Efforts to prevent the onset of symptoms of PTSD and depression by single-session psychological debriefing have produced mixed results, varying from no beneficial effects to even harmful effects of the intervention
(3) . In recent years, the attention has shifted from single-session interventions targeted at all trauma victims to the early treatment of victims with early diagnosis of PTSD or acute stress disorder.
Foa et al.
(4) conducted a nonrandomized controlled trial in 20 recent female assault victims who met the criteria for diagnosis of acute PTSD except for the time criterion of duration of symptoms for at least 1 month. The intervention program consisted of four sessions of cognitive behavioral therapy containing education, relaxation exercises, imaginal exposure, exposure in vivo, and cognitive restructuring. At 2 months after the assault, there were fewer cases of PTSD in the intervention group than in the comparison group. At 5.5 months, groups were only different as to the severity of symptoms of re-experiencing and depression. Although these results are promising, they await to be replicated in a randomized controlled trial in a larger cohort of patients who experienced various types of traumatic incidents.
Several randomized controlled trials on the efficacy of comparable brief early cognitive behavioral therapy programs have been carried out since the study by Foa et al. Brief cognitive behavioral therapy has proven to be efficacious in the treatment of acute stress disorder in civilian trauma survivors
(5 –
7), in victims with mild traumatic brain injury
(8), and in the treatment of acute symptoms of PTSD in physically injured trauma victims
(9) .
The aim of the present randomized controlled trial was to evaluate the efficacy of brief cognitive behavioral therapy intervention in the study by Foa et al.
(4) for patients with symptoms of acute PTSD resulting from various types of psychological trauma. Previous studies into the efficacy of brief early PTSD treatments were hampered by the absence of a nontreated comparison group, except for the study by Bisson et al.
(9) . Such a comparison group is necessary to compare the effect of the intervention with the usual decrease of PTSD symptoms during the first months after the traumatic incident. Other limitations of previous studies were small cohort sizes, lack of systematic information on therapists’ adherence to the protocol, and absence of intention-to-treat analyses
(5,
6,
8,
10) . In this study, these methodological concerns were met. Another difference between the current study and earlier effect studies on brief early cognitive behavioral therapy is that we included a heterogeneous group of victims of various traumatic events instead of victims that experienced one specific traumatic event, since this is the usual population of psychiatric outpatient clinics specializing in PTSD treatment. By doing so, we aimed to improve generalizability and facilitate implementation of the study results.
Method
Patients
Patients were included on the basis of the following inclusion criteria: 1) fulfilling diagnostic criteria for acute PTSD according to DSM-IV, ignoring the time criterion of duration of symptoms for at least 1 month, 2) traumatic event occurred between 2 weeks and 3 months before inclusion, 3) traumatic event is finished at the time of inclusion, 4) age 18 years or older, 5) proficiency in Dutch. Exclusion criteria were 1) suicidal ideation and 2) fulfilling diagnostic criteria for a psychotic disorder, organic disorder, substance abuse, or chronic PTSD according to DSM-IV. The average age at baseline was 37.5 (SD=13.0) years for the cognitive behavioral therapy group and 37.8 (SD=11.5) years for the waiting list comparison group (t=0.14, df=141, p=0.89).
Study Design
The study was conducted at the Center for Psychological Trauma at the Academic Medical Center in Amsterdam, a clinic for diagnosis and treatment of patients with trauma-related psychiatric disorders. Patients were civilian trauma survivors who were referred by the emergency room and trauma unit of the Academic Medical Center in Amsterdam, victim support workers, general practitioners, and company doctors in the Amsterdam area. Recruitment took place Dec. 1999–Aug. 2002; collection of follow-up data was completed in March 2003.
A priori criteria for successful intervention were a 60% reduction of PTSD scores in the cognitive behavioral therapy group versus a spontaneous reduction of 30% in the comparison group. Cohort size calculations showed that each group should consist of at least 49 participants (power=80% and two-sided significance level=0.05). To allow for participant attrition, we decided to enroll at least 60 patients in each group.
Patients were randomly assigned to either brief cognitive behavioral therapy or to the waiting list control condition (comparison group). Random assignment was done on a 1:1 basis using block sizes that randomly varied between six and 10 patients. Randomization was performed by the principal investigator (M.S.) on a central computer and a log file of all random assignments was kept.
Patients were invited to three assessments: a pretreatment assessment (baseline) and two follow-up assessments at 1 week and at 4 months after finishing the intervention. After full explanation of the study procedure by the research assistant, written informed consent was obtained. The study protocol was approved by the Medical Ethical Committee of the Academic Medical Center, Amsterdam.
Intervention
The cognitive behavioral therapy program was based on the model developed by Foa et al. for female victims of rape
(4) adapted by the authors (Drs. Carlier and Gersons) for victims of all kinds of traumatic events. The program consisted of four weekly cognitive behavioral therapy sessions with a duration of approximately 120 minutes per session. The first session was dedicated to information gathering and education. Additionally, the therapist noted the cognitive distortions and the situations that were avoided since the incident. In the second session, the list of avoided situations was completed and ordered according to the degree of anxiety that each situation evoked in the patient. Then, deep muscle relaxation exercises were practiced and audiotaped for use during homework assignments. Further, the patient recounted the traumatic experience in the present tense (imaginal exposure), which was also audiotaped. Hereafter, the cognitive distortions were discussed (cognitive restructuring). The patients were instructed to relive the experience between sessions two and four by listening to the audiotape and to confront avoided but safe situations several times within the following week at home (in vivo exposure). The third session consisted of review of this homework assignment, imaginal exposure (45 minutes), and cognitive restructuring. In the fourth session, the homework was reviewed and imaginal exposure (30 minutes) and cognitive restructuring took place. Finally, the therapist closed the intervention by discussing the progress of the patient.
