect (Wilks’s lambda=0.972; F=5.81, df=2, 29, p=0.008), and time effect (Wilks’s lambda=0.386; F=23.03, df=2, 29, p=0.0001). Identifiers had higher intrusion scores than did nonidentifiers 1 month after the disaster and 4 months afterward (
table 1). For avoidance, repeated measures MANOVA showed a significant group effect (Wilks’s lambda=0.981; F=6.43, df=1, 30, p=0.005), group-by-time effect (Wilks’s lambda=0.977; F=3.66, df=2, 29, p=0.04), and time effect (Wilks’s lambda=0.429; F=19.26, df=2, 29, p=0.0001). Identifiers had higher avoidance scores than did nonidentifiers 1 month after the disaster and 4 months afterward (
table 1).
Of the subjects who identified with the deceased as a friend, 33% (N=3) had PTSD at sometime during the follow-up, compared with only 4.5% (N=1) of the nonidentifiers (χ 2=4.71, df=1, p=0.03). Given this finding, we examined the relationship of PTSD and identification–friend for each time separately. At 4 months, 27% (N=3) of the identifiers had PTSD, compared with 4% (N=1) of the nonidentifiers (χ 2=4.61, df=1, p=0.03). There were no differences in the proportions of subjects with PTSD at 1 month and 13 months.
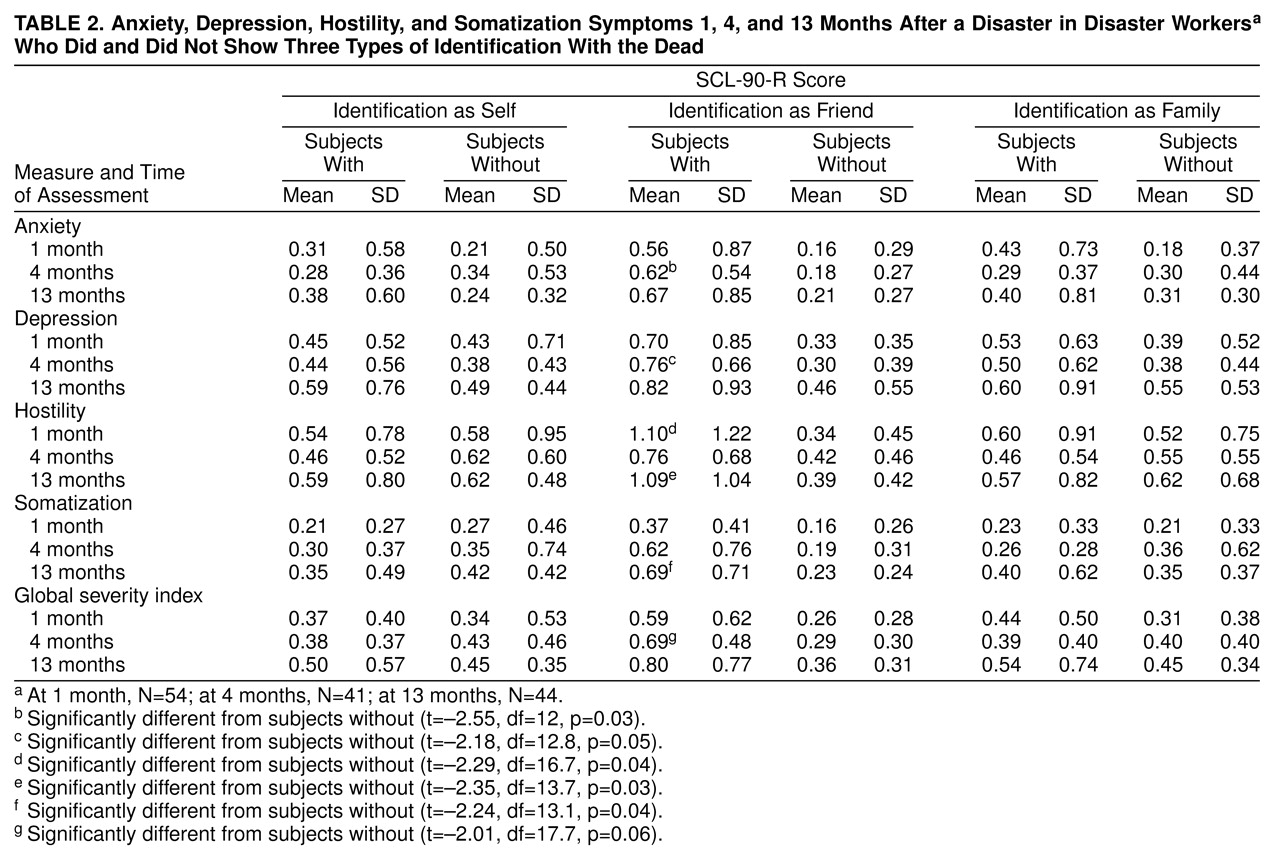
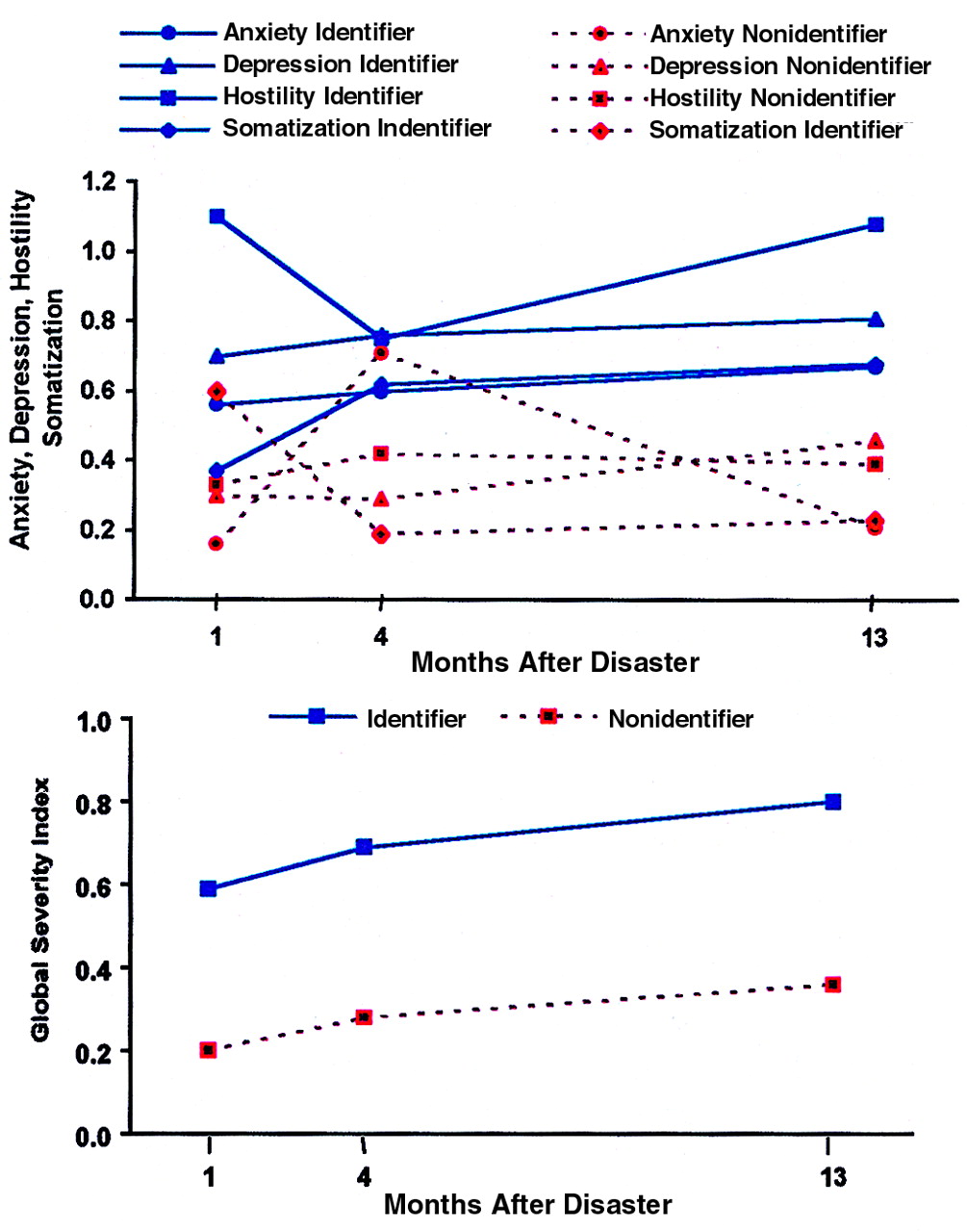
A repeated measures MANOVA of the global severity index scores on the SCL-90-R showed a significant group effect (Wilks’s lambda=0.672; F=15.10, df=1, 31, p=0.0005) (
