Involuntary treatment of eating disorders by means of legal commitment is a controversial issue. Conflicting opinions exist regarding any involuntary treatment of a psychiatric disorder, especially eating disorders. Although patients with eating disorders are not globally incompetent, their impaired thoughts, perception, judgment, behavior, and capacity to meet the ordinary demands of basic sustenance qualify them for commitment purposes
(1). It has been suggested that coerced treatment is counterproductive and adversely affects the therapeutic relationship. Hiday’s review of the involuntary commitment literature
(2) found that two hypotheses guide outcome studies of involuntary legal commitment. One hypothesis predicts that involuntary patients will be angry and negative about their hospitalization and treatment. Thus, they will be less likely to cooperate in the hospital and in the community, thus resulting in rehospitalization. The other hypothesis predicts that the initial anger and negativism of involuntary patients will subside and that they will become positive toward their hospitalization and treatment after they receive help. Their symptoms will be minimized and functioning maximized, thus avoiding future hospitalizations.
Some researchers
(3–
5) have found that patients legally committed for involuntary treatment tend to hold more negative views of their hospitalization than patients admitted for voluntary treatment and report at discharge that little or no benefit has occurred. In contrast, other researchers
(6,
7) have found that most involuntarily committed patients who initially objected to their commitment had positive views of their hospitalization and treatment at discharge and would want to be hospitalized in the future if they became dangerously ill again. These contradictory results could be due to patients expressing negative attitudes toward certain aspects of their hospitalization while appreciating the help they received
(2).
Given the controversy of involuntary treatment in psychiatry and law, it is surprising that there is not a wealth of data on the extent and outcomes of coercion for eating disorder patients. Few empirical studies exist to allow a data-based examination of involuntary treatment of eating disorders. Ramsay et al.
(8) reported that involuntary commitment of patients with anorexia nervosa led to satisfactory short-term treatment results but increased long-term morbidity (follow-up examinations occurred a mean of 5.7 years after the first admission). The mortality at follow-up for the detained patients was 12.7%, compared to 2.6% for the voluntary patients. Sullivan
(9) reviewed 42 studies and found that the aggregate annual mortality rate from anorexia nervosa was more than twice that of female psychiatric patients with other diagnoses, reaching 0.56% per year on average.
In the state of Iowa, the requirements for legal commitment for involuntary treatment of a psychiatric disorder are similar to those in many states: 1) evidence that a psychiatric disorder is present, 2) the disorder is threatening to the life of the patient because of self-harm or neglect of vital care caused by the disorder, and 3) the patient refuses treatment.
Multiple safeguards are built into the legal process of involuntary commitment to protect the rights of the individual. A petition to the court by the family or health professional must precede all commitments. Furthermore, an evaluation by physicians unrelated to the petitioners to determine the presence, severity, and life-threatening nature of the illness is also required. A legal hearing takes place within 48 hours by a court-appointed legal examiner with counsel provided for the patient. Periodic review of the involuntary status is scheduled during the hospitalization.
The present study compares patients admitted to an inpatient eating disorder unit at a tertiary care university hospital for voluntary treatment (N=331) with patients who were legally committed for involuntary treatment (N=66). This study will assess whether involuntary and voluntary patients differ demographically and in diagnostic distribution, illness history, number of previous hospitalizations, length of hospitalization, comorbid illnesses, and psychological testing performance.
Method
A series of 397 consecutive eating disorder patients referred for treatment to the University of Iowa Hospital and Clinics eating disorder program over 7 years (July 1991 to June 1998) were reviewed. Pertinent information was retrospectively extracted from the patients’ clinical chart and recorded on a coding sheet. For patients who were admitted more than once, only information from the first admission was recorded on the coding sheet. The following information was obtained from the patients’ chart: 1) demographic data (race, gender, age, and marital status); 2) duration of the illness; 3) weight history (highest weight, weight at illness onset, lowest weight, admission weight, and discharge weight); 4) number of previous hospitalizations for the eating disorder; 5) comorbid diagnoses (diabetes, depression, alcohol abuse, and drug abuse); and 6) psychological test scores on the Eating Attitudes Test-26
(10), Eating Disorder Inventory
(11), WAIS-R, and MMPI-II.
All diagnoses were made according to DSM-IV criteria, with chart reviewers independently confirming the diagnoses. The code sheet information was double entered into an ACCESS database.
