Dissociative symptoms refer to disruptions in the usually integrated functions of consciousness, such as memory, identity, and perception of the environment (DSM-IV, p. 477). The theoretical assumption that dissociation is primarily a response to overwhelming experiences, especially in childhood
(1,
2), is currently questioned
(3–
5). What is the empirical evidence for this assumed relationship? And, if there is a relationship, is the level of adult dissociation directly associated with early trauma per se, or are other pathogenic factors in childhood relevant as mediators? The term “trauma” is here restricted to psychologically overwhelming experiences inducing fear and helplessness.
Empirical evidence supporting the relation between trauma and dissociation is based on three sources: 1) studies on the relation between dissociation and trauma in adulthood, 2) research examining links between childhood trauma and adult dissociation, and 3) prospective studies of children. Regarding the first source, elevations in the level of dissociation have been demonstrated in adults during or shortly after a traumatic event
(6–
10) as well as long after an overwhelming event
(11). Childhood trauma could be a precursor for these dissociative tendencies, since higher dissociation levels have been found in rape victims reporting childhood sexual abuse than in nonabused rape victims
(12).
Research examining the relation between childhood trauma and adult dissociation has focused primarily on sexual and physical abuse. In particular, sexual abuse, its severity, and its combination with physical abuse have been found to be strongly related to adult dissociation measured by either the Dissociative Experiences Scale
(13–
20) or the Structured Clinical Interview for DSM-III-R Dissociative Disorders (SCID-D)
(21,
22). Two studies
23,
(24) indicated that physical abuse was more important than sexual abuse in the explanation of adult dissociation.
Finally, in prospective research
(25) sexually abused girls had significantly higher initial and 1-year follow-up dissociation levels than nonabused control subjects.
Little is known, however, about the effect of co-occurring distressing circumstances such as parental loss or separation, witnessing interparental violence, and the more chronic adverse circumstances of neglect. Epidemiological research has demonstrated that neglect is a risk factor for later psychopathology in general
(26,
27) and that parental loss is a risk factor for adult depression
(28). Furthermore, in community samples of women, parental dysfunction, interparental violence, and separation from parents were related to sexual and physical abuse as well as to general adult psychopathology
(29,
30). Parental dysfunction and sexual and physical abuse, both in childhood and in adulthood, have been found to be independent predictors of adult psychopathology
(31). In addition, some writers consider dissociative identity disorder primarily an attachment disorder, highlighting the relevance of disturbed attachment relationships in which a child grows up
(32,
33).
Given the interrelationship among family pathology, neglect, early separation, and childhood abuse, which experiences are central in the etiology of dissociation? Empirical findings on the importance of neglect compared with abuse are inconclusive. In one study
(5) the relation between dissociation and sexual abuse disappeared when family pathology was controlled for. In a nonclinical population, loss in the family and intrafamilial and extrafamilial sexual abuse, rather than abuse alone, predicted the level of adult dissociation
(34). Early separation from parents was significantly more often reported by patients with dissociative disorder than by control patients with other axis I diagnoses but was reported as often by patients with cluster B personality disorders; pathological dissociation was strongly related to sexual and physical abuse but only slightly related to early separation and witnessing interparental violence
(22). Among sexually abused female inpatients, physical neglect and witnessing sexual abuse or physical abuse were associated with higher levels of dissociative symptoms, but childhood stressors involving loss were not. A close relationship with a parent, sibling, or friend did not have a mediating effect
(35). Nor did—in a nonclinical sample—perceived availability of emotional support in childhood eliminate the relation between childhood trauma and dissociation
(36). We may conclude that neglect (conceptualized in a variety of ways) and separation from parents, in addition to overwhelming intimate experiences such as childhood abuse, may be precursors of dissociation.