table 1). At 4 months, identifiers had significantly higher scores than nonidentifiers (table 2). No effects of time or group by time were present. Repeated measures MANOVA of the four SCL-90-R subscale scores (anxiety, depression, hostility, somatization) revealed a significant group effect (Wilks’s lambda=0.533; F=5.90, df=4, 27, p=0.002). No group-by-time effect was present; however, there was a borderline effect of time (Wilks’s lambda=0.550; F=2.30, df=8, 23, p=0.06). A repeated measures MANOVA of each of the four subscale scores showed significant group effects for all four: anxiety (Wilks’s lambda=0.644; F=17.10, df=1, 31, p=0.0003), depression (Wilks’s lambda=0.779; F=8.79, df=1, 31, p=0.005), hostility (Wilks’s lambda=0.685; F=14.23, df=1, 31, p=0.0007), and somatization (Wilks’s lambda=0.712; F=12.12, df=1, 31, p=0.0012) (
figure 2.). Examination of the means for anxiety shows that at 4 months, identifiers scored significantly higher than nonidentifiers (table 2). Similarly, the mean score on depression at 4 months was significantly higher for the identifiers than the nonidentifiers. On hostility the identifiers scored significantly higher than the nonidentifiers at 1 month and at 13 months. On somatization the identifiers’ scores were significantly higher than those of the nonidentifiers at 13 months. With respect to time effects, only the effect on somatization was significant (Wilks’s lambda=0.752; F=4.78, df=2, 30, p=0.02).