A multidisciplinary team provided treatment, which emphasized nutritional rehabilitation, cognitive behavior psychotherapy, individualized psychopharmacology, and family assessment and treatment
(12). Nutritional rehabilitation focused on achieving a normal eating pattern and weight through nurse-supervised meals and teaching about balanced patterns of nutrition. Cognitive behavior psychotherapy focused on achieving a decrease in morbid fear of fatness, a decrease in body image distortion, and acceptance of a healthy body weight, the core components of which involved group therapy, role modeling, practice shopping for food and clothing, preparing meals, and readjusting to normal everyday life. Individualized psychopharmacology was prescribed for the treatment of comorbid disorders, such as depression or obsessive-compulsive disorder. Family assessment and treatment focused on educating the family about the eating disorder, requesting the family’s support and cooperation during the treatment process, and facilitating effective communication among the family members, with individualized treatment goals set for each family.
Statistical analysis was performed by using SAS software (Cary, N.C.). A low prevalence of diabetes in our study group prohibited the analysis of comorbid diabetes. Alcohol abuse and drug abuse was combined into one category, substance abuse, to increase power. Pearson’s chi-square tested for proportional differences between the involuntary and voluntary patients for the categorical variables of diagnosis, gender, and presence of depression or substance abuse. Pearson’s chi-square was also used to test for proportional differences for these four variables after controlling for commitment status. Since the proportions among the categorical variables were similar, there was no need to adjust for their effect in the analysis, except for body mass index. Male patients were excluded from all body mass index analyses, since male subjects have a higher body mass index than female subjects and the involuntary group had only a few male patients. We did not want the few male patients in the involuntarily committed group to strongly influence any significant differences.
The continuous variables of admission weight, discharge weight, length of illness, and length of hospitalization were highly skewed. Two-sided Wilcoxon rank sum tests were performed to test for differences between the involuntary and voluntary patient groups. Wilcoxon rank sum tests use a standardized test statistic (z) that has an asymptotic standard normal distribution under the null hypothesis to compute an asymptotic linear rank sum statistic. A continuity correction was not used because it makes the z test statistics smaller and leads to the null hypothesis not being rejected as often.
Body weights were calculated by two methods: 1) body mass index (kg/m
2), which has the advantage of being reference free and is standardized by weight and height, and 2) as a percentage of the mean matched population weight (the average body weight of a reference population standardized by weight, height, and gender, as determined by Kemsley
[13]).
Results
Of the 397 patients admitted, 66 (16.6%) were referred by involuntary legal commitment.
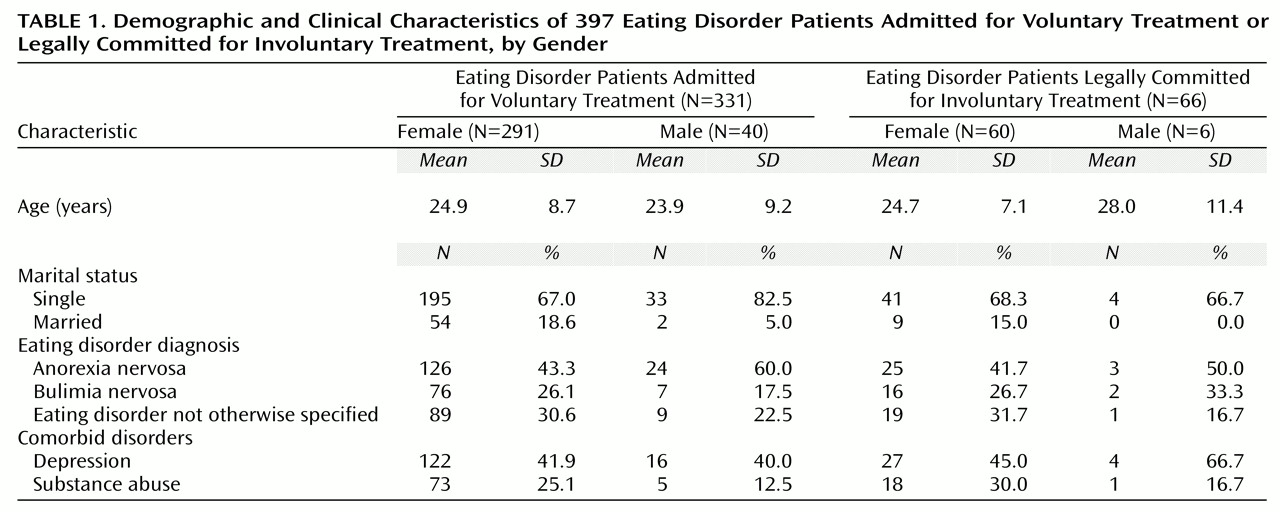
Table 1 summarizes the demographic, diagnostic distribution, and psychiatric comorbidity features of the involuntary and voluntary patients. The two groups did not differ in age, gender, marital status, diagnostic distribution, or psychiatric comorbidity.