The present study was designed to examine the predictive value of childhood trauma, prolonged separation, and neglect in the development of adult dissociation. It was hypothesized that besides neglect (conceptualized as parental dysfunction) and separation from a parent (due to divorce, illness, or death), overwhelming childhood experiences (witnessing interparental violence and, in particular, sexual and physical abuse) would uniquely contribute to the level of dissociative symptoms in an adult psychiatric inpatient population.
METHOD
Instruments
The Dissociative Experiences Scale
(13) is the most widely used screening instrument for dissociative symptoms in clinical samples. Good reliability and good clinical validity have been reported at different centers in North America
(13,
37,
38) and in The Netherlands
(39,
40). The scale, a 28-item visual analogue self-report instrument, contains items referring to amnesia, depersonalization, derealization, absorption, and identity alteration.
The Structured Trauma Interview
(41) is an adapted version for psychiatric patients of the interview developed for a national survey on the prevalence and sequelae of child sexual and physical abuse and perceived neglect
(29). It addresses childhood experiences proven to be risk factors for adult psychopathology (early separation from parents, parental dysfunction, parental physical aggression, sexual abuse, witnessing interparental violence, and other overwhelming experiences before age 16); “parents” includes stepparents and adoptive parents. Adult sexual and physical assault is addressed as well. Although the Structured Trauma Interview has been used in several studies, no data on its validity have been published yet.
Neglect was defined as parental dysfunction or unavailability resulting from recurrent illness, nervousness, depression, alcohol misuse, and use of sedatives. The choice to conceptualize neglect in terms of parental dysfunction is based on the fact that it refers to factual, observable behavior of the parents instead of more subjective indications of their unavailability or lack of affection. Questions were: “Was your (step/adoptive) mother often ill? Was she nervous, tense? Was she depressed? Did she use a lot of alcohol? Did she use sedatives, as far as you know?” The same questions were asked with respect to fathers. Answers were coded in a yes/no format (unclear answers were coded as no). A total score for each parental figure was based on these questions; their internal consistency was reasonable (Cronbach’s alpha for dysfunction of mother: 0.64; for dysfunction of father: 0.65). This measure of neglect was validated by its relation to lack of maternal and paternal affection as measured by the Parental Bonding Instrument
(26) (Pearson’s r=–0.49 and –0.38, respectively, N=1,054, p<0.0001)
(29).
Early separation was defined as the loss of, or separation from, a natural parent or caretaker by death, divorce, illness, foster care, or other reasons before age 12 during a period of at least 6 months.
Physical abuse was defined as severe parental aggression. Parental aggression included physical punishments by parental figures that could have hurt the child physically. Questions were: “Sometimes parents hit their children as a disciplinary measure or because they lose their temper. If your parents wanted to punish you, what did they do? How often do you remember that your parents hit you? If you try to remember the occasions they hit you, which made the biggest impression on you?” Frequency and severity of parent-to-child violence before age 16 were assessed according to the Conflict Tactics Scales
(42). Instances of culturally accepted corporal punishment were not rated as abusive. On the basis of a qualitative analysis comparing aspects of physical aggression (i.e., nature/severity of violence, frequency, duration, injury), a severity index was constructed with scores consisting of absent, mild, moderate, and severe. The mild category included being incidentally hit or kicked, with no injuries. The moderate category included being recurrently hit and/or kicked and incidentally being hit with an object, sometimes leading to injuries such as bruises. The term “physical abuse” was reserved for the category of severe parental aggression. This included recurrent and chronic forms of physical violence that frequently inflicted injuries, such as repeatedly being kicked or hit with a fist or an object (e.g., a stick or a belt), being tied up, or being thrown down stairs.
Sexual abuse was defined as any pressured or forced sexual contact before age 16, ranging from fondling to penetration. The question was: “Nowadays it is clear that many women, but men as well, have had negative sexual experiences in their childhood. Do you know if something like this happened to you?” If the answer was positive, the interviewer inquired about perpetrators, sexual activities, force or pressure, frequency, age at onset, and how upsetting these experiences were at the time. Rape was defined as sexual abuse including penetration. If a patient was sexually abused by more than one perpetrator at different times, the most important incident was chosen by the subject for more detailed inquiry.
