Although major depression is common, costly, and disabling and is one of the most burdensome disorders worldwide
(1 –
3), little is known about changes in its prevalence over time. Retrospective analyses of lifetime depression in one-time cross-sectional studies indicate that prevalence rates of depression in the United States have dramatically increased over the past 50 years
(4 –
6) . An earlier longitudinal study conducted in Sweden also found increasing rates of depression from the 1940s through the 1970s
(7), and recent cross-national studies of depression conducted largely in the 1980s generally support the finding of increasing prevalence of depression in more recent cohorts
(8), despite shorter periods of risk.
However, methodological concerns about the reliability of reporting of lifetime rates of depression have cast some doubt on the validity of these findings
(9 –
11) . Reported rates of depression among younger respondents might increase relative to rates among older respondents if studies systematically undercounted the disorder in older cohorts who have poorer recall of remote events. A differential recall bias of this sort appears to be supported by findings from a 40-year study of a community in Canada
(12) that found stable rates of depression over the course of repeated evaluations in 1952, 1970, and 1992.
Data from more recent surveys designed to assess trends in the prevalence of major depression over the past decade, using the same repeated cross-sectional design as our study, also can be considered. The prevalence of current major depressive episode was 10.1% in the 1990–1992 National Comorbidity Survey (NCS; 13) and 8.7% in the 2001–2002 National Comorbidity Survey Replication (NCS-R; 14). However, because the two surveys used different diagnostic criteria (DSM-III-R and DSM-IV, respectively) and because of extensive differences in how the surveys assessed major depression
(15,
16), the two studies’ prevalence rates are not comparable, and thus change over time cannot be reliably assessed. In addition, the baseline NCS rate was overestimated, for two major reasons. First, unlike DSM-IV, DSM-III-R did not include the clinical significance criterion for major depression requiring that distress or impairment be present for a diagnosis. When the clinical significance criterion was applied to the NCS baseline data, the prevalence of current depression was reduced from 10.1% to 6.4%
(17) . Second, the NCS baseline sample excluded persons over the age of 54, who have lower rates of current depression. Without this exclusion, the prevalence of current depression in the NCS baseline would be further reduced to 5.4%. Moreover, the NCS assessed youths 15–17 years of age, but the NCS-R did not. Excluding this youngest subgroup from the NCS would reduce the baseline rate yet again, but no data exist from which to estimate the magnitude of the reduction. Given these methodological problems, a conclusion based solely on the NCS and NCS-R prevalence rates that major depression has not increased much over the past decade
(17) is of limited value.
Understanding whether the prevalence of current major depression has recently increased in the United States is critical to etiologic research and health services planning. Addressing these questions with methods that overcome problems related to measurement and sample size is essential. Accordingly, the major objective of this study was to determine whether and how rates of major depression over the past decade have changed. We analyzed data from two large, nationally representative surveys of the adult U.S. population, both from the National Institute on Alcohol Abuse and Alcoholism: the National Longitudinal Alcohol Epidemiologic Survey (NLAES; 18), conducted in 1991–1992, and the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC; 1, 19), conducted in 2001–2002. Both surveys used the most current criteria for diagnosing major depression, assessed past-year major depressive episode, and applied consistent measures for diagnosing major depressive episode. The samples were large enough to examine for statistically stable prevalence estimates in the population as a whole as well as in important sociodemographic subgroups.
In view of the high rate of comorbidity between major depression and substance use disorders, we also sought to determine whether any changes observed in the rates of depression were associated with changes in rates of comorbid substance use disorders, a hypothesis tested in at least one previous study
(20) . We examined rates of major depressive episode for the total U.S. population and separately for those with and without current co-occurring substance use disorders. If rates of major depressive episode changed in the total sample but not among those without comorbid substance use disorders, it could be inferred that the changes in depression rates were associated with the changes in rates of comorbid substance use disorder. Likewise, if similar changes in depression rates were observed in the total sample and among those with and without comorbid substance use disorders, then other variables would have to be considered to account for changes in the rates of depression.