The proportion of patients who had a history of substance abuse (involuntary patients: 28.8%, N=19; voluntary patients: 23.6%, N=78) was similar for commitment status, diagnosis, gender, and depression. The two groups had a similar proportion of subjects with depression (involuntary patients: 47.0%, N=31; voluntary patients: 41.7%, N=138).
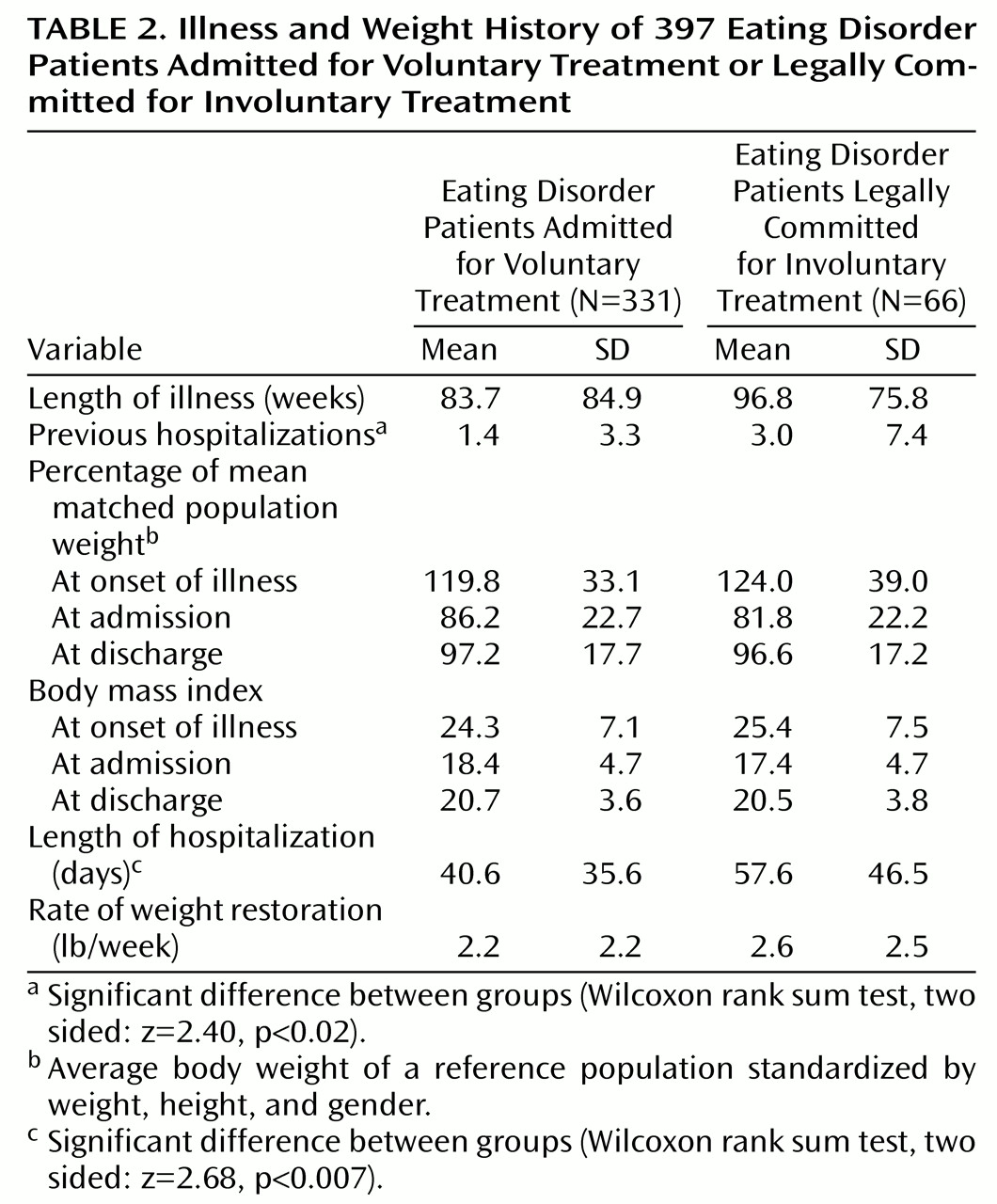
Table 2 summarizes the illness and weight history of the involuntary and voluntary patients. Both groups began dieting at weights above their mean matched population weight. At admission, the two groups did not significantly differ in their percentage of mean matched population weight or body mass index (female patients only). The illness duration of the involuntary patients was longer than that of the voluntary patients, but the difference did not reach statistical significance (Wilcoxon rank sum test, two sided: z=1.79, p<0.07).