Two experienced and trained psychotherapists administered the cognitive behavioral therapy protocol individually. Protocol adherence was ensured by monthly supervisions and measured by a rating system specifically designed for this study. In this rating system, we measured the occurrence of 1) proscribed (1=present, 0=absent) and 2) forbidden behaviors (present=0, absent=1) in audiotaped sessions, following the recommendations of Waltz et al.
(11) . Both scores were added up to an overall protocol adherence score.
Patients in the comparison group did not receive the intervention but were assessed at the same follow-up times as the patients in the cognitive behavioral therapy group. After the 4-month follow-up assessment, patients who still met diagnostic criteria for PTSD were offered the cognitive behavioral therapy program described earlier or referred to our outpatient clinic for regular 16-session PTSD treatment
(12) .
Measures
Severity of symptoms of PTSD, anxiety, and depression was assessed at three occasions: at baseline (within the first 3 months after the traumatic incident) and at the two follow-up assessments (1 week and 4 months after completion of the 4-week cognitive behavioral therapy program). Ten clinical psychologists conducted the assessments. All assessments for one patient were done by the same person. Comparability of the outcomes produced by these professionals was ensured by joint, weekly supervision by the researcher (M.S.), during which time the scores of all patients were discussed.
PTSD symptoms were measured with the Structured Interview for PTSD
(13,
14), which is a 17-item clinical interview that records the presence and severity of DSM-IV diagnostic criteria for PTSD. Each item is rated on a 0–4 scale; a score of 2 or higher is considered indicative of the presence of that particular symptom. The sum of the item scores results in the Structured Interview for PTSD total score (range=0–68), which was our main outcome measure. Higher scores indicate the presence of more symptoms. Structured Interview for PTSD scores correlate highly with clinicians’ ratings and self-report PTSD instruments
(13,
14) . For the Dutch version of the Structured Interview for PTSD, adequate internal consistency (Cronbach’s alpha=0.93) and interrater reliability were found (Cohen’s kappa=0.88)
(14) .
The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient Edition (SCID-I, Patient Edition)
(15,
16) was used to assess axis I comorbidity at baseline and at the 4-month follow-up assessment. The SCID-I, Patient Edition is a widely used structured interview for diagnosing and documenting the major axis I disorders of adults according to DSM-IV criteria. Training in the administration and scoring of the SCID-I, Patient Edition was provided by the developers of the Dutch version of the SCID-I, Patient Edition at the Stanley Foundation Bipolar Network at the University Hospital in Utrecht, the Netherlands.
States of anxiety and depression were measured with the Hospital Anxiety and Depression Scale
(17,
18), a well-established 14-item scale containing two subscales: Hospital Anxiety and Depression Scale-A (anxiety, 7 items; range=0–21) and Hospital Anxiety and Depression Scale-D (depression, 7 items; range=0–21). Higher scores indicate more anxiety and/or depression. The Dutch version of the Hospital Anxiety and Depression Scale showed satisfactory reliability and validity
(18) .
Finally, the patients in the cognitive behavioral therapy group were asked whether they were satisfied with the received intervention. This item was scored on a 1–4 scale (1=“very satisfied” to 4=“very unsatisfied”).
Data Analysis
We used chi-square tests and independent t tests to compare baseline characteristics between the two study groups, between the total study group versus patients lost to follow-up, and to compare treatment satisfaction of responders (cognitive behavioral therapy patients without diagnosis of PTSD at 4 months) with that of nonresponders (cognitive behavioral therapy patients with diagnosis of PTSD at 4 months).
We used repeated-measures analyses to study the changes over time in the Structured Interview for PTSD score and in the Hospital Anxiety and Depression Scale anxiety and depression scores between the two groups. We applied mixed-linear models to take into account that measurements within the same individual were correlated
(19) . No mathematical pattern was imposed on the covariance structure for measurements within the same individual (unstructured). These repeated-measures models have the advantage of data from all available visits being used in the analysis, not just the complete cases. The mean scores for each outcome at week 1 and at month 4 were modeled as a function of the intervention given (two levels), time since intervention (as a categorical variable with two levels), the baseline measurement (continuous), and the interaction between time and intervention. This interaction term was added to the model to allow the treatment effect to be different at the 1-week and 4-month follow-ups. The main question of whether the response pattern was different between the two study groups was evaluated by jointly testing that the treatment difference was zero at 1 week and at 4 months. Only if this overall test was significant, we examined the size of the treatment effect by calculating the difference in mean scores between the two study groups at both time points with a corresponding 95% confidence interval (CI) using our linear-mixed model.
Subgroup analyses were only carried out for the main outcome measure (Structured Interview for PTSD). Based on earlier studies on predictors for treatment of chronic PTSD, we examined the following factors measured at baseline: comorbid acute stress disorder (yes/no), comorbid major depression (yes/no), comorbid anxiety disorder other than PTSD (yes/no), prior trauma (yes/no), and time elapsed between trauma and inclusion in the study (<1 month versus 1 to 3 months). The possibility of a subgroup effect was examined by testing whether the difference in treatment effect between subgroups was significantly different from zero.
