It is well known that depression is twice as common in women as in men, but the origins of this dramatic difference remain obscure
(1). Life stressors have long been hypothesized to be risk factors for depression
(2), and contemporary theories continue to emphasize the role of psychological stress in the etiology of major depressive disorder
(3–
6). Empirical studies support these theoretical formulations; in both case-control comparisons and recent studies of multiple risk factors, exposure to stressful life events is a strong predictor of liability for major depression
(7,
8). Despite the importance of life stressors in predicting depression and the higher rates of depression in women, few studies have directly examined whether stress accounts, at least in part, for the high rates of depression in women. In order to address this issue, it is important to determine whether women are exposed to more stressors, have greater exposure to certain types of stressors, or respond differently to stressors than do men.
The purpose of this article is to examine the empirical data regarding the role of exposure to the specific stressor of childhood sexual abuse in the adult onset of depression, with particular emphasis on whether higher rates of childhood sexual abuse in girls may in part account for the higher incidence of depression in women. Sexual abuse during childhood is a stressor experienced more frequently by girls than boys, with estimates of the incidence of childhood sexual abuse in girls varying from 6% to 62%
(9). This wide range is related to disparate definitions of childhood sexual abuse and differing methods of data collection, but most studies estimate the incidence to be at least 6%–15%
(9). Childhood sexual abuse is considerably less common in males, with the ratio of female to male victims estimated to be as high as 12:1
(10). There is also some evidence that childhood sexual abuse may be particularly pernicious in its effects and that it is more likely to predict the subsequent development of psychiatric illness than does sexual assault occurring in adulthood
(11).
We begin by examining the literature regarding the relationship between childhood sexual abuse and the development of depression in adult women, which demonstrates an association between the two. Next, we present studies comparing the relative impact of childhood sexual abuse on the occurrence of adult-onset depression in women and men, which suggest that boys who are victims of childhood sexual abuse may be less likely to become depressed subsequently than abused girls. We then briefly consider which characteristics of childhood sexual abuse may influence the likelihood of depressive episodes in adulthood.
In the second half of the article, our focus turns to factors, both psychosocial and neurobiological, that may mediate the observed relationship between childhood sexual abuse and adult-onset depression. In particular, we review the evidence suggesting that early stress induces permanent changes in the regulation of the hypothalamic-pituitary-adrenal (HPA) axis, which may result in an increased vulnerability to depression following stress in adulthood. Finally, we hypothesize that there is a sexual dimorphism in the HPA axis response to stress that may create a higher biological vulnerability to depression in women.
EFFECT OF CHILDHOOD SEXUAL ABUSE ON ADULT- ONSET DEPRESSION IN WOMEN
Most studies aimed at understanding the relationship between childhood sexual abuse and adult-onset depression have used all-female study groups. Of these, seven were derived from community populations, five from college women, and nine from clinical populations. The incidence of childhood sexual abuse ranged from 6% to 46% in studies of nonclinical study groups and from 7% to 43% in studies using patient groups for which subjects were not selected on the basis of childhood sexual abuse. Although the retrospective design in all but one of these studies confers methodological limitations, the pattern of results across studies is remarkably consistent. Only one study did not find a higher incidence of adult-onset depression in women who had been abused as children than in women who had not been abused.
