Social cognition is a specialized domain of cognition hypothesized to have developed in order to solve social and adaptive problems. The capacity for understanding another’s mental state may have evolved from the ability to experience our own mental states
(1) . In healthy subjects, the neural bases of various aspects of social cognition have been explored, including the “theory of mind,” empathy, moral/ethical judgments, and social cooperation
(2,
3) . In parallel, there is an increasing interest in social cognition in schizophrenia
(4) because difficulties with social cognition might directly contribute to impaired social functioning in these patients.
There have been only a few neuroimaging studies examining the neural basis of social cognition in people with schizophrenia. Russell and colleagues
(7) reported left middle and inferior frontal cortex underactivation in people with schizophrenia during mental state attribution. Using an intention attribution task, Brunet and colleagues
(8) showed right medial prefrontal cortex underactivation in people with schizophrenia. These findings raise the question as to whether deficient activation during social cognition can “recover” with clinical improvement. In support of this suggestion, patients with schizophrenia showed a return of task-related brain activation similar to that of healthy subjects following verbal memory training
(9) and treatment with typical
(10) and atypical antipsychotic medication
(11) . There is also some evidence that social cognition improves in parallel with clinical improvement in schizophrenia
(12) .
Hence, we hypothesized that, on a social cognition fMRI paradigm, 1) the medial prefrontal cortex of patients with schizophrenia is underactivated during an acute episode in relation to healthy comparison subjects and their own activation levels after recovery from an acute episode and that 2) the improvement in medial prefrontal activation is associated with enhanced illness insight and social functioning. To test these hypotheses, we scanned 14 patients during an acute episode of their illness and again following clinical improvement. Fourteen healthy comparison subjects were also scanned twice, with approximately the same time interval between scans as in the patient group, to control for the effects of time, scan repetition, and paradigm exposure. In view of the suggested association between Wisconsin Card Sorting performance and social functioning
(13), we also examined the relationship between Wisconsin Card Sorting Test performance and brain activation changes.
Discussion
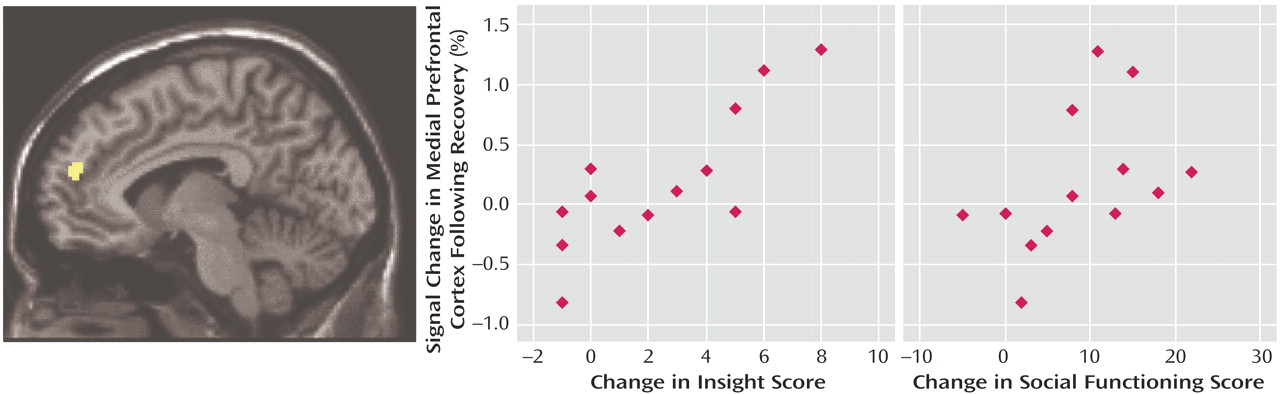
This study employed a repeated-measures design to investigate the neural basis of social cognition during and after an acute episode in patients with schizophrenia. Symptom ratings, social functioning, illness insight scales, and the Wisconsin Card Sorting Test were used to examine whether improvement on these measures was predicted by recovery of brain activation in response to the social cognition paradigm. Our study showed that patients with schizophrenia displayed less activation than healthy subjects in the left medial prefrontal cortex, among other regions. However, clinical improvement after treatment was accompanied by enhanced activation in this region. The increase in left medial prefrontal cortex activity was specifically associated with improved insight and social functioning (just less than significant) scores in these patients. This increased activation may have provided a partial explanation for the neural basis of improved social cognition after recovery observed in other studies
(12) . We also found that reduced severity of negative symptoms was associated with enhanced activation in the left ventral anterior cingulate cortex.