All our analyses were on an intention-to-treat basis, unless otherwise indicated. A two-tailed alpha level of p=0.05 was used to determine statistical significance. For all analyses, the Statistical Package of the Social Sciences, Version 12.0.1 was used.
Results
Patients
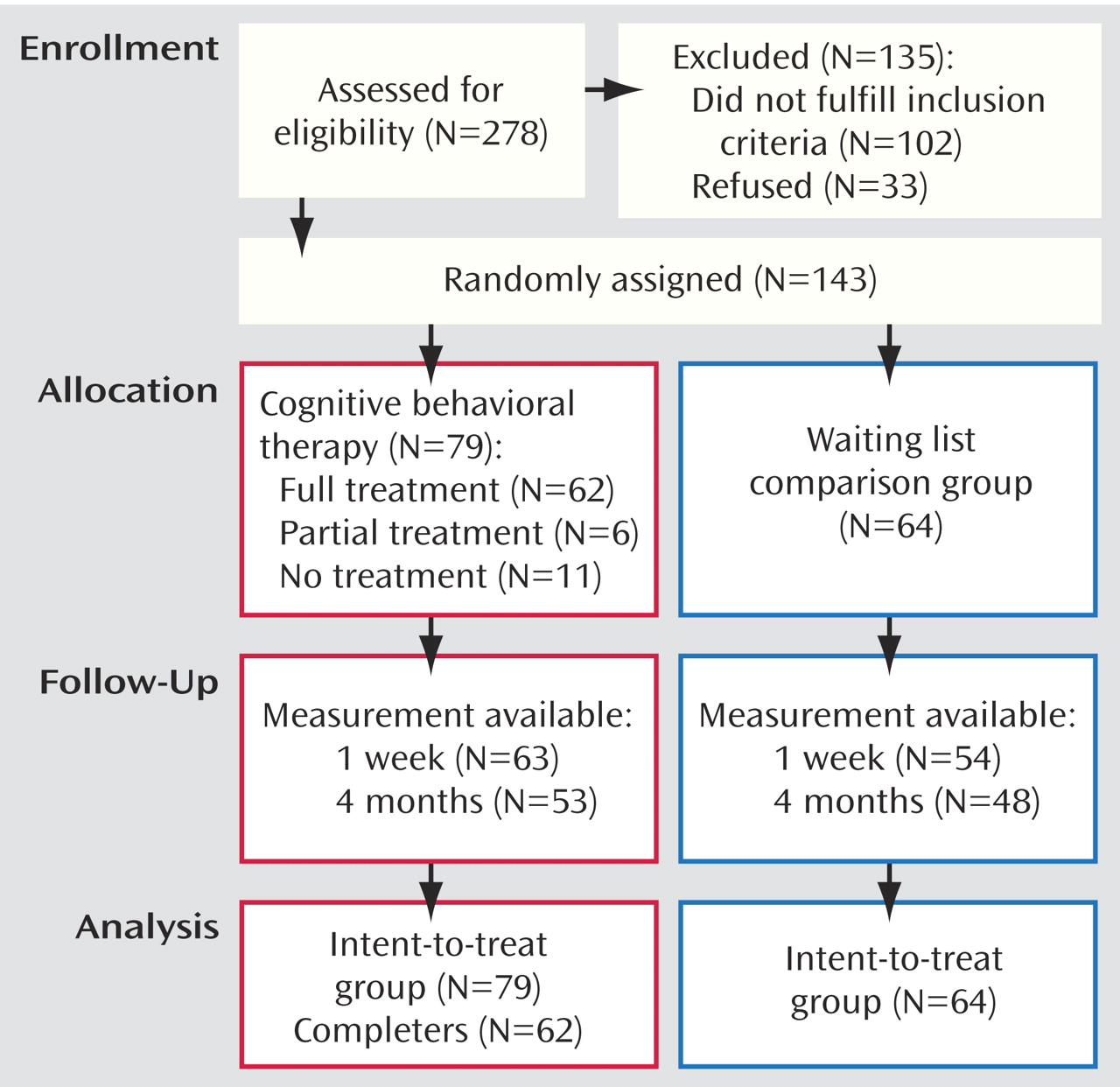
Figure 1 summarizes the flow of patients through the trial. Of the 278 respondents that were assessed for eligibility, 143 were randomly assigned. Excluded were 135 respondents because of refusal of further participation (N=33 [24.4%]), no diagnosis of acute PTSD (N=68 [50.4%]), traumatic event occurred more than 3 months before (N=2 [1.5%]), traumatic event was not over at the time of enrollment (N=7 [5.2%]), no proficiency in Dutch (N=6 [4.4%]), suicidal ideation (N=8 [2.9%]), diagnosis of substance abuse (N=5 [3.7%]), or chronic PTSD (N=6 [4.4%]) according to DSM-IV.
