We studied individuals with schizophrenia who had and had not attempted suicide. The goals of this study were 1) to characterize a study group of individuals with schizophrenia and schizoaffective disorder who had attempted suicide and 2) to compare individuals with schizophrenia who had and had not attempted suicide with respect to demographic and clinical variables.
RESULTS
Thirty-three percent (N=52) of this study group reported at least one suicide attempt; 60% (N=31) of those who had attempted suicide reported multiple attempts. The rates of attempts for those with schizophrenia and those with schizoaffective disorder were not significantly different (39%, N=17, versus 31%, N=35) (χ2=0.77, df=1, p=0.38). There also was no significant difference between those who had and had not attempted suicide with regard to the rate of schizoaffective disorder (33%, N=17, versus 26%, N=27) (χ2=0.78, df=1, p=0.38). Therefore, individuals with schizophrenia and schizoaffective disorder were combined.
Fifty-two percent (N=27) of those who had attempted suicide made attempts of moderate to extreme lethality, and 36 (76% of the 47 patients for whom these data were available) reported strong suicidal intent. For the most severe attempts, suicidal behavior included overdosing (42%), slitting one’s wrists (16%), jumping (8%), hanging (6%), and other methods (i.e., running into highway traffic or stabbing oneself) (18%). Fifty-seven percent of those who had attempted suicide were admitted to inpatient medical units, and 11% were treated in emergency rooms after their attempts.
The 88 reasons given for the attempts included depression (N=28), loss of a significant other (i.e., spouse, boyfriend/girlfriend) (N=14), being bothered by psychotic symptoms (N=11), response to a stressful life event (N=10), response to command auditory hallucinations (N=4), “to escape” (N=4), because he or she was being physically abused (N=3), substance abuse (N=2), for attention (N=2), and for unknown reasons (N=10).
Given the large number of comparisons conducted, the Bonferroni correction was calculated for the six demographic comparisons, and the significance level was set at p<0.008. Those who had and had not attempted suicide were comparable with respect to age (had attempted suicide: mean=37.17 years, SD=10.41; had not: mean=37.82 years, SD=12.54) (t=0.04, df=120, p=0.73); sex (62% were men versus 58% were men) (χ2=0.21, df=1, p=0.64); race (50% Caucasian, 21% African American, 17% Latino, 12% other versus 39% Caucasian, 27% African American, 22% Latino, 12% other) (χ2=2.60, df=3, p=0.46); education (mean=12.06 years, SD=2.96, versus mean=12.5 years, SD=2.77) (t=0.88, df=109, p=0.37); marital status (never married: 73% versus 72%) (χ2=1.13, df=4, p=0.89), or living arrangement (live with family/friends: 63% versus 61%) (χ2=6.34, df=7, p=0.50).
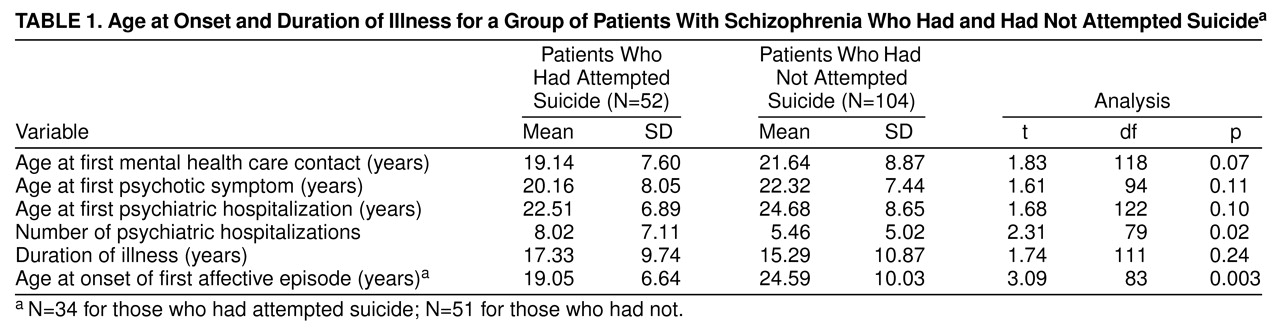
The Bonferroni correction was used for the 14 analyses assessing clinical characteristics, and the significance level for these analyses was set at p<0.004 (
Table 1). The groups were comparable with respect to age at onset of psychosis, duration of illness, age at first mental health care contact, age at first psychiatric hospitalization, and number of psychiatric hospitalizations.