Community Studies
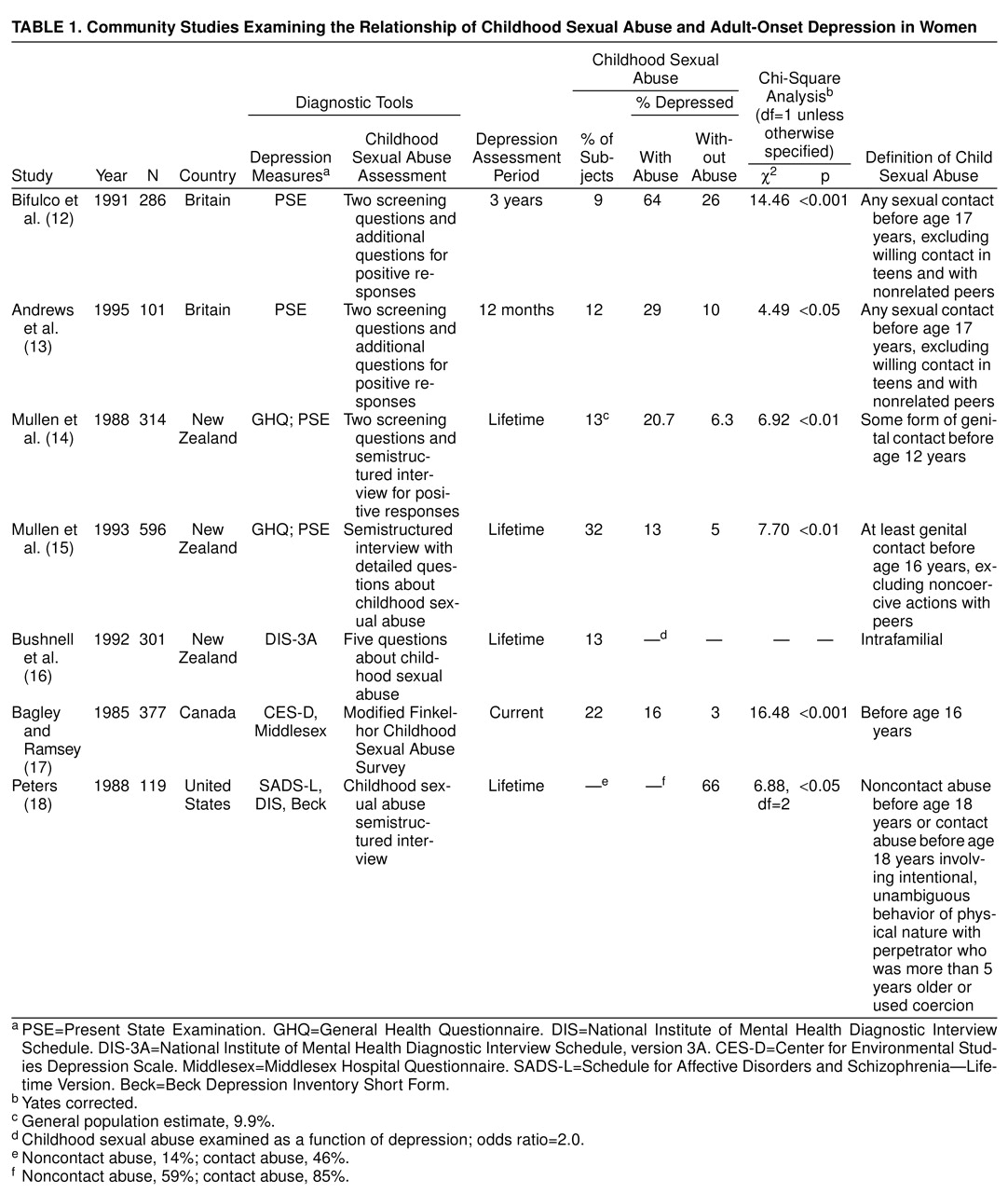
All seven studies using various groups of community-based subjects found a significantly higher occurrence of adult-onset depression in women who reported histories of childhood sexual abuse when compared to those without reported childhood abuse. Although the incidence of depression varied across groups because of differences in population characteristics, ascertainment methods, assessment instruments, and diagnostic criteria, the pattern of results remained the same.
Table 1 summarizes the features and findings of these studies conducted across several different countries.
Two investigations from Britain used randomly selected community samples to study the relationship between childhood sexual abuse and adult-onset depression in working-class mothers. In the first of these studies (N=286)
(12), 64% of women who reported childhood sexual abuse before age 17 years were diagnosed with adult-onset depression during the 3-year study period, whereas 26% of the nonabused women suffered from a major depressive episode. This study attempted to control for the possibility that the presence of depression influenced the reporting of childhood sexual abuse by excluding those subjects who were depressed at the time that a history of childhood sexual abuse was determined. The relationship between childhood sexual abuse and adult-onset depression was maintained in this second analysis (50% versus 15%) (Yates-corrected χ
2=7.50, df=1, p<0.01). In the second random sample of working-class British mothers (N=101)
(13), subjects with a history of childhood sexual abuse were also more likely to be diagnosed with depression during a 12-month period, compared to those without such a history (29% versus 10%). The presence of childhood sexual abuse was identified in both of these studies by using two screening questions, followed by further questioning for those subjects with positive responses. The five community studies described below employed more rigorous methods to determine a history of childhood sexual abuse by means of detailed questioning of all subjects
(14) and use of structured sexual abuse interviews
(15–
18).
In a random sample of 314 women selected from Dunedin, New Zealand
(15), 20.7% of women with a history of childhood sexual abuse met lifetime diagnostic criteria for an adult psychiatric disorder (mostly depressive), but only 6.3% of those not abused met such criteria. These investigators defined childhood sexual abuse as some form of genital contact before age 12, which represented the youngest cutoff age among the community study groups. In a second randomly selected sample of urban New Zealand women, 298 subjects reporting childhood sexual abuse were compared with 298 subjects without reported childhood sexual abuse
(16). A history of major depression was again found to be more common in women who reported past abuse than in those who denied childhood abuse (13% versus 5%). A third study, by Bushnell and colleagues
(14), examined the rates of childhood sexual abuse in 301 urban New Zealand women who met lifetime criteria for an affective disorder, eating disorder, and/or substance use disorder. This study, the only investigation that focused on intrafamilial childhood sexual abuse, found that women with a lifetime diagnosis of depression were twice as likely to report a history of intrafamilial childhood sexual abuse as women who had never been depressed.