During the trial, it became apparent that we had more early dropout in the cognitive behavioral therapy group than anticipated, e.g., dropout after random assignment but before any treatment was given. We counteracted this loss by altering the composition of the randomization blocks in such a way that an additional 15 patients would be randomly assigned to the cognitive behavioral therapy group at the end of the trial. In all, 79 patients were randomly assigned to the cognitive behavioral therapy group and 64 patients to the comparison group. The baseline assessment took place at a mean of 40 days (range=18–92 [SD=15] days) after the traumatic incident. The mean number of intervention sessions was 3.3. Eleven (13.9%) patients who were randomly assigned to cognitive behavioral therapy did not attend any cognitive behavioral therapy sessions; three (3.8%) patients attended one session; two (2.5%) patients attended two sessions; and one (1.3%) patient attended three sessions. Sixty-two (78.5%) patients completed the full four-session cognitive behavioral therapy program. Reasons for treatment dropout were refusal (N=10 [55.6%]), physical health problems (N=3 [16.7%]), or other reasons (N=5 [27.8%]).
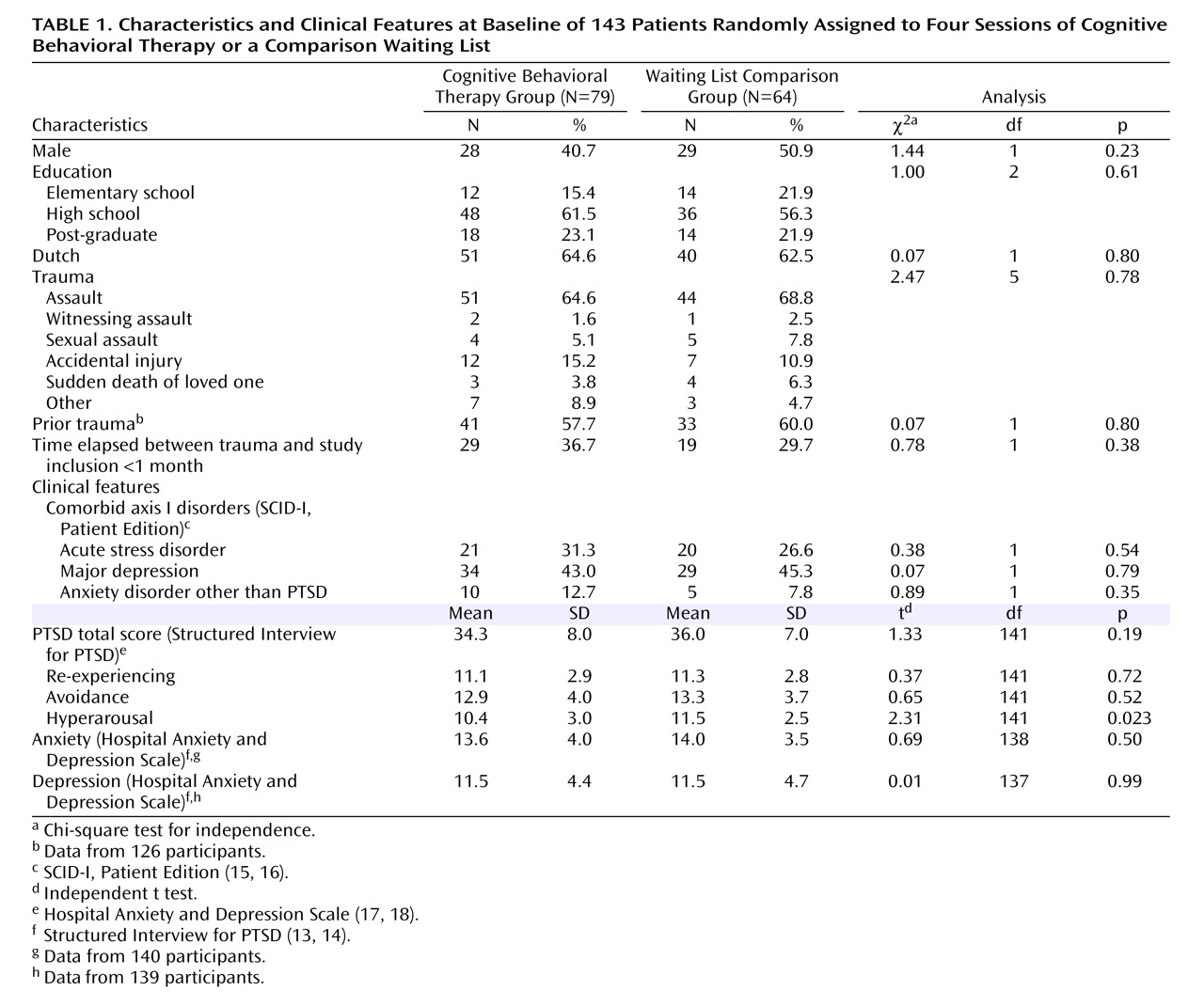
Baseline characteristics of the two study groups are given in
Table 1 . Of 10 (12.7%) cognitive behavioral therapy patients and five (7.8%) comparison patients who fulfilled criteria of one or more anxiety disorders other than PTSD, one (1.3%) cognitive behavioral therapy patient and two (3.1%) comparison patients had a panic disorder without agoraphobia; four (5.1%) cognitive behavioral therapy patients and two (3.1%) patients in the comparison group had a specific phobia, three (3.8%) cognitive behavioral therapy patients and one (1.6%) comparison patient had a social phobia; and one (1.3%) cognitive behavioral therapy patient had a generalized anxiety disorder. One (1.3%) cognitive behavioral therapy patient fulfilled criteria of both panic disorder without agoraphobia and specific phobia. No differences in baseline characteristics between the cognitive behavioral therapy group and the comparison group were found, except that the hyperarousal score at baseline was significantly lower in the cognitive behavioral therapy group than in the comparison group (
Table 1 ).