There was no significant association between health care utilization and subjects who did and did not identify with the deceased as a friend.
Identification–Family
The majority (95.4%, N=21) of the subjects who identified with the deceased as a family member were currently married. Of the nonidentifiers, 75.0% (N=24) were married (χ2=3.93, df=1, p=0.05). No other demographic variables were significantly different between the two groups.
A repeated measures MANOVA for Impact of Event Scale total score showed a borderline group effect (Wilks’s lambda=0.885; F=3.90, df=1, 30, p=0.06) but no significant group-by-time effect (table 1); there was a significant effect of time (Wilks’s lambda=0.421; F=19.98, df=2, 29, p=0.0001). Repeated measures MANOVA showed no significant group or group-by-time effect for intrusion and avoidance modeled together, but as expected, there was a significant time effect (Wilks’s lambda=0.411; F=9.68, df=4, 27, p=0.0001). Repeated measures MANOVA for avoidance showed no group or group-by-time effect, but there was a significant time effect (Wilks’s lambda=0.493; F=14.89, df=2, 29, p=0.0001). For intrusion the group-by-time effect was not significant; however, there was a significant group effect (Wilks’s lambda=0.842; F=5.62, df=1, 30, p=0.02) and time effect (Wilks’s lambda=0.493; F=14.91, df=2, 29, p=0.0001). One month after the disaster, the scores on intrusion were higher for the subjects who reported identifying with the deceased as a family member than for those who did not (table 1).