Both of the studies from North America examined the lifetime incidence of major depression in community-based study groups. In the first, in which the study group was drawn from a large Canadian city, Bagley and Ramsey
(17) found depression to be significantly more common in women with a history of childhood sexual abuse than women who had not been abused (16% versus 3%). In the second study, the study group was culled from a large sample of Los Angeles county women
(18). Results showed that a significantly greater proportion of women who reported histories of childhood sexual abuse had experienced at least one depressive episode than had women who did not report abuse (85% versus 66%). The high percentage of depressed subjects in this study is likely due to the fact that the subjects were selected from those participating in a larger study of sexual socialization and sexual experiences. In fact, this study reported a 60% incidence of childhood sexual abuse, which was markedly greater than the incidence rates in any of the other six studies.
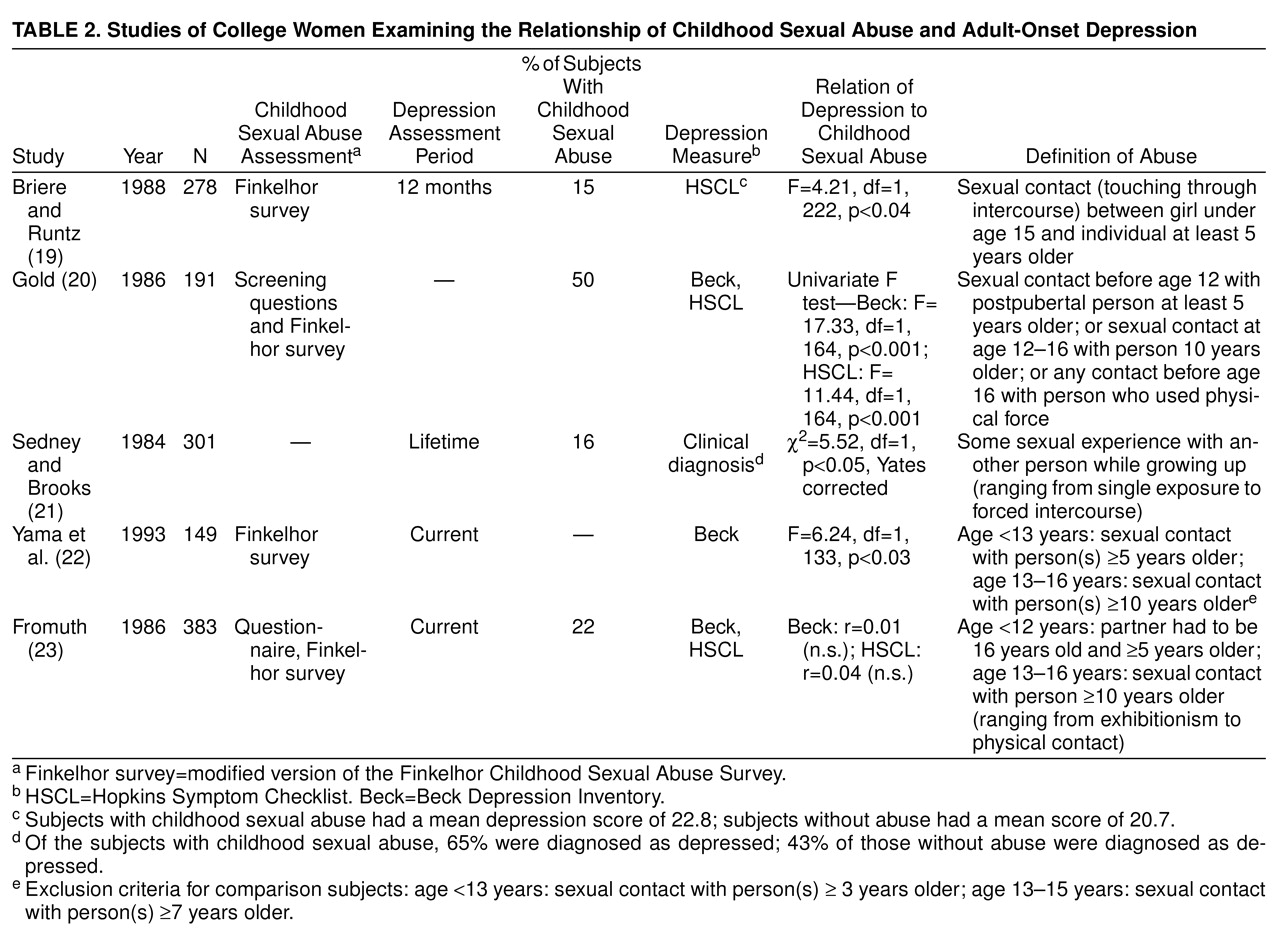
Studies of College Women
Five studies used nonclinical study groups composed of college students to examine the relationship between childhood sexual abuse and adult-onset depression in a high-functioning group. It has been suggested that investigations of college women who report a history of sexual abuse selects for “healthy survivors”—i.e., those who have coped well enough with the effects of past abuse to achieve academic standing at a college level. Nonetheless, four of these studies found a significantly greater incidence of depressive symptoms in those women who reported a history of childhood sexual abuse than those who did not
(19–
22). All five studies assessed depressive symptoms (unlike the community studies, most of which required a diagnosis of depression) and used a variety of symptom checklists.