More men dropped out at the 4-month follow-up assessment than women (χ 2 =3.9, df=1, p=0.05). No other differences in baseline characteristics between the patients who completed the follow-up period and the patients who dropped out were found. Similarly, there were no significant differences in baseline characteristics comparing the cognitive behavioral therapy patients who completed all four treatment sessions with the cognitive behavioral therapy patients who received 0–3 sessions.
Treatment Integrity
We randomly selected 22 interventions (32.4% of all started interventions) for independent scoring of protocol adherence by two raters. Interrater reliability was good, with an intraclass correlation coefficient of 0.76 (95% CI=0.51–0.89). The mean total protocol adherence score was 71 (range=53–91), meaning that according to the raters, 71% of the desired protocol components occurred during the cognitive behavioral therapy intervention.
Main Outcomes
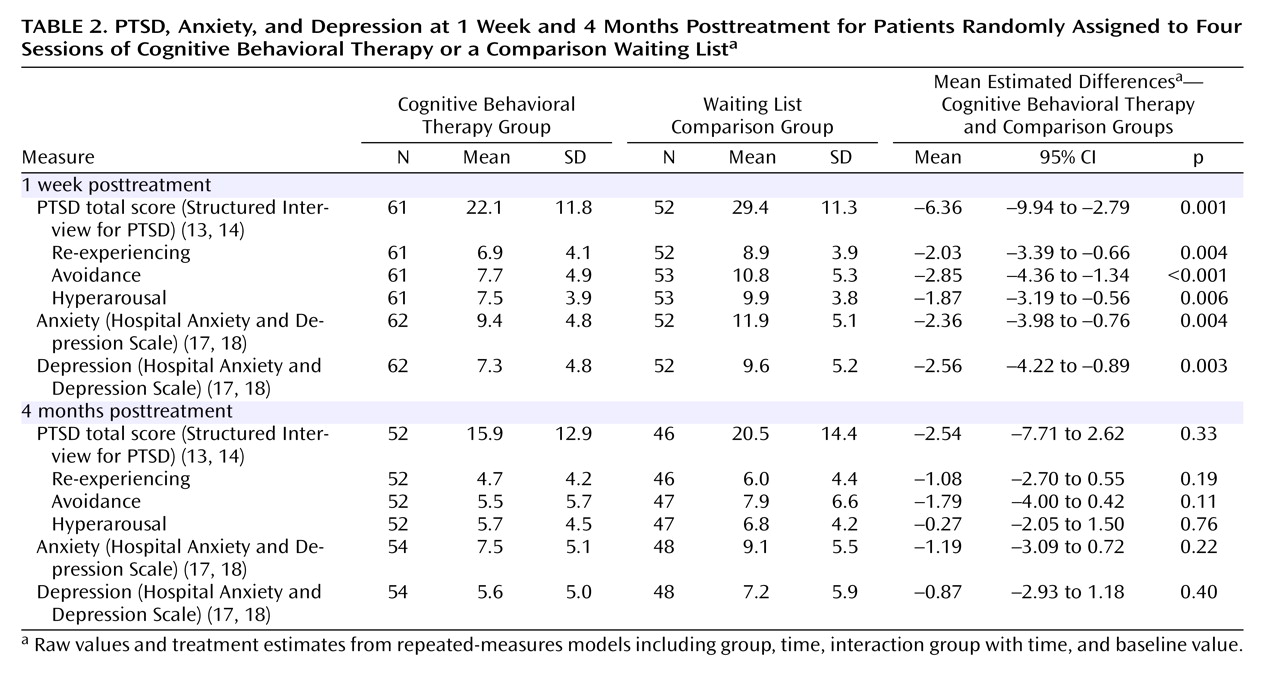
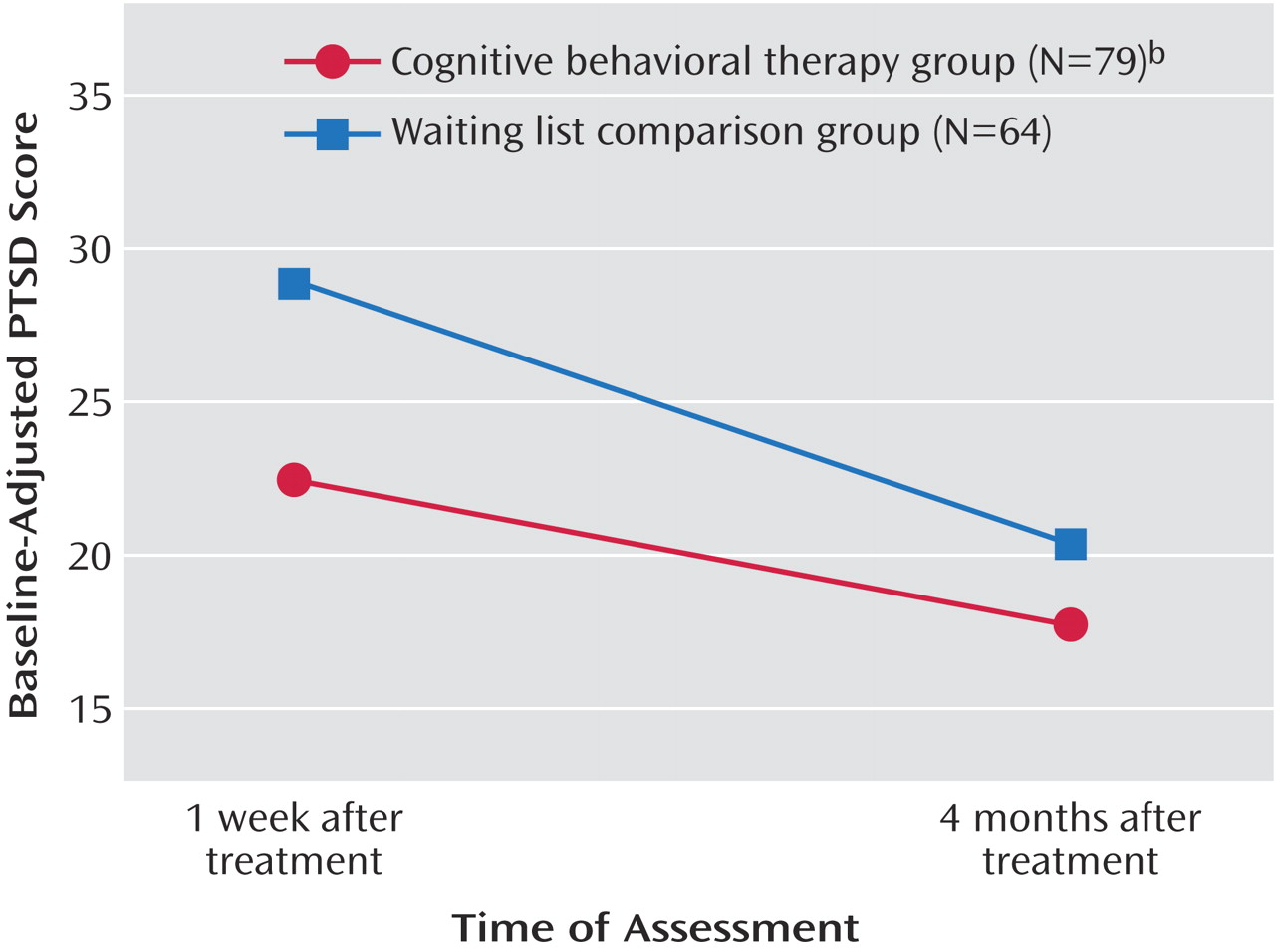
The results of the intention-to-treat analyses based on all 143 subjects are shown in
Table 2 and
Figure 2 . The mixed-model analysis on main outcome measure Structured Interview for PTSD score showed a significant main effect of time (F=35.95, df=31, p<0.001) and group (F=5.27, df=110, p=0.02), but no significant interaction between time and group (p=0.10). The overall test for a treatment effect for Structured Interview for PTSD scores was significant (F=6.82, df=2, 112, p=0.002). Analysis by follow-up time revealed that Structured Interview for PTSD scores were significantly lower in the cognitive behavioral therapy group than in the comparison group at 1 week (t=–3.53, df=109, p=0.001), but this difference was no longer significant at the 4-month follow-up (t=–0.98, df=84, p=0.33) (
Table 2 ).