The finding that the medial prefrontal cortex was activated in our social cognition paradigm in comparison subjects is in line with many other neuroimaging studies of the neural basis of understanding the mental states of others
(5) . The medial prefrontal cortex is activated when attention is directed to the self (self-awareness)
(23) . The common engagement of this area for representing the mental states of others and the self may provide the neural basis for intersubjectivity
(24), the interplay between two different subjective minds. Considering this common engagement, it is important to highlight that the increased activation in the left medial prefrontal cortex was associated with improved “illness insight” in people with schizophrenia. The specific association between improved illness insight and medial prefrontal activation in our repeated scans is strengthened because patients with schizophrenia in general have greater variability in brain activation across time in relation to healthy comparison subjects
(25) .
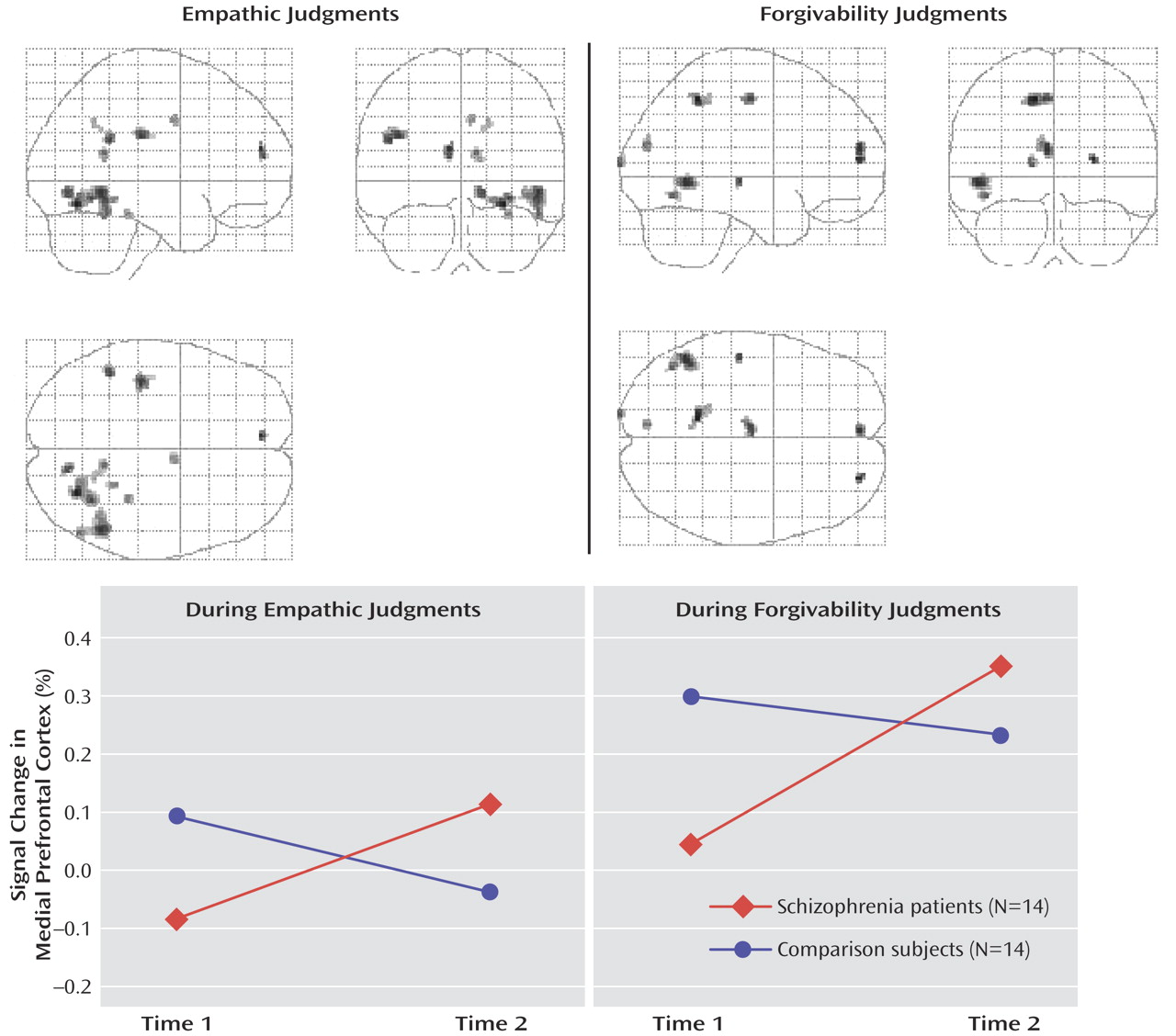
In this study, in both comparison and schizophrenia subjects, activation generally decreased over time. In the left medial prefrontal cortex, however, we found that activation change over time in patients was in the opposite direction of that of comparison subjects. Patients showed increased activation at the second scan, whereas the comparison group showed decreased activation at the second scan (
Figure 1 ). Thus, at the second scan, there were no significant group differences in activation in the left medial prefrontal cortex. Other studies have reported similar task-related brain activation “recovery” in patients with schizophrenia. Wexler and colleagues
(9) showed that increased activation in the left inferior frontal cortex was significantly correlated with patients’ behavioral improvement in verbal memory performance following verbal memory training for 10 weeks. On the other hand, studies of healthy volunteers have reported that task-relevant activation may be reduced when they are presented with familiar stimuli or when a task has been previously rehearsed
(26) . Increased efficiency or reduced anxiety to task in healthy subjects may explain the reduced activation over time.