Experiences of witnessing physical or sexual violence between parents before age 16 were rated as childhood witnessing of interparental violence.
Procedure
During 18 months all consecutively admitted adult inpatients of a general psychiatric hospital were invited by staff members to participate in the study. According to the national records that follow the ICD, this inpatient population matches the national inpatient population diagnostically. Multiple admissions were treated as one case. Criteria for eligibility included fluency in Dutch, freedom from organic dysfunction, and stabilization that was adequate for giving informed consent. After complete description of the study to the subjects, both written and verbal informed consent was obtained.
The Dissociative Experiences Scale was administered along with other self-report instruments. Participants were interviewed about childhood experiences independently. Interviewers were trained psychiatric nurses, a social worker, and a psychologist who were supervised on countertransference issues during data gathering. Unless patients expressed the wish to share the information with their treating clinicians, research data were kept confidential.
Data Analysis
A series of bivariate analyses were conducted to examine the predictive value of selected childhood experiences. Chi-square tests with Yates’s correction and two-tailed t tests were used where appropriate. When cell sizes were 5 or less, we used Fisher’s exact test of probability. Multivariate stepwise regression analysis was used to examine the relative importance of childhood trauma for the explanation of the variance in dissociation.
RESULTS
Of 313 admitted patients, 182 were willing and able to participate. However, 15 patients refused to participate during data gathering, and another seven participated as “pilot subjects,” leaving 160 subjects (51.1%). The main reasons for nonparticipation were a hospital stay that was too short to administer all instruments (39%), refusal (35%), and permission not granted by the treating clinician (19%).
More women (N=94) than men (N=66) participated (χ2=10.08, df=1, p<0.005), fewer participants lived alone (43%, versus 59% of the nonparticipants; χ2=14.70, df=4, p<0.005), and fewer were unemployed (53%, versus 71% of the nonparticipants; χ2=34.34, df=3, p<0.0001). The participants were slightly younger than the nonparticipants (mean age=35.6 years, SD=12.0, and mean=38.5 years, SD=14.0, respectively; t=1.97, df=310, p<0.05). They did not differ in the number of psychiatric hospitalizations.
Some demographic differences may be explained by the fact that patients suffering from psychosis or schizophrenia were often considered unable to participate by their treating clinician; 36% of the participants suffered from psychotic symptoms, compared with 62% of the nonparticipants (χ2=17.13, df=1, p<0.0001). More participants (41%) than nonparticipants (25%) met the criteria for a DSM-III-R axis II diagnosis (χ2=7.98, df=2, p<0.05). As axis II diagnoses are made over time, this difference could be a bias resulting from the short hospital stays among the nonparticipants. Thus, the study group was selective mainly toward including more nonpsychotic patients. This bias is inherent to clinical research.
No adverse consequences of the standardized interview were observed.