The mixed-model analysis on the Structured Interview for PTSD subscale of re-experiencing showed a significant main effect of time (F=37.94, df=32, p<0.001), a significant main effect of group (F=5.53, df=111, p=0.02), and no significant time-by-group interaction (p=0.21). The overall test for a treatment effect for re-experiencing was significant (F=4.34, df=2, 112, p=0.06). Analysis by follow-up time revealed that re-experiencing scores were significantly lower in the cognitive behavioral therapy group than in the comparison group at 1 week (t=2.94, df=112, p=0.004), but this difference was no longer significant at the 4-month follow-up (t=1.31, df=103, p=0.19) (
Table 2 ).
Mixed-model analysis on the Structured Interview for PTSD avoidance showed a significant main effect of time (F=18.55, df=42, p<0.001) and group (F=8.24, df=107, p=0.005), but no significant interaction effect of time-by-group (p=0.30). The overall test for a treatment effect for avoidance was significant (F=7.02, df=2, 112, p=0.001). Analysis by follow-up time revealed that avoidance scores were significantly lower in the cognitive behavioral therapy group than in the comparison group at 1 week (t=–3.74, df=111, p<0.001), but not at 4 months (t=1.61, df=100, p=0.11) (
Table 2 ).
For Structured Interview for PTSD hyperarousal, there was a significant main effect of time (F=31.82, df=38, p<0.001) and group (F=2.50, df=109, p=0.12) and no significant interaction between time and group (p=0.005). The overall test for a treatment effect for hyperarousal was significant (F=4.81, df=2, 112, p=0.01). Analysis by follow-up time showed that Structured Interview for PTSD scores were significantly lower in the cognitive behavioral therapy group than in the comparison group at 1 week (t=2.82, df=111, p=0.006) but not at 4 months (t=0.30, df=101, p=0.76) (
Table 2 ).
The “completers-only” analyses, in which the 17 patients who did not complete the full cognitive behavioral therapy program were excluded, revealed comparable results both for Structured Interview for PTSD total score and for subscale scores of re-experiencing, avoidance, and hyperarousal.