More than 80% (N=43) of those who had attempted suicide reported that their first attempt occurred after the onset of psychosis (mean=3.86 years after onset, SD=8.01) (paired t=3.41, df=49, p=0.001) and after their first hospitalization (mean=4.57 years after first hospitalization, SD=8.62) (paired t=3.68, df=46, p=0.001).
The groups did not differ with respect to history of 1 week of significant depressed mood (had attempted suicide: 60%, N=31; had not: 55%, N=57) (χ2=0.33, df=1, p=0.56) or history of a major depressive episode (58%, N=30, versus 43%, N=45) (χ2=2.89, df=1, p=0.09). Suicidal ideation during depression occurred twice as often for those who had attempted suicide (80%, N=24) as for those who had not (42%, N=19) (χ2=9.93, df=1, p=0.002), and 57% (N=17) of those who had attempted suicide who had a history of depression reported having made a suicide attempt during a major depressive episode. Those who had attempted suicide reported that their first affective episode occurred significantly earlier than that of those who had not. The groups were comparable with respect to history of a manic episode (27%, N=14, versus 23%, N=24) (χ2=0.09, df=1, p=0.77). The groups did not differ with respect to history of alcohol abuse/dependence (31%, N=16, versus 21%, N=22) (χ2=1.24, df=1, p=0.27) or drug abuse/dependence (27%, N=14, versus 24%, N=25) (χ2=0.34, df=1, p=0.56).
DISCUSSION
The rate of suicide attempts in this group of individuals with schizophrenia and schizoaffective disorder was high and comparable to that found in other studies
(1–
3). In contrast to groups without schizophrenia, the suicide attempts were serious, typically requiring medical attention. Intent was strong, and the majority of those who had attempted suicide made multiple attempts. Compared with other groups, the rate of suicide attempts by overdose was relatively low (only 42%, N=22), and the rate of more lethal methods was higher. Consistent with other research, those with schizophrenia who had and had not attempted suicide did not differ with respect to demographic characteristics
(1–
3).
This is the first study to document reasons for having made a suicide attempt among individuals with schizophrenia. The most frequent reason was that the person was depressed. We do not know how many individuals in this group actually met the criteria for major depression at the time of the attempt. The next most frequent reason was the loss of a spouse or boyfriend/girlfriend. While most individuals in this study group were not married, they had been involved in romantic relationships. These types of relationships have not been fully considered in previously published reports. As documented by others
(1–
3), the rate of suicide attempts in response to command hallucinations was low, although 11 attempts were made because the presence of psychotic symptoms was bothersome. This stresses the importance of treating psychosis and monitoring symptoms throughout the course of illness. Few patients reported that they had made a suicide attempt because of problems with substance abuse. Ten attempts were made in response to stressful life events, emphasizing the importance of attending to psychosocial functioning.
More than 80% (N=43) of first suicide attempts occurred after the onset of psychosis and within the first 5 years of illness, suggesting that the risk for suicidal behavior is higher after the onset of schizophrenia. Since the suicidal behavior did not occur at the actual time of onset of psychosis or at the time of the first mental health care contact, it is unlikely that suicidal behavior was the reason for the first mental health care contact.
No clinical syndromes differentiated the patients who had from those who had not attempted suicide; thus, their mere presence is not predictive. The findings are consistent with, but not necessarily predictive of, a stress-diathesis model such that clinical syndromes may trigger suicidal behavior in those already at risk. For example, while a history of depression did not differentiate the groups, depression increased the risk for suicidal behavior for those who had attempted suicide. The earlier onset of affective illness in those who had attempted suicide also highlights the importance of early recognition and treatment of affective illness in schizophrenia.
Lifetime psychopathology and suicidal behavior were assessed by using a standardized interview. While the study group size is relatively large, it is not large enough to adequately detect group differences when subgroups of individuals are considered or to apply sophisticated multivariate analyses. A strength of the study group is that individuals were not necessarily in an acute state of illness when they participated, providing a more community-based, more representative study group. However, all participants had to agree to participate in the research, thereby limiting the generalizability of the results. Finally, suicidal behavior was remote relative to the time of the assessment, so that this study does not examine the relationship between suicidal behavior and specific risk factors more proximal to a suicide attempt.
This study supports the need for prospective evaluation of suicidal behavior and its associated risk factors; it also supports the need for ongoing biopsychosocial assessments and interventions targeting psychotic and depressive symptoms with pharmacological agents and psychosocial interventions.