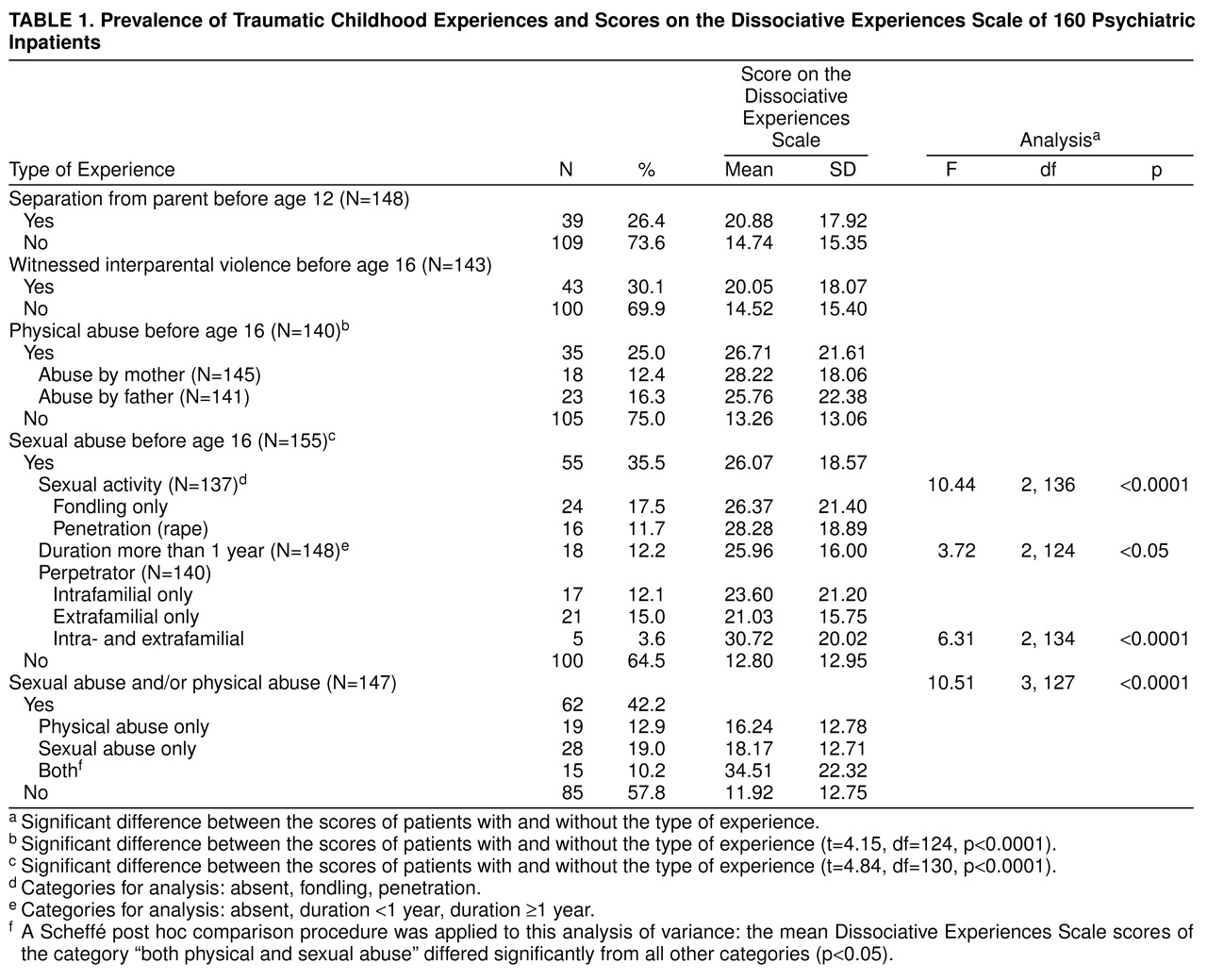
Table 1 presents both characteristics of childhood trauma and their prevalence. To a certain extent, childhood experiences were interrelated: early separation from a parent was related to sexual abuse (r=0.20, N=147, p<0.05), to physical abuse (r=0.17, N=148, p<0.05), and to witnessing interparental violence (r=0.25, N=143, p<0.01); sexual and physical abuse were related (r=0.18, N=147, p<0.05); and physical abuse was related to witnessing interparental violence (r=0.25, N=143, p<0.05), but sexual abuse was not.