One week after the intervention, PTSD was diagnosed in 24 (38.1%) participants in the cognitive behavioral therapy group versus 33 (61.1%) participants in the comparison group. The relative risk for PTSD if no treatment was given was 1.60 (95% CI=1.10–2.35) and the number needed to treat
(20) was 4.3, meaning that 4.3 patients needed to be treated to prevent one case of PTSD at the 1-week follow-up. At the 4-month follow-up assessment PTSD was diagnosed in 14 (26.4%) participants in the cognitive behavioral therapy group and in 21 (43.8%) participants in the comparison group (relative risk=1.66, 95% CI=0.95–2.88; number needed to treat=5.8 patients).
Secondary Outcomes
The mixed-model analysis on Hospital Anxiety and Depression Scale anxiety scores showed a significant main effect of time (F=26.29, df=37, p<0.001) and group (F=5.34, df=109, p=0.02), but no significant interaction effect between-group and time (p=0.19). The overall test for a treatment effect measured by Hospital Anxiety and Depression Scale anxiety was significant (F=4.27, df=2, 112, p=0.02). One week after the intervention, the cognitive behavioral therapy group displayed significantly lower Hospital Anxiety and Depression Scale anxiety scores than the comparison group (t=2.91, df=106, p=0.004), but not at the 4-month follow-up (t=1.24, df=90, p=0.22). The “completers-only” analyses on Hospital Anxiety and Depression Scale anxiety, excluding the 17 patients who did not complete the full cognitive behavioral therapy program, showed very similar results.
Mixed-model analysis on Hospital Anxiety and Depression Scale depression scores also revealed a significant effect of time (F=16.34, df=28, p<0.001) and group (F=4.30, df=109, p=0.04) and no significant interaction effect between group and time (p=0.07). Additionally, the overall test for treatment effect measured by Hospital Anxiety and Depression Scale depression was significant (F=5.16, df=2, 111, p=0.007). At the 1-week follow-up the cognitive behavioral therapy group had significantly lower Hospital Anxiety and Depression Scale depression scores than the comparison group (t=3.05, df=107, p=0.003), but at the 4-month follow-up there were no significant differences between the cognitive behavioral therapy and the comparison group in Hospital Anxiety and Depression Scale depression scores (t=0.85, df=87, p=0.40). The “completers-only” analyses on Hospital Anxiety and Depression Scale depression, excluding the 17 patients who did not complete the full cognitive behavioral therapy program, showed very similar results.
At the 4-month follow-up assessment, 10 (19.6%) patients in the cognitive behavioral therapy group and 10 (22.7%) patients in the comparison group fulfilled criteria for major depression. Six (11.8%) patients in the cognitive behavioral therapy group and one (2.3%) patient in the comparison group fulfilled criteria for one or more anxiety disorders other than PTSD; of those, one (2.3%) comparison patient had a panic disorder without agoraphobia, two (3.9%) cognitive behavioral therapy patients had a social phobia, and three (5.9%) cognitive behavioral therapy patients had a specific phobia. One (2.0%) cognitive behavioral therapy patient fulfilled criteria for both panic disorder without agoraphobia and generalized anxiety disorder. Finally, one (2.0%) patient in the cognitive behavioral therapy group and one (2.3%) patient in the comparison group fulfilled criteria for alcohol use.
When asked to evaluate their satisfaction with the intervention, 93.2% of responders (patients with diagnosis of PTSD at 4 months) and 100% of nonresponders (patients without PTSD at 4 months) in the cognitive behavioral therapy group reported being “very satisfied” or “satisfied,” whereas 5.4% of responders and 0% of nonresponders were “very unsatisfied” (χ 2 =0.34, df=1, p=0.56).
Subgroup Analyses
We considered the following subgroup analyses: baseline diagnosis of acute stress disorder (yes/no), major depression (yes/no), prior trauma (yes/no) and time elapsed between trauma and inclusion in the study being less than 1 month or 1–3 months. We decided not to study the subgroup effect of one or more baseline diagnoses of an anxiety disorder other than PTSD because of the small size of that subgroup (N=11 at baseline).
We found no indication that treatment effects were different in any of these subgroups, except for major depression and time elapsed between trauma and study inclusion. Treatment effect in patients with and without comorbid major depression at baseline was not different at the 1-week follow-up (t=–0.75, df=110, p=0.45), but cognitive behavioral therapy led to significantly lower PTSD scores in patients with comorbid depression at 4 months (mean differences between cognitive behavioral therapy and comparison groups: –8.67, 95% CI=–1.03 to –16.3, t=2.02, df=110, p=0.05), whereas no such effect of cognitive behavioral therapy was seen in patients without major depression (mean differences between cognitive behavioral therapy and comparison groups: –1.73, 95% CI=–8.55 to 5.09, t=–0.50, df=110, p=0.62). Cognitive behavioral therapy was also more efficacious in reducing symptoms of PTSD in patients who were included within the first month after the traumatic incident than in patients included after 1–3 months, both at 1 week and at 4 months follow-up; the mean differences between the cognitive behavioral therapy and comparison groups in PTSD scores were –12.4 points at 1 week (95% CI=–18.6 to –6.25, t=3.98, df=110, p=0.0001) and –9.76 points at 4 months (95% CI=–18.78 to 0.74, t=2.15, df=110, p=0.03).