Method
Samples
The NLAES (N=42,862) and the NESARC (N=43,093) have been described in detail elsewhere
(1,
18,
19) . Both surveys used nationally representative samples of the adult population of the United States; the target population for each survey was civilians 18 years of age and older. Overall response rates were 90% for the NLAES and 81% for the NESARC. Oversampling of young adults and blacks in the NLAES and of young adults, blacks, and Hispanics in the NESARC increased the proportion of each of these groups in the total samples.
All potential NLAES and NESARC respondents were informed in writing about the nature of the survey, the statistical uses of the survey data, the voluntary aspect of their participation, and the federal laws that provide for the confidentiality of identifiable survey information. Respondents who gave consent were then interviewed. The research protocol, including informed consent procedures, was approved by the Census Bureau’s institutional review board and the U.S. Office of Management and Budget.
The complex sampling designs necessitated adjusting the data from both surveys to reflect oversampling of young adults and nonresponse at the household and person levels. The weighted data for both groups were then adjusted to be representative of the U.S. population according to current census data (1990 data for the NLAES and 2000 data for the NESARC).
Interviewers and Training
All interviews for both the NLAES and the NESARC were conducted by professional interviewers from the U.S. Bureau of the Census. On average, the interviewers (1,000 for the NLAES and 1,800 for the NESARC) had 5 years of health survey experience. All completed a 5-day self-study course followed by a 5-day in-person training session. To verify the quality of interviewing, 10% of all respondents were randomly selected to be recontacted by regional supervisors by telephone and were reasked a set of 30 questions from different parts of the interview to verify answers.
Diagnostic Assessment
All diagnoses in the NLAES and the NESARC were made on the basis of data from the Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV Version (AUDADIS-IV), a structured diagnostic interview designed for use by lay interviewers
(21) . The two surveys included the same core symptom questions to assess major depression, including the clinical significance criterion of DSM-IV. The NESARC used two additional distress items to assess the clinical significance criterion, but they were excluded from this analysis to enhance consistency between the two surveys. Excluding these items did not affect the rates of depression in the NESARC. In both studies, all questions were asked by highly trained interviewers; responses were recorded with pencil and paper in the NLAES and on laptop computers in the NESARC.
In this study, we examined current major depression, defined as meeting criteria for DSM-IV major depressive episode during the 12 months preceding the interview. Examining the rates of current major depressive episode rather than current major depressive disorder is more relevant to quantifying the burden on service delivery and associated economic costs. Assessing current major depressive episode is also most relevant in determining the magnitude of the disorder as it occurs and need for treatment regardless of whether individuals could be classified with lifetime unipolar major depressive disorder or bipolar illness. Consistent with DSM-IV, major depressive episodes due to a medical condition or bereavement were excluded. The NLAES and NESARC survey instruments used somewhat different methods to rule out substance-induced major depression, and the two could not be equated exactly. Thus, substance-induced cases were included, but given their extremely low prevalence (<0.01%
[1] ), their inclusion could not have affected the results reported here.
Symptom questions for DSM-IV substance abuse and dependence were asked separately for alcohol and each drug and aggregated into a composite measure of substance use disorders. Consistent with DSM-IV, a diagnosis of abuse required that the respondent report at least one of the four criteria for abuse within the 12 months prior to the interview, and a diagnosis of dependence required that at least three criteria from a list of seven be met.
As reported in detail elsewhere, the validity
(1,
22– 24) and test-retest reliability
(22,
25,
26) of AUDADIS-IV measures of major depression were rated as good (0.64–0.67), and a clinical reappraisal study of major depression diagnoses
(22) showed good agreement between AUDADIS-IV diagnoses and psychiatrists’ diagnoses (kappa=0.64–0.68). Test-retest reliability
(1,
22,
25– 28) (kappa>0.74) and validity as demonstrated in clinical reappraisal (kappa >0.70)
(29) and other validity procedures
(30 –
32) were good to excellent (kappa >0.64) for substance use disorders in studies conducted in the United States as well as in numerous countries in the World Health Organization/National Institutes of Health Joint Project on Reliability and Validity
(25,
28,
29,
33) .