Table 2 summarizes the features and findings of these studies composed of college women. Symptom severity, as evidenced by itemized or mean scores on symptom scales, was provided only in the study by Briere and Runtz
(19) (table 2).
The one study that failed to find a significant relationship between past sexual abuse and depression
(23) used a relatively broad definition for past abuse. For example, this study classified subjects who reported a one-time “exhibition” as having been sexually abused. Use of this broad definition may have contributed to the lack of an observed correlation between abuse and adult symptoms. However, the study by Sedney and Brooks
(21) also used a broad definition of sexual abuse (“some kind of sexual experience with another person while growing up”), yet found a greater likelihood of depressive symptoms in those with past “sexual experiences.” In contrast, the most stringent definition of childhood sexual abuse was required in the study by Briere and Runtz
(19); these authors found a significant relationship between a history of childhood sexual abuse and a higher rate of chronic depressive symptoms.
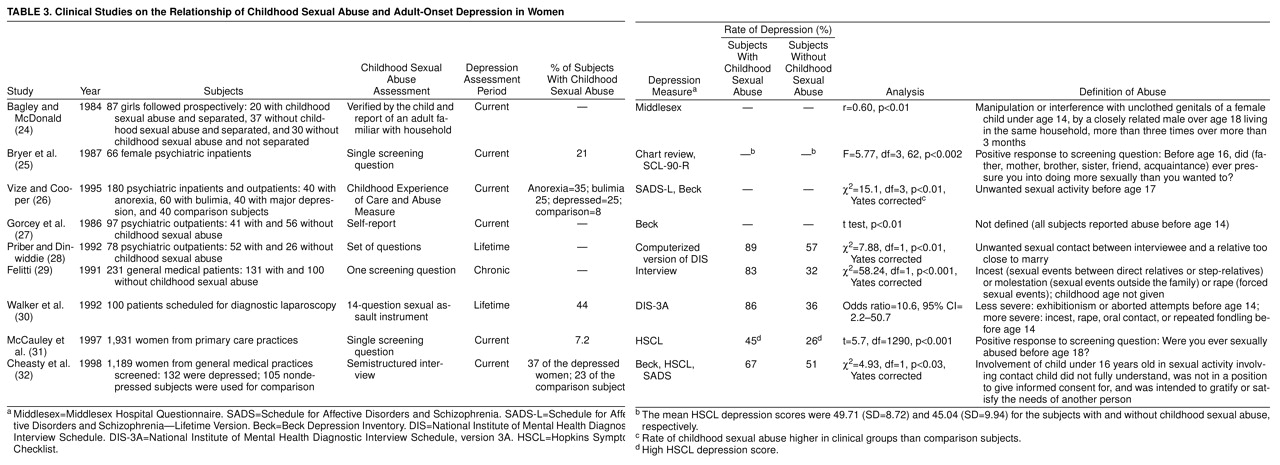
Clinical Studies
Nine studies used subjects from clinical settings to examine the relationship between childhood sexual abuse and adult-onset depression. Although rates of reported childhood sexual abuse might have been higher when studying individuals seeking help, all nine investigations found a significant relationship between a history of childhood sexual abuse and adult-onset depression. The features and findings of these studies examining clinical study groups are summarized in
Table 3.
The only prospective study to investigate the relationship between childhood sexual abuse and adult-onset depression identified and followed a group of girls removed from their homes because of known sexual abuse and compared them with girls separated from their homes (because of disorganization in the home, absence of the mother, physical neglect or abuse) who had not been sexually abused
(24). At follow-up, a group of women who were neither separated nor abused as girls was added as another comparison group. As adults, the women with histories of childhood sexual abuse had more depressive symptoms than both comparison groups.
Two studies used groups composed totally, or in part, of psychiatric inpatients. Bryer et al.
(25) reviewed consecutively admitted female psychiatric inpatients with a variety of psychiatric diagnoses and found that women with a reported history of abuse (sexual or physical) before age 16 years had significantly more depressive symptoms than did those who did not report abuse. Since over half of those who reported childhood sexual abuse before age 16 years also reported subsequent sexual abuse as adults, revictimization may have played a role in these findings. Vize and Cooper
(26)) examined the rates of childhood sexual abuse in female inpatients and outpatients with diagnoses of major depressive disorder, anorexia nervosa, and bulimia nervosa compared with normal subjects. They found that there was a significantly greater rate of childhood sexual abuse in the clinical groups than in the comparison groups but no difference in rates between the three clinical groups.
Two studies examined childhood sexual abuse in women seeking outpatient treatment. In the first study, a group of women with a history of sexual abuse before age 14 years scored significantly higher on the Beck Depression Inventory than did patients who had not been abused
(27). The second study focused specifically on the effects of incest occurring before age 14 years
(28). It found that the lifetime incidence of major depression was significantly higher in women who had been victims of incest than in female patients who had not been victims of incest (89% versus 57%).