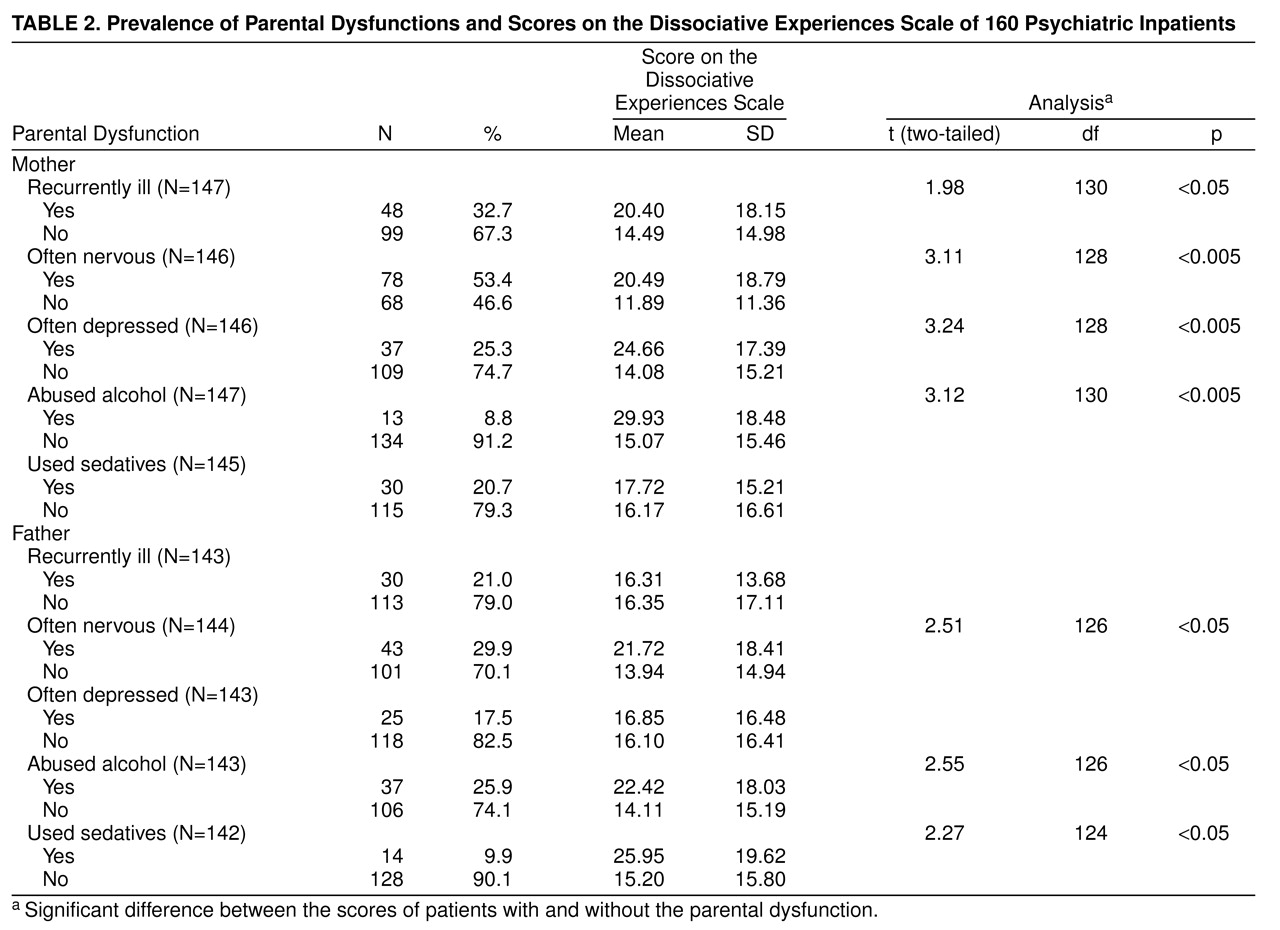
The nature and frequency of parental dysfunction are shown in
table 2. Except for alcohol misuse, mothers were reported to have been dysfunctional more often than fathers. Total scores for each parental figure were only slightly related (Pearson’s r=0.15, N=136, p<0.10). Perceived maternal dysfunction was more closely related to childhood trauma than perceived paternal dysfunction. The level of maternal dysfunction was associated with early separation (r=0.33, N=144, p<0.0001), witnessing interparental violence (r=0.29, N=140, p<0.0001), and sexual abuse (r=0.18, N=143, p<0.05). However, the level of paternal dysfunction was only related to witnessing interparental violence (r=0.25, N=137, p<0.01).