Repeated measures MANOVA showed no significant group, time, or group-by-time effects on scores on the global severity index as well as the SCL-90-R subscales together (table 2).
There was no significant association between health care utilization and subjects who did and did not identify with the deceased as a family member.
DISCUSSION
Several researchers have observed an association between PTSD and identification with the deceased in disaster workers exposed to dead bodies
(8,
13,
14,
29). This study is the first empirical examination of this observation. Importantly, subjects were exposed to only one aspect of disaster trauma, working with the dead. This provided the opportunity to examine exposure to traumatic death without the confounding effects of other disaster stressors. In addition, the subjects were followed longitudinally over the year after the disaster. The results of our study indicate that identification is both common and frequent, occurring in nearly 75% of disaster workers exposed to deceased victims. In addition, identification with the dead, particularly as a friend, is associated with higher rates of PTSD and greater intrusion, avoidance, and somatization, both acutely and over the long term.
Our findings are consistent with the notion that identification is not only a risk factor for negative outcomes but also a mechanism by which exposure to the dead leads to disease and symptoms in disaster workers. The longitudinal nature of this study decreases the possibility that the association of identification with negative outcome is a measurement effect, since identification was measured only at 1 month after the disaster yet predicted later outcomes. It is not clear, however, whether 1) exposure to deceased victims activates identification and subsequently the development of symptoms, 2) some individuals who are characteristically identifiers are a high-risk group for this particular type of exposure, or 3) identifiers are generally at risk of more psychiatric illness and symptoms regardless of exposure. The fact that all types of identification were not equally predictive of PTSD and other symptoms (i.e., identification with the victim as a friend was specifically associated with negative outcome) supports some specificity in the identification process rather than a global identifier trait. The fact that younger individuals were more likely to report identification with the deceased as a friend might also provide an explanation for the often reported finding that younger individuals exposed to death and trauma are at greater risk of negative outcomes
(5,
30). Perhaps the specific recall of friends (i.e., “chumships”) is related to developmental experiences of friend formation in childhood. Certainly it highlights the often neglected role of friendships in adult development.
The study of the mechanisms by which somatic symptoms and health care utilization are related to PTSD is complicated by the known association of increased rates of PTSD among persons who are injured in a disaster or traumatic event
(31–
33) and the increased smoking
(17) and accidental injury
(34) associated with chronic PTSD. Since participants in our study had no injuries, were not exposed to other disaster stressors, and suffered primarily from acute PTSD, the finding of increased levels of somatization in the identification–friend group (but no increase in health care utilization) is of particular interest. The identifier group may have had an increased awareness of physical frailty and bodily health issues, either prior to or as a result of their exposure to deceased victims. Better measures of health care utilization may be helpful in identifying potential costs of somatization or clarifying the relationship between somatic complaints and health care utilization
(18) in PTSD.
Several important limitations should be considered in interpreting the results of our study. A larger number of subjects would have been preferable in order to increase the level of confidence in our results. To generalize our findings to other disaster populations, a more diverse study group, allowing for examination of possible contributions of demographic variables, would also have been preferable. Although we used self-reports to assess both predictor and outcome variables, we used previously validated scales or scale items. Future studies should address the measurement of identification with the dead—both frequency and intensity—to further understand the relationship of identification with the deceased to PTSD and somatization.
Beyond these methodological considerations, this study suggests that the association of PTSD, disaster-related intrusive and avoidant symptoms, and general symptoms (including anxiety, depression, hostility, and somatization) with identification with the dead in disaster workers is prominent and mediated by the time since the disaster work and, importantly, by the type of identification (i.e., friend versus self and family). Further study of the causes of identification—psychological, contextual, and neurobiological—particularly identification–friend, are important to understanding this stress-illness process. If identification is a causative mechanism, interventions directed to decreasing identification should also decrease negative outcomes.