Study groups of women drawn from general medical practices were used in the remaining four studies. A total of 131 consecutive women outpatients who gave a history of childhood incest, molestation, or rape described themselves as depressed more often than did nonabused comparison subjects (83% versus 32%)
(29). In a group of 100 women scheduled for diagnostic laparoscopy, the risk for lifetime diagnosis of major depression was higher for those who gave a history of severe sexual abuse (incest, rape, oral contact, or repeated fondling) than for those with less severe abuse (exhibitionism or aborted attempts) or no abuse (86% versus 36%)
(30). A series of patients from four community-based primary care practices composed the largest clinical study group examined (N=1,931)
(31). Despite the use of a single screening question to define a history of childhood sexual abuse, those subjects with childhood sexual abuse demonstrated a significantly higher mean score on the depression subscale of the Hopkins Symptom Checklist-90 than did those without childhood sexual abuse. A rigorous screening method was utilized to identify depressed subjects and to define the history of childhood sexual abuse in another large study group drawn from a general medical practice (N=1,189)
(32). These investigators considered the history of childhood sexual abuse in women who were depressed versus those who were not depressed and discovered that whereas 37% of the depressed women reported childhood sexual abuse, only 23% of the nondepressed comparison subjects reported childhood sexual abuse.
RELATIONSHIP OF CHILDHOOD SEXUAL ABUSE TO ADULT-ONSET DEPRESSION IN MEN COMPARED WITH WOMEN
A review of the literature identified three studies that provide data on the relationship between childhood abuse and adult-onset depression in men versus women. Only two of these focused specifically on the impact of childhood sexual abuse on adult-onset depression
(33,
34), whereas the third defined past abuse as sexual or physical
(35).
All three studies found a strong positive correlation between reported childhood abuse and adult-onset depression when the data were analyzed without regard to gender. When the data for each gender were examined independently, one study found no difference in the strength of this relationship between women and men, but 168 women were compared to only 20 men
(33). However, results from two studies raised the possibility that this relationship may be greater for women than for men
(34,
35). The first of these studies
(35) found that female subjects with a history of childhood abuse were more than twice as likely to have depressive symptoms as males with childhood abuse histories (69% versus 27%). The second study, by Stein and colleagues (34), which reanalyzed data from a community study of 3,132 adults
(11), excluded those subjects whose first incident of sexual abuse occurred after the age of 16 years. In this study, female victims had a significantly higher lifetime prevalence and current incidence rates of major depressive disorder when compared with female nonvictims, whereas male victims failed to demonstrate significantly higher rates of major depressive disorder when compared with male nonvictims
(34).
CHARACTERISTICS OF CHILDHOOD SEXUAL ABUSE AND SUBSEQUENT ADULT-ONSET DEPRESSION
The relationship between a number of characteristics of childhood sexual abuse and its psychological sequelae have been examined in order to establish which aspects of abuse are most deleterious. The data strongly suggest that greater severity, frequency, and duration of abuse results in an increased likelihood of subsequently developing depression
(15,
19,
21,
36). For example, Bifulco et al.
(12) found the incidence of depression to be 100% in women who suffered forced intercourse, 78% in those with repeated abuse not involving intercourse, and 30% in those with a single episode of abuse not involving intercourse.
While there have been mixed findings regarding the impact of the age at which childhood sexual abuse takes place on the subsequent development of adult-onset depression, the majority of studies have failed to demonstrate a clear relationship
(12,
15,
19,
21,
37). Similarly conflicting findings have also emerged regarding the effect of the relationship between the victim and the perpetrator
(14,
21,
23,
38). While no consistent pattern has been observed for abuse by a relative versus a nonrelative, a stranger versus an acquaintance, or incest versus nonincest, it has been suggested that father-daughter incest may be more damaging than other sorts of abuse
(38,
39).
FACTORS MEDIATING THE RELATIONSHIP BETWEEN CHILDHOOD SEXUAL ABUSE AND MAJOR DEPRESSIVE DISORDER
The evidence just presented suggests that childhood sexual abuse in girls is a risk factor for adult-onset depression in women. We now consider the mechanisms, both psychosocial and neurobiological, by which such early traumatic experiences may result in psychiatric disorders in adulthood.
Psychosocial Factors
It has been suggested that there may be a direct causal relationship between childhood sexual abuse and adult-onset depression. However, it is also possible that other variables, such as poor parenting, may increase the likelihood of both childhood sexual abuse and adult-onset depression. There is a large collection of literature offering theoretical explanations for the connection between childhood sexual abuse and depression
(39,
40), but few of these theories are based on empirical data. Areas in which empirical studies have been performed include the effects of parenting, cognitive style, and lifestyle on the long-term consequences of childhood sexual abuse.
Parenting
It has been suggested that poor parenting may either independently increase the risk of both childhood sexual abuse and adult-onset depression or that it may act to increase the likelihood of subsequent depression in children who have been abused
(24).