Data Analysis
Prevalence estimates and standard errors, derived separately for the NLAES and the NESARC, were compared using t tests for independent samples in the total sample and among respondents with and without comorbid substance use disorders (
34, p. 89). All p values reported here are two-sided. Results are not reported when standard errors were too imprecise to be reliable. All standard errors were estimated using SUDAAN
(35), which accounts for the design characteristics of complex sample surveys.
Results
Past-Year Major Depression in the Total Samples
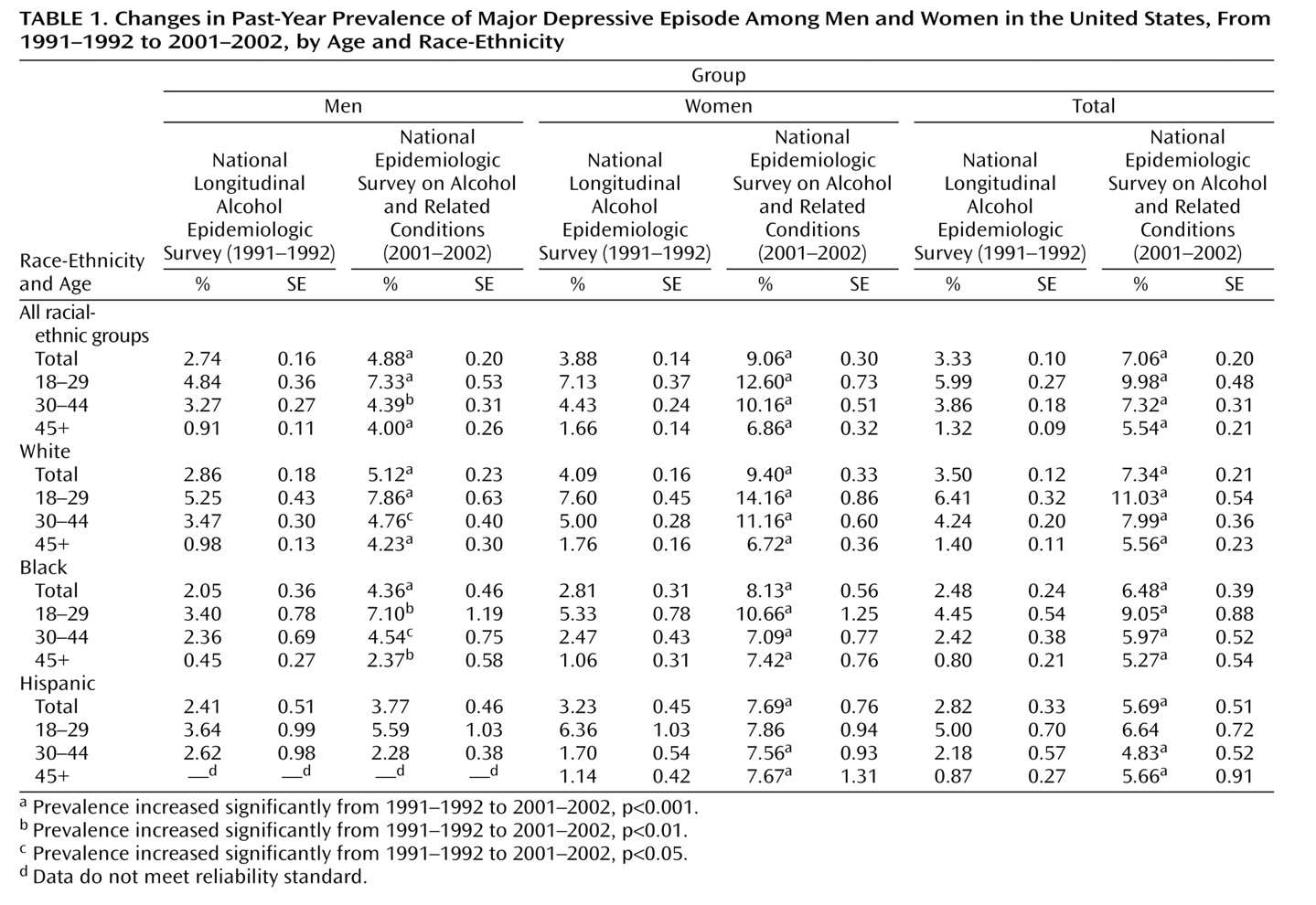
The prevalence of past-year major depressive episode in the total samples increased significantly from 3.33% in 1991–1992 to 7.06% in 2001–2002 (
Table 1 ). Furthermore, in nearly every age, racial-ethnic, and sex subgroup examined, significant increases in rates of depression were observed over the past decade. Although significant increases were observed for Hispanics overall in nearly all age groups, increases among Hispanic men and among 18-to-29-year-old Hispanic women were not statistically significant.