The mean Dissociative Experiences Scale score was 17.4 (SD=16.8, median=12.1, N=139); 25.2% (N=35) of the patients scored beyond 25, and 18.0% (N=25) beyond 30. The scores of male and female patients did not differ. Younger patients scored somewhat higher (r=–0.18, N=139, p<0.05).
The severity of dissociative symptoms was significantly related to reported physical abuse and sexual abuse but not to early separation (
table 1). The severity of sexual abuse (penetration and duration longer than 1 year) was strongly related to the level of dissociation. Highest dissociation scores came from patients who were sexually abused both inside and outside the family or who were both sexually and physically abused.
The severity of dissociative symptoms was also related to perceived parental dysfunction (
table 2): perceived maternal dysfunction due to illness, nervousness, depression, and alcohol misuse and perceived paternal dysfunction due to nervousness, alcohol misuse, and use of sedatives. Highest levels of dissociation were shown by patients who reported having mothers who were heavy drinkers. In terms of the combined total score, maternal dysfunction was associated with dissociation (r=0.32, N=130, p<0.0001); paternal dysfunction was correlated not as strongly (r=0.24, N=126, p<0.01).
Multivariate stepwise regression analysis, using gender and age as control variables, indicated that all trauma and neglect variables together accounted for 23% of the variance in the Dissociative Experiences Scale scores. Physical abuse and sexual abuse were the strongest predictors (both betas=0.24, p<0.01), but maternal dysfunction was significant as well (beta=0.21, p<0.05).
DISCUSSION
Our central question was, What is the predictive value of childhood trauma, in the sense of overwhelming experiences, compared with prolonged separation and neglect due to parental dysfunction in the development of adult dissociation? Although maternal dysfunction in particular turned out to be important in this prediction, sexual and physical abuse each made an independent contribution to the level of adult dissociation.
Given the theoretical overlap between the concepts of abuse and neglect, the correlations between the two were not so strong as to consider abuse and neglect (conceptualized as parental dysfunction) as co-occurring phenomena. Collinearity, though expected, was not really present.
Our findings—indicating that childhood stressors in the form of either severe physical or sexual abuse or repetitive sexual trauma were associated with a higher degree of dissociative symptoms—support previous findings
14,
(16–
20,
25). Multiple victimization, in particular in intimate relationships, seems to reinforce the dissociative response.
Contrary to our expectation, witnessing violence and early separation from a parent did not contribute independently to the level of dissociation when compared with parental dysfunction and other overwhelming childhood experiences. Experiences of parental loss or separation were not related to greater severity of dissociative symptoms, confirming earlier clinical data based on a similar dissociation measure and similar definition of loss
(35), but contradicting results based on different instruments in a nonclinical sample
(34,
36). Apparently, our study needs replication in a nonclinical population.
One explanation for why sexual abuse and physical abuse are related to the level of adult dissociation, and loss or separation are not, may be the secrecy and denial associated with these forms of abuse. Subjectively, the child lives in a fragmented reality, and social support is limited because traumatization occurs through exactly the persons on whom the child is dependent.
The fact that maternal dysfunction is important in the explanation of adult dissociation disconfirms the theoretical assumption of a sheer trauma-related etiology of dissociation. We suppose that dysfunction and unavailability of caretakers contribute to a lack of soothing capacities in the child
(43) and thus to the vulnerability to overwhelming feelings and the use of dissociation as a defense against them. In the early stages of treatment of the dissociative patient, strengthening of the self-soothing capacities or coping skills is very important.
Our findings provide support for the clinical observation that patterns of insecure/disorganized attachment are related to increased levels of dissociation
(31,
32,
44). They also support findings in nonclinical samples that the quality of the object relations (measured by similar parental availability measures and the Parental Bonding Instrument) is a major factor in adult outcome
(28,
30). They support the notion that perceived availability of emotional support in childhood is an important mediator in adult proneness to dissociation
(36).