The patients who were legally committed for involuntary treatment had significantly more previous hospitalizations than did the patients admitted for voluntary treatment, but the number of previous hospitalizations was skewed. The majority of the study patients (52.1% [N=201 of 386]) had no previous hospitalizations, whereas 2.3% (N=9 of 386) had more than 10 previous hospitalizations. Wilcoxon rank sum tests comparing previous hospitalizations of involuntary and voluntary patients conducted without these nine patients (z=2.13, p=0.03) and with them (
Table 2) showed that the extremes were not driving the significance. The overwhelming majority of the study patients (95.1% [N=367 of 386]) had five or fewer past hospitalizations.
Both involuntary and voluntary patients responded well to the refeeding program. Involuntary patients gained a mean of 18.8 pounds (SD=15.9) during their hospitalization, while voluntary patients gained a mean of 13.9 pounds (SD=14.5) (Wilcoxon rank sum test, two sided: z=2.47, p=0.01). The rate of weight restoration was not significantly different, as the involuntary patients gained 2.6 lb/week, while voluntary patients gained 2.2 lb/week (
Table 2). However, it took involuntary patients significantly more days to restore their weight (58 versus 41 days, respectively). While the involuntary patients remained in treatment for 17 more days, the proportion of patients in the involuntary group who were above 85% of their mean matched population weight (or who had a body mass index of >18) at discharge was 78.8% (N=52), which was not significantly different from the voluntary group (80.7%, N=267).
At discharge, the percentage of mean matched population weight for the two groups did not differ (
Table 2. The discharge mean matched population weight of the 28 involuntary patients with anorexia nervosa was 90.5%, which was similar to the mean matched population weight of the 150 voluntary patients with anorexia nervosa (91.2%). Discharge body mass indexes for involuntary and voluntary female patients were also similar (as mentioned earlier, male patients were not included in body mass index analyses, since male subjects have a higher body mass index than female subjects and the involuntary group had only a few male patients).
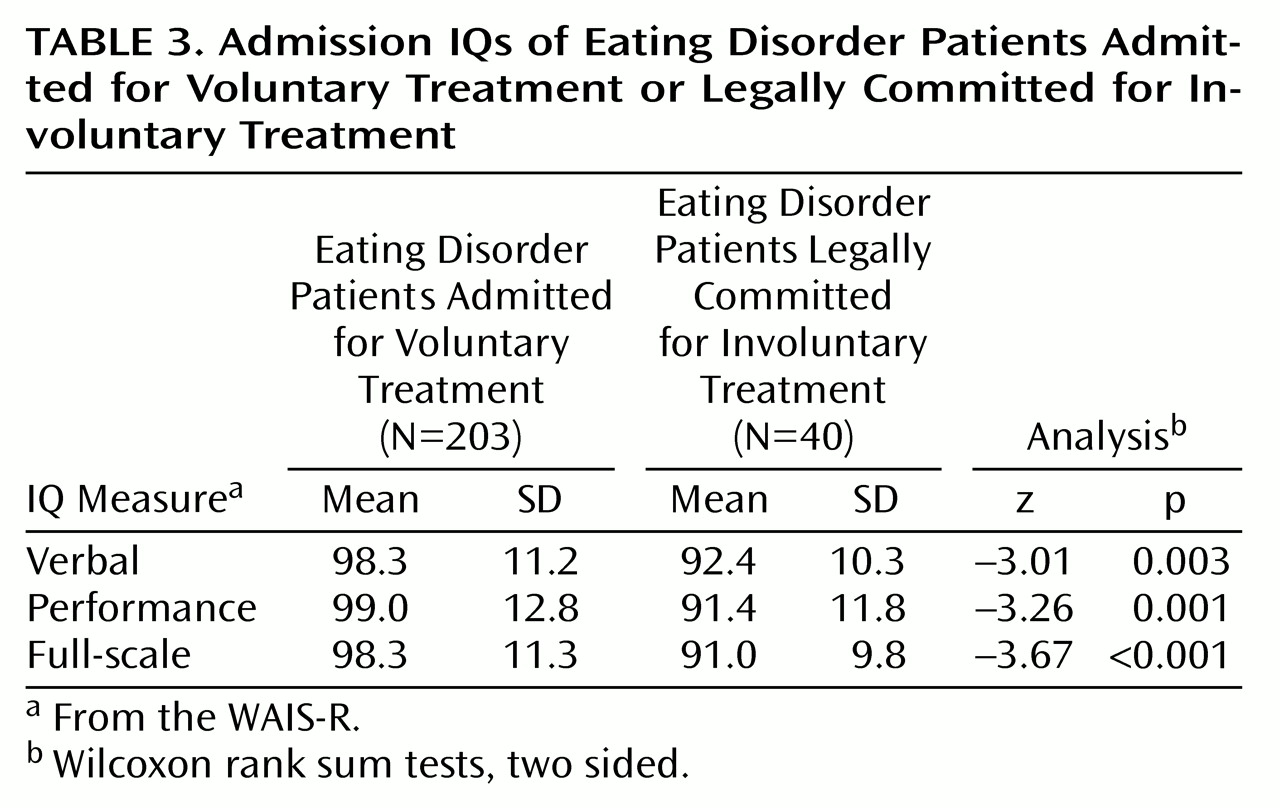
Standardized psychological testing results for the two groups at admission were similar with regard to scores on the Eating Attitudes Test-26, Eating Disorder Inventory, and MMPI-II. However, verbal, full-scale, and performance IQ measures at admission were significantly lower for the involuntary patients (
Table 3).