Discussion
Our randomized controlled trial demonstrated that a brief early cognitive behavioral therapy program accelerated initial recovery of symptoms of PTSD, anxiety, and depression measured at 1 week after the intervention. At 4 months after the intervention, differences in symptoms of PTSD, anxiety, and depression between patients treated with cognitive behavioral therapy and comparison subjects on a waiting list were no longer statistically significant.
In explaining the efficacy of the brief early cognitive behavioral therapy program in reducing symptoms of PTSD, anxiety, and depression, Foa and Kozak
(21) suggested that repeated imaginal exposure to the traumatic incident results in fear reduction, since habituation to the emotional responses to reliving of the traumatic incident between sessions occurs. Further, it is suggested that irrational beliefs of being incompetent and helpless are corrected during the brief early cognitive behavioral therapy program because the acquisition of techniques for coping with anxiety, relaxation, and cognitive restructuring helps the victim to learn to successfully control his or her anxiety, thus stimulating self-competence
(4) .
The results found in our overall study group only partly agree with previous trials in patients with acute PTSD symptoms. In accordance with the results of our mixed-model analysis, slope analyses in the nonrandomized study by Foa et al. showed that cognitive behavioral therapy patients improved faster during the first 2 months, but not later on
(4) . However, we did not replicate the modest long-term effects in the study by Foa et al. of brief early cognitive behavioral therapy on re-experiencing and depression symptoms at 5.5 months after the traumatic incident
(4), nor did we observe the differences between cognitive behavioral therapy patients and comparison subjects in symptoms of PTSD reported by Bisson et al. at their final assessment point
(9) . Moreover, our findings are less positive than those found by Bryant et al. in earlier intervention studies on brief early cognitive behavioral therapy in the treatment of acute stress disorder
(5 –
8) . There are several possible explanations for the absence of statistically significant long-term effects in our trial. First, our cognitive behavioral therapy program consisted of four sessions, whereas other randomized controlled trials showing efficacy of brief early cognitive behavioral therapy used five sessions
(5 –
9) . It has been suggested that the number of sessions in trauma-focused cognitive behavioral therapy is likely to be predictive for its efficacy, but unfortunately this hypothesis has not yet been systematically studied
(22) . Second, the lack of a long-term effect of brief early cognitive behavioral therapy for acute PTSD could also be attributed to the timing of the intervention, which was relatively late (inclusion in the trial was at a mean of 40 days after the traumatic event), whereas in most earlier studies, except for that of Bisson et al.
(9), the cognitive behavioral therapy treatment started within the first month after the trauma. Our subgroup analyses indeed revealed that cognitive behavioral therapy was more efficacious in patients who were included within the first month than in patients included between 1–3 months. Third, it is possible that cognitive behavioral therapy is especially efficacious in patients with high initial distress, such as patients with acute stress disorder, since higher levels of symptomatology allow greater room for improvement and spontaneous recovery is less likely to occur. In our trial, cognitive behavioral therapy was not more effective in patients with acute stress disorder, but we cannot rule out that this was caused by a lack of statistical power given the limited number of acute stress disorder patients (N=41) included in our trial. In fact, subgroup results in this trial show enhanced efficacy of brief early cognitive behavioral therapy for patients with comorbid major depression. Although this finding is at variance with the findings of reduced cognitive behavioral therapy efficacy among chronic PTSD patients with comorbid depression
(23), we suspect that in the early phase after a traumatic incident the presence of comorbid depressive symptoms primarily reflect a higher level of general posttraumatic distress
(24,
25) .
Methodological strengths of our trial include assignment through randomization, inclusion of a waiting list comparison group, intention-to-treat analysis, and the assessment of protocol adherence. A limitation is the attrition, with about 22% of cognitive behavioral therapy patients never starting or prematurely ending the cognitive behavioral therapy program and 8.4% of comparison patients dropping out after the baseline assessment. These percentages are comparable to those in earlier studies on PTSD treatment
(26) . Since the results of intention-to-treat analysis based on all randomized participants were very similar to the results of the completers, we expect that potential bias of our results because of attrition is unlikely, although such bias can never be ruled out completely. Second, loss of statistical power might have occurred because of heterogeneity in our cohort with respect to baseline levels of PTSD symptom score and to a larger reduction in symptoms in our patients in the comparison group than we expected when designing this trial. Third, the possibility exists that the assessment interviews positively affected recovery in the comparison group. Finally, the results of our exploratory subgroup analyses should be interpreted with caution, since this study was not originally designed to answer these hypotheses.
The current intervention can probably easily be implemented in clinical care for recently traumatized patients, since it requests limited time from health care services as well as from PTSD patients themselves. In fact, the briefness of the intervention in comparison with the 16-session PTSD treatment that is standard in our institution was an argument frequently heard from patients for participating in the trial. In addition, our results further support recommendations in recently developed practice guidelines that for patients with a severe initial traumatic response brief trauma-focused cognitive behavioral therapy may speed recovery and prevent PTSD if treatment begins 2–3 weeks after trauma exposure
(22,
27) . However, the optimal time of intervening with recently traumatized individuals remains a relevant topic of future research, preferably in a randomized trial comparing cognitive behavioral therapy applied early after the trauma with cognitive behavioral therapy offered after a few months.