Eight studies have examined the relationship between family dysfunction, childhood sexual abuse, and adult-onset depression
(12,
15,
17,
18,
20,
22,
23,
41). Of these, four found a positive correlation between childhood sexual abuse and various markers of familial dysfunction, including early parental separation, family violence, physical punishment, and lack of parental warmth
(12,
17,
20,
22). Indeed, evidence suggests a positive correlation between poor parenting and adult-onset depression, even in the absence of childhood sexual abuse
(12,
18,
22,
23), and one study found that poor parental support was a better predictor of subsequent impaired psychological functioning than childhood sexual abuse
(23) However, in the four studies in which the variables related to family dysfunction or poor parenting were controlled, the relationship between childhood sexual abuse and adult-onset depression was maintained
(12,
15,
17,
41). When considering all eight studies together, the weight of evidence suggests that there is a relationship between childhood sexual abuse and adult-onset depression in women, even when controlling for poor parenting as a risk factor for later depression.
Cognition
Gold has pointed out that studies directed at understanding the long-term effects of childhood sexual abuse tend to consider variables surrounding the abuse event and do not address ways in which the cognitive characteristics of the victim, or the victim-environment interaction, might predict outcome
(20). Gold stated the hypothesis that a person’s “causal attributions and expectancies” are critical in his or her response to the environment and, therefore, in how he or she is affected by a stressful event such as sexual abuse during childhood. Empirical work by Gold showed that attributional style (measured in terms of internal-external, stable-unstable, and global-specific attributions) was related to adult functioning. Specifically, those women who had been sexually abused as children and also had high scores on psychological distress scales (such as the Beck Depression Inventory) tended to have internal, stable, and global attributional styles when confronted with adverse events. However, it is not clear whether these attributional styles preceded the abusive event or resulted from it. These findings generate further questions about the role of predisposing cognitive factors and reflect the difficulty in determining the long-term effects of early abuse by means of retrospective investigation, with all of its associated methodological difficulties (such as recall bias and the problem of distinguishing cause and effect).
Lifestyle
A number of studies have found that women with histories of childhood sexual abuse lead more disadvantaged lives in general, with a greater incidence of teenage marriage, divorce or separation, lower socioeconomic status, and higher rates of various other life stressors than women without abuse histories
(12,
14,
17). Although data are not available to show the role of these psychosocial variables in the childhood sexual abuse-adult depression relationship, one might postulate that these life circumstances are mediating factors between childhood sexual abuse and adult-onset depression.
Neurobiological Factors
Neurobiological hypotheses regarding the relationship between childhood stressors and adult-onset depression have generally focused on the HPA axis. Particular emphasis has been placed on the increased levels of corticotropin-releasing hormone (CRH), adrenocorticotropic hormone (ACTH), and corticosteroids seen both following early stress and in patients with depression.
A number of investigators have demonstrated that early stressors may result in both acute and chronic changes in the activity and regulation of the HPA axis, chiefly in the form of hypersecretion of CRH. This has led to the hypothesis that such CRH hypersecretion may create a biological vulnerability to the subsequent development of depression, either directly or by means of an increased sensitivity to stressors in adulthood
(42–
50).
There are two main lines of evidence supporting this hypothesis. First, the HPA axis is known to be hyperactive in depression, with higher production and secretion of CRH. Second, data from animal and human studies suggest that early stress produces both acute HPA hyperactivity (by means of increases in CRH) and long-term changes in HPA activity, resulting in a differential response to stressors in adulthood. Thus, both the effects of stress and the pathophysiology of depression are associated with similar changes in HPA axis activity.
In addition to providing a possible explanation for the association of stress and depression, both the magnitude and the nature of the stress-induced changes in the HPA axis may differ between the sexes. The mechanism of these differences may be particularly important in understanding the disparity between the genders in both the response to stress and the prevalence of depression. Of special relevance to this review is the increased frequency and impact of one particular early stressor in females—childhood sexual abuse—and how HPA axis dysregulation induced by childhood sexual abuse might provide a biological basis for vulnerability to adult-onset depression in women.
HPA AXIS IN DEPRESSION
Major depressive disorder is associated with hyperactivity of the HPA axis
(51). Abnormalities documented in patients with depression include an elevation in urinary free cortisol and basal plasma cortisol and failure to suppress endogenous cortisol secretion in response to dexamethasone administration. In addition, it is likely that there is centrally mediated hypersecretion of CRH in subjects with major depressive disorder. This is reflected in a blunted ACTH response to stimulation with exogenous CRH
(51,
52). Further evidence in support of hypersecretion of hypothalamic CRH in patients with major depression includes the findings that increased concentrations of CRH are found in the CSF of depressed subjects
(53,
54), that healthy subjects given infusions of CRH display a similar pattern of cortisol hypersecretion to that seen in depressed subjects
(51), and that there is a decreased density of CRH-binding sites in the frontal cortex of suicide victims
(55). In addition, glucocorticoids stimulate serotonin breakdown, hippocampal serotonergic projections reduce hypothalamic CRH secretion, and compounds with proserotonergic effects (such as selective serotonin reuptake inhibitors and
l-tryptophan) have antidepressant activity
(56).