Past-Year Major Depression Among Persons With a Current Substance Use Disorder
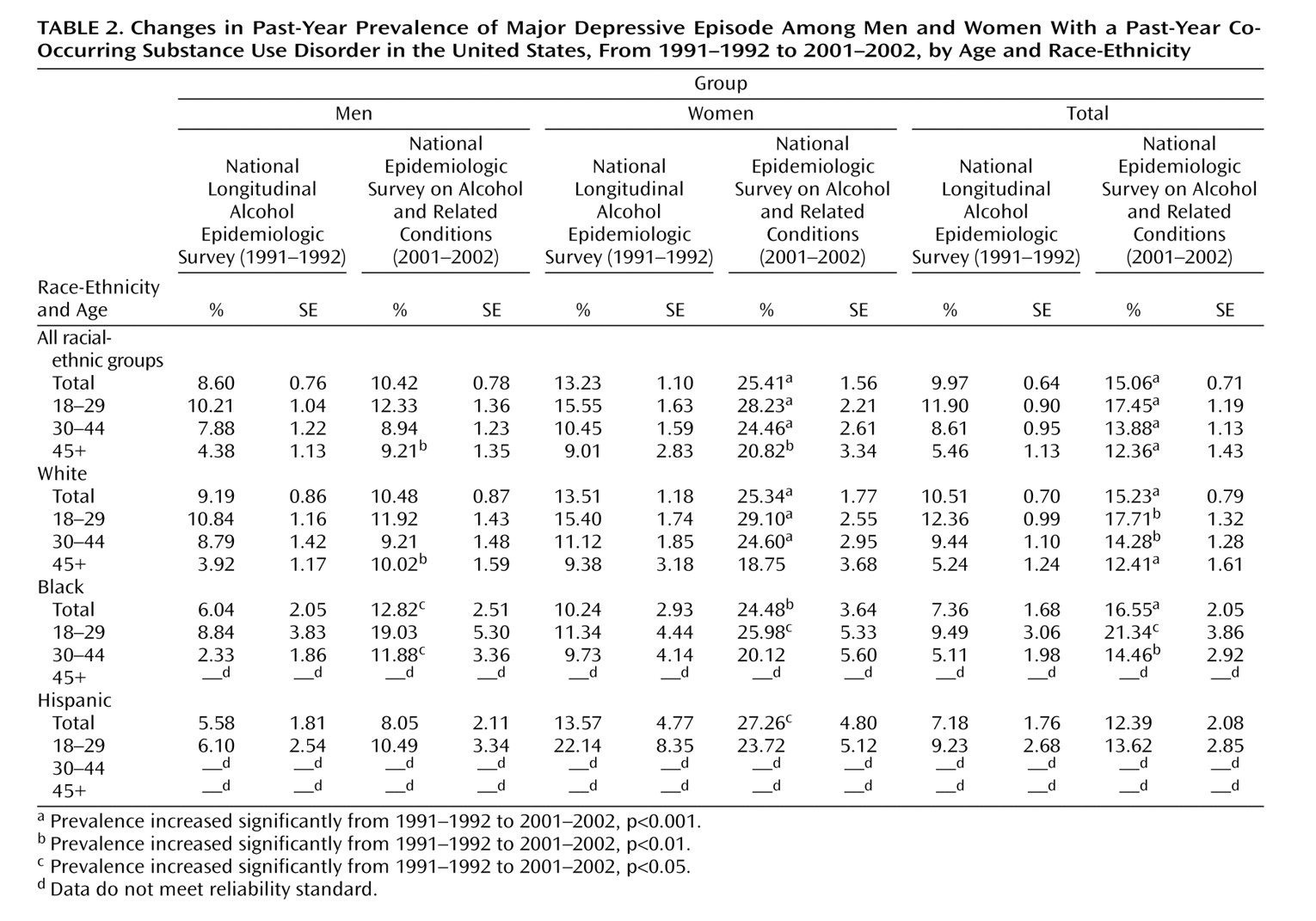
As shown in
Table 2, past-year major depressive episode among persons with a current substance use disorder increased from 9.97% in 1991–1992 to 15.06% in 2001–2002. Overall, significant increases in the prevalences of depression were observed among whites, blacks, and women and in each age group. Rates also increased significantly among whites and blacks of every age group examined and in nearly all age groups among white and black women. Statistically significant increases in depression rates were not seen for men overall, for Hispanics overall, or for most racial-ethnic-by-age subgroups of men. Increased rates of depression were only found among men age 45 years and older, white men age 45 years and older, black men overall, and black men 30 to 44 years of age.
Past-Year Major Depression Among Persons Without a Substance Use Disorder
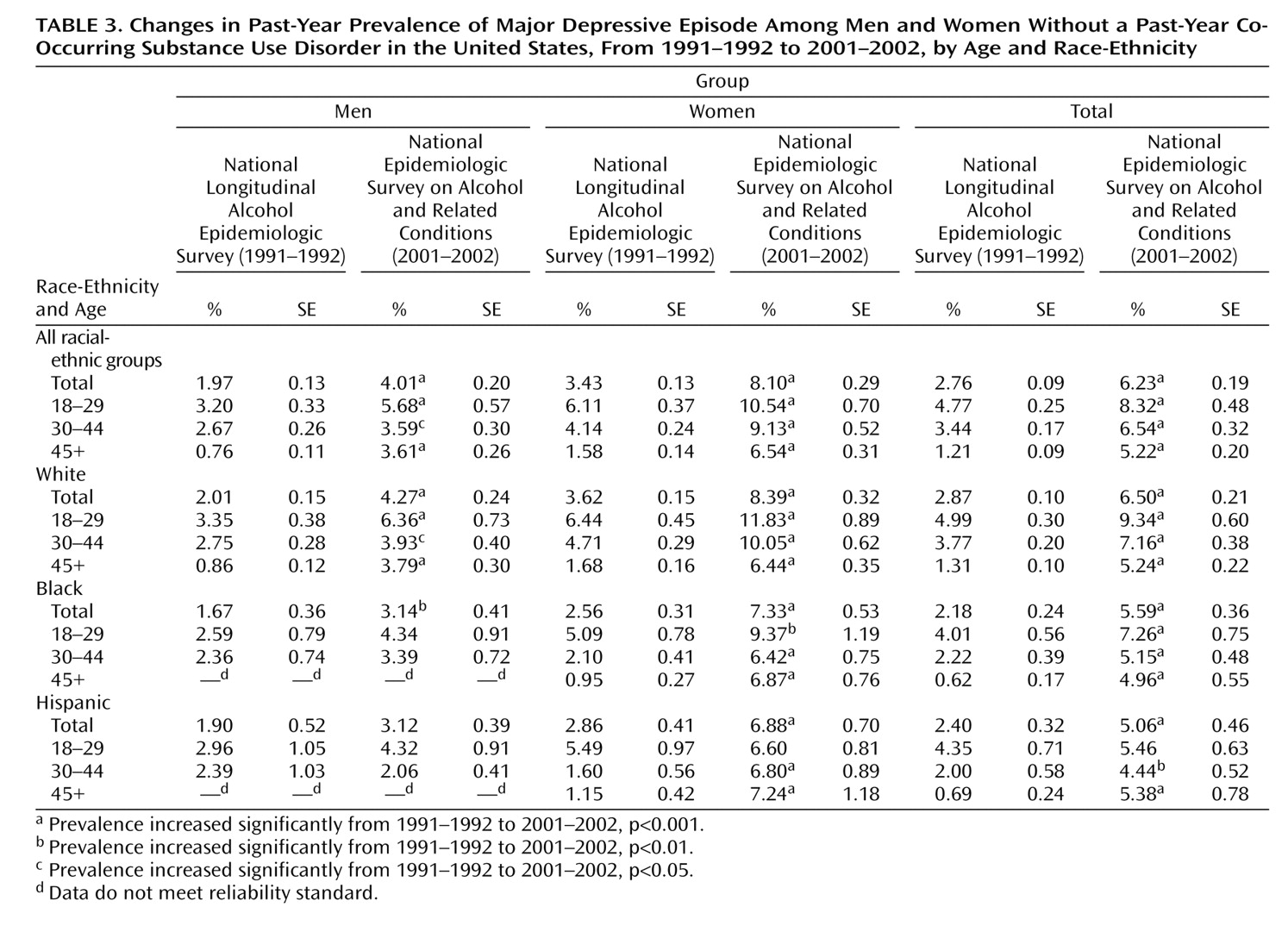
As shown in
Table 3, rates of past-year major depressive episode among persons without a co-occurring substance use disorder were substantially lower than rates among those with a co-occurring substance use disorder. In this group, the prevalence of major depressive episode increased from 2.76% in 1991–1992 to 6.23% in 2001–2002 (p<0.001). Increases were observed in nearly every age-by-race-by-sex subgroup, and most were statistically significant. In contrast, rates among Hispanic men, Hispanic women 18–29 years old, and black men in the 18-to-29-year and 30-to-44-year age groups remained stable.
Discussion
