It has been suggested
(1) that one pathological substrate of key clinical symptoms in schizophrenia is an abnormal cerebral midline neural circuit mediating attention and information processing. The adhesio interthalamica (or massa intermedia) is a midline structure formed from the medial borders of both thalami, which fuse into the adhesio interthalamica between the 13th and 14th weeks of gestation
(2). In an earlier in vivo magnetic resonance imaging (MRI) study
(3), the adhesio interthalamica was found to be absent more often among patients experiencing their first episode of schizophrenia than in healthy subjects. This study also found that patients without the adhesio interthalamica had larger third ventricle volumes.
We investigated whether the adhesio interthalamica is more often absent in male patients with schizophrenia than in healthy men and whether the absence may be related to the volume of the third ventricle and clinical features in the patient group.
Method
We recruited 30 male right-handed inpatients with schizophrenia diagnosed according to DSM-IV. The patients were 18–47 years old (mean age=29.4, SD=7.97). Demographic information and clinical history were obtained by using a semistructured interview. The patients had been ill for 6 months to 23 years (mean=6.4 years, SD=6.7). They had been hospitalized two to 20 times. All patients had received neuroleptic medication. The clinical variables were documented by using the Brief Psychiatric Rating Scale (BPRS), Positive and Negative Syndrome Scale, and Scale for the Assessment of Negative Symptoms (SANS).
The comparison group comprised 30 healthy right-handed male volunteers who were recruited from the community. Like the patients, they were 18–47 years old (mean age=29.2, SD=8.0), and they were also matched for educational achievement.
Neither the healthy subjects nor their first-degree relatives had a history of neurological or mental illness. Exclusion criteria for both groups were any history of serious neurological disorder (head injury, evidence of brain damage), use of benzodiazepine or cortisol medication in the last 3 months, any mental illness other than schizophrenia, or previous ECT. All patients and comparison subjects provided written informed consent after the procedures had been fully explained.
MRI images (1.5 Tesla Magnetom Vision, Siemens) were acquired by using coronal T
2- and proton-density-weighted dual-echo sequences (TR [3710 msec]/TE=22/90 msec; number of acquisitions=1; field of vision=230 mm; matrix=240×256; slice thickness=3 mm) and a three-dimensional magnetization-prepared rapid gradient echo sequence (TR/TE=11.6/4.9 msec; number of acquisitions=1; field of vision=230 mm; matrix=240×256; slice thickness=1.5 mm). For further image processing (size reduction from 16 to 8 bit, transformation to a uniform matrix of 256×256 on 192 slices of 1.5-mm slice thickness) the software package ANALYZE was used (Biomedical Imaging Resource, Mayo Foundation, Rochester, Minn.). All data sets were realigned and resampled three dimensionally according to the coordinates of Talairach with the software program BRAINS on an SGI workstation
(4,
5).
Presence or absence of the adhesio interthalamica was determined qualitatively by trained raters who were blind to subjects’ diagnosis (E.M.M. and T.F.) in T
1-weighted MRI images with established inter- and intrarater reliability (
Table 1). After we determined the midsagittal slice, the adhesio interthalamica was evaluated in the coronal
(3) and transversal plane. This procedure was applied to check for the possibility of partial volume effects. For those scans in which the raters’ assessments did not match, the raters reviewed the MRI data set together and assigned a consensus rating.
Morphometric measurement of the volume of the third ventricle was performed on the MRI data sets by using the program BRAINS
(4,
5). The anterior boundary was defined at the anterior commissure, and the posterior boundary coincided with the section immediately anterior to the last slice in which the aqueduct was seen. Interrater and intrarater reliability was found to be high (
Table 1). The length was calculated by multiplying the number of slices defined by the manually traced volume of the third ventricle.
For statistical analysis, the chi-square test was used to compare differences between the subgroups with and without the adhesio interthalamica. Student’s t test for independent samples was used to test differences in third ventricle length and volume and in clinical data between patients and comparison subjects.
Results
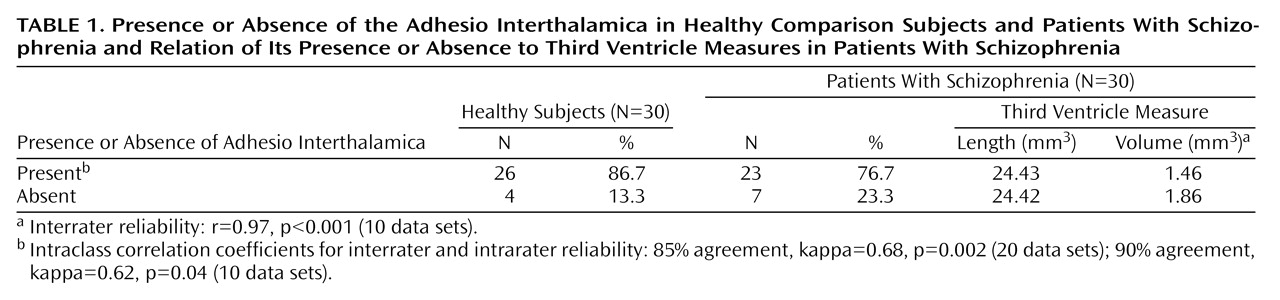
The presence or absence of the adhesio interthalamica in patients and comparison subjects is shown in
Table 1. The percentage of patients without the adhesio interthalamica (23.3%) was not significantly higher than the percentage of comparison subjects without the adhesio interthalamica (13.3%) (χ
2=1.0, df=1, p=0.31). The presence or absence of the adhesio interthalamica was not correlated with the length of the third ventricle for either group. The volume of the third ventricle was significantly larger in the patient group (t=–2.43, df=48.0, p=0.02). Nevertheless, the volume of the third ventricle was not significantly larger among patients without the adhesio interthalamica than in patients with the adhesio interthalamica (
Table 1) (t=1.34, df=7.3, p=0.22). There were no significant differences for total volume of the third ventricle between the healthy subjects without the adhesio interthalamica and the healthy subjects with the adhesio interthalamica (t=1.57, df=28, p=0.13).
The presence or absence of the adhesio interthalamica did not correlate with age for either patients with schizophrenia (t=–0.86, df=58, p=0.43) or healthy subjects (t=–0.31, df=58, p=0.77). In the patient group, there were no significant differences between patients without the adhesio interthalamica and patients with the adhesio interthalamica in age, age at onset of illness, duration of illness, and scores on BPRS and the Positive and Negative Syndrome Scale. However, the patients without the adhesio interthalamica had significantly higher SANS scores (t=–2.1, df=22.9, p=0.04).
Discussion
The presence or absence of the adhesio interthalamica did not differentiate between men with schizophrenia and healthy comparison subjects. This result is supported by the postmortem findings of Snyder et al.(3) on 41 subjects with chronic schizophrenia. However, our results are in contrast to their vivo MRI study of 52 patients experiencing their first episode of schizophrenia (3). Some methodological limitations might hinder direct comparison of that study with ours because we used standard realignment of all MRI data sets and the evaluation of the adhesio interthalamica was done in the coronal and transversal plane with 1-mm slice thickness. Nevertheless, from our viewpoint it seems reasonable to interpret our results as influenced by the relatively small number of subjects in the study.
In our study, the patients with schizophrenia had larger volumes of the third ventricle, but there were no significant differences for total volume of the third ventricle between the patients with and without the adhesio interthalamica.
Interestingly, the patients without the adhesio interthalamica had higher scores for negative symptoms on the SANS. Although our conclusions can only be tentative because of the limited number of subjects involved, our preliminary findings suggest that patients without the adhesio interthalamica are characterized by more severe negative symptoms.