Effects of Stress on the HPA Axis
There is considerable experimental evidence that the physiologic response to stress is largely mediated by an increase in CRH production and secretion, resulting in an increased release of ACTH and cortisol
(57). These increases are usually transient, but certain acute stressors, when acting on the subject during particular periods in early life, appear to cause chronic hypersecretion of CRH and ACTH, with accompanying adrenal and pituitary hypertrophy. This chronic hyperactivity of the HPA axis following early stress is likely to be mediated, at least in part, by changes in gene expression, as demonstrated by higher CRH mRNA levels in the paraventricular nucleus neurons
(58).
It has been theorized that early stress, such as maternal deprivation or childhood sexual abuse, may produce a biological vulnerability to depression that can become manifest in response to adult stress
(42,
44). Although few studies address this issue directly, both animal and human data may be helpful in clarifying the neurobiological relationship between early stress and adult-onset depression.
Animal studies
Animal studies have been important in delineating the neuroendocrine response to stress, and some lend support to the notion that the stress response is associated with hypersecretion of CRH
(59–
61). Although most animal studies have focused on responses to stress in rats at a single point in time, several studies have shown chronic changes in the HPA axis in response to the early stress of mother-infant separation
(44,
62–
64). Of particular relevance are the following three studies that examined the response of the HPA axis to stress in adults who had been exposed to stress as infants.
A group of adult, nonhuman primates exposed to early stress (rearing by mothers exposed to environmental unpredictability) were found to have elevated concentrations of CRH in their CSF when compared to a group not exposed to early stress
(65). These findings suggest long-term hyperactivity of the HPA axis following early stress that persists into adulthood.
Ladd and colleagues hypothesized that early stress could affect CRH neurons in a manner that would neurochemically predispose animals to a particular stress response in adulthood
(44). Accordingly, they administered a foot shock to two groups of adult rats—those that had been maternally deprived as pups and those that had not. When the neurochemical responses of these two groups were compared, adult rats that had been maternally deprived had higher basal ACTH concentrations, a greater ACTH response to stress, fewer CRH binding sites in the anterior pituitary, more CRH binding sites in the rapine nucleus, and higher CRH concentrations in the parabrachial nucleus and the median eminence. Similarly, Plotsky and Meaney
(66) found elevations in baseline hypothalamic CRH mRNA in adult male rats that had experienced early maternal separation when compared with adult rats that had not. In response to restraint stress, adult rats that had been maternally separated had higher plasma cortisol responses than did comparison animals. These animal data suggest that there are long-term effects of early stress on the neurophysiological status of the HPA axis in male rats and nonhuman primates and that these effects may produce hypersecretion of CRH in response to stress in adulthood. Furthermore, the lasting neurochemical changes seen following early stress appear to be similar to those found in patients with depression.
Human studies
In a study of men and women who had experienced parental loss before age 17 years, Briere et al.
(67) assessed the quality of the subjects’ home lives following their loss and their adult psychiatric status; measured their resting levels of plasma cortisol, β-endorphin, and ACTH; and performed dexamethasone suppression tests. Those individuals with adult psychopathology had significantly higher levels of plasma cortisol and β-endorphin than did subjects without psychopathology; these plasma levels were inversely correlated with the quality of childhood home life following parental loss. Another group found significantly lower basal and CRH-stimulated ACTH levels in a group of girls aged 7–15 years who had been sexually abused when compared with matched comparison girls who had not
(68). The subjects were not depressed at the time of the study, and a mean of 4.7 years had elapsed following the abuse. While there were no group differences in free cortisol levels or CRH cortisol stimulation, it was notable that the decreased ACTH response to CRH stimulation in these girls was similar to the blunted ACTH response to CRH previously demonstrated in adult depressed subjects. In contrast, Kaufman et al.
(69) compared depressed prepubertal children with a history of abuse to depressed, nonabused children and normal comparison subjects and found a significantly greater ACTH response to exogenous CRH in those subjects with a history of abuse.
These six studies
(44,
65–
69) offer preliminary evidence that early stress results in long-term changes in HPA axis function and regulation similar to those believed to be important in the pathophysiology of depression. These similarities lend support to the hypothesis that a significant adverse event during childhood may contribute to depressive illness during adulthood by means of chronic dysregulation of the HPA axis.
Sex Differences in HPA Axis Response to Stress
Considerable human and animal data suggest that the HPA axis is more reactive to stress in females than in males
(70–
74). These studies examine the effects of sex on the response of the HPA axis to a wide variety of stressors. The study most relevant to this review is that of McCormick et al.
(75), who found that female rats exposed to prenatal stress developed greater ACTH and corticosteroid levels in response to restraint as adults, whereas similarly exposed male rats did not.