Our data do not support the view expressed by Nash et al.
(5) that sexual abuse, compared with neglect due to family pathology, is irrelevant in the etiology of adult dissociative symptoms. An explanation of this discrepancy could lie in the weak and unusual dependent measure used in that particular study: scores on two MMPI-based measures of dissociative experiences and the Dissociation Content Scale. In addition, Nash et al. used rather specific criteria for sexual abuse—i.e., involving at least genital manipulation to orgasm of or by the child. Furthermore, the method of statistical analysis they used (analysis of covariance instead of regression analysis) does not allow the inferences that were made
(45).
We may presume that the inconclusive findings thus far on the prediction of dissociation are probably due to weaknesses in the abuse measures and neglect measures as well as in the dissociation measures used.
Some limitations of our study should be noted. It was based on retrospection. The context of family dysfunction may be a risk factor for sexual and physical abuse, but it may also be an artifact resulting from the retrospective projections of helplessness and isolation of abused patients
(46). Nevertheless, it is striking that mothers are perceived as less available than fathers and that the perception of their unavailability is more important in the prediction of adult pathology
(26). Assigning causality is problematic, though, because of the cross-sectional method we used. Also, memory bias could be present among highly dissociative patients: one could hypothesize both underreporting of trauma due to dissociative amnesia and overreporting due to high suggestibility in those patients, although suggestibility has been found not to be related to the level of dissociation
(47). Because of the need for confidentiality, no independent corroborating evidence was sought for any self-reported case of childhood abuse. Therefore, the validity of abuse reports cannot be ensured. Although the bias in the study group (skewed toward less psychotic patients) is a general problem in clinical research, the results should be considered with some reservations. Only 23% of the variance was explained by childhood trauma and perceived parental dysfunction. This suggests that the severity of dissociative symptoms might be accounted for by other factors, such as recent traumatic experiences
(6,
8–
10), stress caused by a psychiatric admission, general distress that made an admission necessary, or other influences. Inpatients in general present high levels of dissociation, of which some are trauma-related and others are not (Friedl and Draijer, manuscript submitted for publication).
The current questions being raised about the etiology and phenomenology of dissociation
(4) should affect the choice, conceptualization, and operationalization of both criterion and predictor variables in empirical research on the precursors of adult dissociation. The limited prediction of the level of dissociation may be partly due to the criterion, the Dissociative Experiences Scale score. The clinical validity of the Dissociative Experiences Scale has been questioned
(3,
4); some of the items of the scale refer to nonpathological dissociation, such as absorption, automatic daily behavior, and imaginative involvement, whereas other items, such as amnesia, depersonalization, and identity alteration, refer to pathological changes in consciousness. Therefore, in future research on the etiology of dissociation, instruments focusing on pathological dissociation, such as a structured clinical interview (SCID-D)
(21) or the Dissociative Experiences Scale-T
(48), should be preferred. Recent stressors should be taken into account as well. The assessment of neglect could be improved by using standardized instruments, such as the Parental Bonding Instrument
(26).
CONCLUSIONS
This study shows that sexual and physical abuse make a unique contribution to the severity of adult dissociative symptoms, compared with neglect due to perceived parental dysfunction. In particular, perceived dysfunction of the mother—her unavailability—seems to be important. Assuming that retrospective perceptions of parental availability refer to a certain extent to external reality, these results could be interpreted as pointing to the importance of early attachments between parent and child, the quality of object relations in early development, or supportive relationships at the time or after the abuse took place. These results call for an integrative approach to the treatment of dissociative patients, combining psychodynamic and trauma theory. They stress the importance of relational issues, such as the necessity of support, the persistence of distrust, and related transference and countertransference issues. We conclude that the criticism of the superficial interpretation of sexual abuse as the sole explanation of a diversity of psychiatric symptoms is correct
(49).