Major depression increased markedly among adults in the United States, from 3.33% in 1991–1992 to 7.06% in 2001–2002. No previous studies have been able to examine current major depression across a decade in representative samples of the U.S. adult population using consistent methods for case ascertainment. Furthermore, no previous studies of major depression have had large enough samples to allow comparison of rates of major depression across time for important subgroups of the population. Consistent increases in major depression were observed among all age, racial-ethnic, and sex subgroups, except Hispanic men in all age groups and Hispanic women 18–29 years of age. These results are not consistent with an increase in the prevalence of depression specific to a particular age cohort at a particular point in time
(4 –
8), since both older and younger groups had increased rates of depression.
To examine the hypothesis that increases in major depression may be related to changes in rates of comorbid substance use disorders, rates of major depression were examined in persons with and without current substance use disorders. For women of all ethnicities (except young Hispanic women) and for white men, increases in the rates of major depression cannot entirely be explained by increases in co-occurring substance use disorders; rates of major depression increased significantly in the total sample and among those with and without co-occurring substance use disorders. For black men, increases in depression were observed in the total sample for each age group examined. However, the increases in depression among young black men with and without co-occurring substance use disorders were not significant. Taken together, these results indicate an increase in comorbid substance use disorders and major depression among young black men, in which substance use disorders may account in part for the observed increases in depression. This finding highlights the need to examine changes in substance use disorder comorbidity across time in concert with changes in the rates of major depression. Furthermore, this result underscores the need for research in which rates of various comorbid disorders are examined as confounding factors in changes in rates of depression as well as other psychiatric disorders.
In marked contrast to most subgroups of the U.S. population, Hispanic men and young Hispanic women did not have significant increases in major depression in the total sample or among those with and without co-occurring substance use disorders. A recent study of immigration and psychiatric disorders among Mexican Americans and non-Hispanic whites (24) provides a clue about the possible causes of this stability in rates. In that study, the rates of specific psychiatric disorders, including major depression, were not found to differ between foreign-born Mexican Americans and foreign-born non-Hispanic whites. However, U.S.-born Mexican Americans had a clear mental health advantage over U.S.-born non-Hispanic whites. These results supported the role of traditional cultural retention as protective against psychiatric morbidity among Mexican Americans, an effect not shared by non-Hispanic whites, and this same protective effect of cultural retention may be evidenced in the stability of rates of major depression among Hispanics observed in this study.