In considering what might account for the sex differences in the HPA axis response to stress, some groups have examined the possible role of gonadal steroids. It has been demonstrated that castration results in an increase in the adrenal response to stress in adult male rats and hamsters, and estrogen administration in both sexes causes an increase in basal cortisol secretion, accompanied by a greater ACTH and cortisol response to stress
(70,
71). Following exposure to exogenous glucocorticoids, male rats have a diminished ACTH response to restraint stress, whereas, by contrast, intact female rats maintain an ACTH response similar to that before glucocorticoid exposure; ovariectomized female rats show an intermediate ACTH response
(76). Finally, a direct effect of estrogen on parvocellular hypothalamic CRH cells has been suggested by the localization of estrogen receptor mRNA within these cells
(71), and evidence has been found for an estrogen-responsive portion of the promoter region of the CRH gene
(77). Thus, these studies suggest that neurochemical changes occurring as a result of childhood stress may be long lasting, may appear to differ between women and men, and may create a greater biological vulnerability to depression in women.
DISCUSSION
There is considerable evidence that childhood sexual abuse has long-term effects. Studies of community, college, and clinical groups of women demonstrate a clear relationship between childhood sexual abuse and adult-onset depression, and this relationship appears to persist even when controlling for other variables that may be independently associated with adult-onset depression. In addition, there is a positive correlation between the severity of sexual abuse in childhood and the incidence of subsequent adult-onset depression. Studies including both men and women have shown less consistent results, but some evidence suggests that women with histories of childhood sexual abuse may be more likely to suffer from depression in adulthood than men who have been victims of childhood sexual abuse.
A small but growing body of evidence from both animal and human studies suggests that a neurobiological mechanism may explain the link between the trauma of childhood sexual abuse and adult-onset depression. The pathophysiological similarities observed in both the stress response and depressive illness, together with the evidence linking the clinical experience of stress and depression, suggest a neurophysiological relationship between the two. Of particular interest here is the chronic dysregulation of the HPA axis sometimes induced by early stress, as well as the apparent sexual dimorphism in the HPA axis response to stress. Such dimorphism may produce sex differences in the neurobiological response to stress and perhaps, therefore, in the incidence of depression.
We suggest that gonadal steroids have some role in the modulation of the HPA axis and thus may be important in the higher sensitivity of the HPA axis to stress in females. In apparent contrast, other work has shown that the use of estrogen as augmentation to serotonin-promoting drugs results in a therapeutic effect on mood symptoms
(78). These two findings may not be incompatible, since gonadal steroids may play a role in early sensitization to extreme stress and thereby increase the possibility of a stress-induced mood syndrome. At the same time, estrogen may be important in the regulation of mood by means of other mechanisms outside the stress-related pathways. In addition, recent preclinical evidence suggests that stress can elevate gonadal steroids and estrogen, which may be protective when it occurs in moderation but lead to dysfunction when exaggerated
(79). Moreover, it is clear that the etiology and pathophysiology of depression are complex, and there exist a number of critical factors beyond the scope of this article. Those most relevant here include the neuroendocrinologic interactions between estrogen and serotonin
(80), cultural responses (which may lead victimized women toward depression and victimized men toward alcoholism)
(81), and hereditary factors
(7) (some of which have been hypothesized to be associated with abnormalities in the serotonin system passed from abusive alcoholic fathers to their daughters who develop depression
[82]).
While the focus of this review is on the relationship of childhood sexual abuse to adult-onset depression, some studies report on the impact of childhood sexual abuse with regard to the subsequent development of other psychiatric conditions. For example, there is evidence that a number of psychiatric disorders may be higher in populations of women who have been sexually abused in childhood
(25). Bulimia nervosa
(13), panic disorder with agoraphobia (83), generalized anxiety disorder
(84), somatization disorder
(84), and borderline personality disorder
(85) have each been found not only to be associated with childhood sexual abuse but to be more prevalent in women than in men (DSM-IV). Although Wexler et al.
(86) found a specific association between childhood abuse and adult-onset depression as compared with other disorders, it is important to recognize that while depression may be the most common negative long-term effect of early sexual abuse, it is not the only possible negative outcome.
Additionally, it is possible that other severe early traumas may increase the risk for adult-onset depression or other psychiatric syndromes. We have focused on childhood sexual abuse in this review since it is the form of childhood trauma that has been investigated far more than any other. Other types of childhood trauma examined include parental loss
(67), poor parenting
(87), parental drinking, family violence, and parental mental illness
(88).
The studies reviewed here only begin to shed light on questions about why some abused girls and not others develop a depressive illness later in life. Investigations have begun to consider the type of sexual abuse encountered, the environmental factors that accompany abuse (such as parenting), and attributional styles. However, these variables need further study, as do predictors of depression that may have existed before the abuse, such as genetic loading and temperament. In addition, particular attention to self-concept, core beliefs, and coping style would be useful, as recent literature suggests that these may play a role in mediating the onset of adult disorders after exposure to early adversity
(89,
90). It is possible that there are victims who were already more vulnerable to injury or less able to adapt in the face of an early trauma. Further research needs to be conducted to understand the nature of this relationship. Such research should include studies of the mediating factors between childhood sexual abuse and adult-onset depression and, in particular, the effects of sex on stress-induced dysregulation of the HPA axis.