Discussion
In this study, patients who were legally committed for involuntary treatment of their eating disorder were similar in virtually all aspects to patients admitted for voluntary treatment except, of course, in their willingness to seek treatment for their life-threatening eating disorder. The involuntary and voluntary patients were similar in age, gender, marital status, and diagnostic distribution. However, involuntary patients had more previous hospitalizations. The frequent hospitalizations of the involuntary patients indicated that they were more resistant to treatment.
Despite the fact that the length of their hospitalization was significantly longer than that of the voluntary patients, the involuntary patients responded well to the treatment program. About 80% of both groups were discharged at weights greater than 85% of mean matched population weight. Of the involuntary patients with anorexia nervosa, 75.0% (N=21 of 28) were discharged at weights greater than 85% of their mean matched population weight, compared to 72.7% (N=109 of 150) of the voluntary patients with anorexia nervosa. The overall mean weight of the involuntary group at discharge was not significantly lower than that of the voluntary group, which suggests that legal detainment for treatment does not necessarily prevent the development of a therapeutic alliance or clinical improvement. After discharge from inpatient care, the legal commitment of the involuntary patients was often transferred to outpatient follow-up to maintain their weight and prevent future hospitalizations. The longer hospitalization of involuntary patients was proportional to their lower body mass index at admission. The impact of comorbid diabetes on involuntary treatment outcome could not be determined because of a low prevalence in our study population.
Anecdotally, many of the involuntary patients reported to the treatment team at the time of discharge that they recognized and endorsed the need for treatment. Not a single patient in this study entered a legal complaint or complaint to a medical society after discharge regarding the inappropriateness of the involuntary commitment or even informally complained that the treatment was unnecessary. This change in attitude suggests that the initial negative attitude might have resulted from the patient’s illness or an unrealistic appraisal of the usefulness of treatment
(7). It also supports the need to treat some seriously ill patients against their will.
A comparison of psychological test results at admission for the detained and voluntary patients revealed no difference in scores on the Eating Attitudes Test-26, Eating Disorder Inventory, or MMPI-II. However, results of verbal, performance, and full-scale IQ measures from the WAIS-R were lower for the detained patients, which suggests that these patients may have slightly less capacity to recognize the severity of their condition and seek treatment.
This study does not resolve important philosophical, legal, or moral issues of whether any person should be involuntarily committed for treatment of a psychiatric disorder. Nevertheless, there appears to be selected cases of eating disorders that are life threatening and associated with core features of denial of illness or thinness to a degree that the use of involuntary legal commitment may be appropriate. At times, the comorbid depressive illness or personality disorder or both that often accompanies an eating disorder may have added to the denial of illness and unwillingness to seek treatment. It appears that a relatively small proportion of the eating disorder population (16.6%, N=66 of 397 in our study) is severely ill enough to be detained for treatment.
One could argue that eating disorder patients could be treated effectively as outpatients. Several well-designed and controlled studies that compared hospitalization to outpatient treatment of the mentally ill showed that outpatient treatment was as good as or better than inpatient care and usually less costly
(14). However, studies on outpatient treatment of life-threatening forms of eating disorders are limited or nonexistent.
At a minimum, this study suggests that severely ill eating disorder patients who do not recognize their need for treatment do reasonably well in short-term treatment. However, follow-up study is needed to determine the enduring effects of involuntary legal commitment to treatment of eating disorders. Ramsay et al.
(8) confirmed that short-term treatment of involuntary and voluntary patients are comparably effective, but the long-term outcome is more problematic for the involuntary patients.