The striking increase in the overall rates of depression among most subgroups of the population found in this study cannot be attributed solely to recall bias or increases in the rates of substance use disorder comorbidity. How do these results compare with those of other national surveys? The main comparison is to the NCS and NCS-R studies, which show a decrease in past-year major depression in the U.S. from 10.1% in 1990–1992 to 8.7% in 2001–2002
(13,
14) . As discussed earlier, the two studies used different diagnostic classification systems (DSM-III-R versus DSM-IV), different sampling frames (ages 15–54 years versus ages 18 years and older), and different questionnaires for assessing major depression. These differences make it difficult to compare the results of those studies with our results. Future work will need to compare the specific assessments used in these different surveys so that methodological reasons for the differences in the results can be considered.
Could some other methodological artifact or confounding factor explain the increases? Although the interviews in both surveys used the same core questions to assess past-year diagnoses of major depression, the contexts within which the questions were embedded differed. In the NLAES all respondents were asked about the occurrence of past-year depressive symptoms regardless of whether they responded positively to depression screening questions. This was done to obtain a continuous scale of past-year depressive symptoms for all respondents. This additional depressive symptom section was eliminated from the NESARC because of time constraints. To determine whether this variation could have contributed to the observed increases across the decade, we examined rates of lifetime major depression, which had identical questions and context, and found increases of a magnitude similar to those found for past-year major depression (9.86% in the NLAES compared with 13.23% in the NESARC). We conclude that the contextual differences between the two interviews were unlikely to account for the increases in rates of past-year major depression. To further examine potential methodological reasons for the increase, we studied rates of endorsement of the two depression screening questions for low mood and anhedonia and found nearly identical rates in the two studies (31.6% in the NLAES and 33.8% in the NESARC). Thus, while there was no major shift in the basic propensity for low mood, there was a shift in the full syndrome of major depression. Did the U.S. population become more willing in general between 1991–1992 and 2001–2002 to report psychiatric symptoms? If that were the case, one might expect rates of reporting to increase for all psychiatric symptoms, yet increases of the same magnitude as those found for major depression were not discerned for substance use disorders during the same period
(30,
31) . Nevertheless, it is possible that some factor specific to self-report of depressive symptoms could have influenced case ascertainment in the more recent survey. For instance, media campaigns designed to increase awareness of depression and direct advertising of antidepressants to consumers may have played a role in increased reporting of depressive symptoms. These campaigns began during the interval between the two surveys, and just such a general factor is consistent with the broad-based increases seen in this study. On the other hand, differences observed for men and women with and without co-occurring substance use disorders and between white, black, and Hispanic men and young Hispanic women argue against a general change in reporting propensity as a full explanation.
It appears that one or more general factors had an impact on rates of major depression among most subgroups of the population. Since such a rapid change cannot be explained by genetic causes, attention in future research should be drawn to environmental changes that have taken place during the past decade. Further elaboration of changes in historical and cultural factors, marital stability, health insurance status, household composition, psychiatric and medical comorbidity, and composition of the labor force and other economic indices are necessary to begin to understand the rising rates of major depression. The demonstration of possible environmental factors in the rates of major depression, of course, does not rule out the genetic vulnerability to major depression. On the contrary, environmental factors that might influence genetic liabilities may well change over time, resulting in rising rates of depression. An understanding of this type of gene-environment interaction promises to elucidate the etiology of the disorder and lead to more effective prevention and intervention initiatives in the future.
The observed increase in major depression also may have profound health care and economic implications. If the prevalence of depression continues to increase at the pace it has over the past decade, demand for services will increase dramatically in the future and may outstrip the capacity of service delivery systems. In any case, clinicians can expect to encounter depression more frequently in their practices, especially among young adults. The increases in depression rates observed in this study also suggest that the stability of estimates of the economic costs of depression over the past decade
(14) based on declining rates of major depression derived from the NCS and NCS-R have masked the true increases in the economic burden of this illness and underestimated the growing and devastating toll of depression on the quality of life of persons afflicted with this disorder and those around them.