To date, we are aware of two neuroimaging studies of social cognition in patients with schizophrenia. Russell and colleagues
(7) reported that people with schizophrenia made more errors in the mental state attribution of photographed eyes, and had less activation in the left prefrontal cortex in relation to comparison subjects. A positron emission tomography study by Brunet and colleagues
(8) used a sequencing task that involved having to infer a character’s intention and choosing a card to complete sequences. In this task, in contrast to the finding of Russell et al., people with schizophrenia showed decreased activation in the right medial prefrontal cortex. We speculate that language material used in our study (written scenarios and response options) and Russell and colleagues’ (matching words with photographs) might engage the left prefrontal cortex more than the right. The nonverbal material used in the study by Brunet and colleagues might explain why they showed right prefrontal activation. Our study showed that areas exhibiting enhanced activation in patients after recovery (left medial prefrontal cortex, Brodmann’s area 9/10) were not identical to those that were deficient in activation at the first scan (Brodmann’s area 8/9). It is possible that these various prefrontal areas are part of one functionally defined area of the cortex because these areas are frequently reported in social cognition studies
(5) . Alternatively, patients may have recruited different prefrontal areas to perform the task when they were acutely ill.
The other brain area that schizophrenia patients consistently failed to activate for both empathic and forgivability judgments at the first scan was the right posterior fusiform gyrus. Schultz and colleagues
(27) showed that the right posterior fusiform gyrus, which has been associated with face perception, is activated in response to a task involving perception of moving geometric shapes interacting with each other in a social manner. Another study by Geday and colleagues
(28) demonstrated that the right posterior fusiform gyrus was activated in response to emotional pictures of people in social situations as well as facial emotion expressions. These studies suggest that the posterior fusiform gyrus is heavily involved in processing emotionally important cues and attributes of other people. Because patients with schizophrenia consistently showed underactivation in this area during facial emotion recognition
(29), future studies might examine the link between facial emotion recognition and social cognition in schizophrenia.
Healthy comparison subjects showed increased activation in the thalamus during empathic and forgivability judgments compared with baseline social reasoning judgments, whereas patients failed to activate this region. A number of studies have shown functional and structural thalamic abnormalities in schizophrenia
(30) . Whether the reduced thalamic activation in patients in this study is directly related to social cognition dysfunction or is associated with a lack of attention and sensory information processing remains to be determined. Nonetheless, studies showing thalamus-anterior cingulate network activation in mothers listening to infant cries
(31) and involvement of this network in rodent maternal behavior
(32) suggest that this network activity might represent attention to emotional and social stimuli, consisting of a neural basis for social cognition.
Following recovery from the acute episode, the patient group showed increased activation in the left subgenual anterior cingulate cortex, which was associated with reduced negative symptoms. This area was not part of our hypothesis. Subgenual anterior cingulate cortex activity has been related to emotional responsivity and is reported to be decreased in people with depression
(33) . The current study, however, did not assess depressive symptoms or neuroleptic-induced movement disorders that partly overlap with negative symptoms. Statistical significance for this activity was weak, and the functional significance of increased subgenual anterior cingulate cortex activation in patients with schizophrenia could be addressed by future studies.
There are some issues to consider in interpreting the results of this study. In our study, the subjects were predominantly men. There is some evidence suggesting that women experience fewer adverse psychosocial consequences of schizophrenia
(34) . Second, we used a less conservative activation threshold in this study, which would increase the number of areas detected. We were, however, particularly interested in consistent findings across different comparisons. Finally, the need for the development of social cognition tasks for schizophrenia research should also be noted. The development of our fMRI tasks was based upon literature showing that an individual’s empathic responses arise as a direct result of observing someone in distress
(35) . Future studies might want to develop tasks to assess different aspects of social cognition in schizophrenia because social cognition is a wide domain of cognition and consists of multiple emotional and cognitive processes.
In summary, our study supports the hypothesis that improved insight following recovery from an acute episode of schizophrenia is reflected in enhanced medial prefrontal activation during social cognition tasks. The results of our study also suggest that medial prefrontal cortex underactivation in patients relative to healthy comparison subjects may reflect deficits in the representation of self and others and that these deficits may partially be ameliorated when patients can recruit the medial prefrontal cortex for social cognition. Our study highlights the biological responsivity of the prefrontal cortex to therapeutic intervention
(10,
36) and forms the basis upon which to investigate further neural mechanisms for psychosocial function in schizophrenia.