Several studies have observed a negative association between rheumatoid arthritis and schizophrenia
(1) and in abnormal immune function in patients with schizophrenia
(2). These observations suggest that the human leukocyte antigen (HLA) region on chromosome 6p may play a role in the development of schizophrenia, although the region might not be a single major locus in light of previous linkage studies
(3). In the Japanese population, to our knowledge, five studies have consistently shown a higher frequency of HLA-DR1 in patients with schizophrenia than in healthy subjects
(4–
8); the frequencies of subjects with HLA-DR1 were 22% versus 10% (4), 23% versus 10%
(5), 15% versus 9%
(6), 16% versus 11%
(7), and 22% versus 9%
(8) in patients and comparison subjects, respectively. No exception has been observed, to our knowledge. When data from the four DNA-based studies
(5–
8) are combined, the frequencies are 17% (98 out of 588) in patients with schizophrenia and 10% (93 out of 942) in the comparison subjects (χ
2=15.30, df=1, p=0.00009). This result suggests an association between the presence of HLA-DR1 and schizophrenia in the Japanese population.
The mechanism of association remains unknown; however, several genetic and environmental factors may be correlated with the association. HLA generally plays a critical role in the control of infections and other immune functions. Also, it is widely accepted that a disturbance of neurodevelopment may be related to the development of schizophrenia. It is hypothesized, therefore, that an interaction between HLA and a peri- or prenatal infection, which can affect neurodevelopment, might be associated with schizophrenia.
The present study aimed to investigate demographic and clinical factors, which might be related to the possible mechanism of association between HLA-DR1 and schizophrenia. The most interesting factor is winter birth, which might be associated with pre- or perinatal infections; an excess of winter births in schizophrenia has been observed in several studies
(9,
10). Age at onset and gender were also studied.
Method
Subjects consisted of 367 unrelated patients (200 men and 167 women), mean age=43.5 years (SD=13.2). All patients were ethnic Japanese and met the DSM-IV criteria for schizophrenia. The patients were interviewed by one of the authors (T.S., K.N., I.K., T. Kato, and K.M.), and the clinical charts were reviewed to confirm diagnosis. Eighty-five percent (N=312) had a history of psychiatric admission. Most of the patients (N=303) had participated in our previous studies
(5,
7,
8). The patients were recruited from the inpatient and outpatient clinics of the departments of psychiatry of several mental or university hospitals, including Kichijoji Mental Hospital, Tokyo; Toda Mental Hospital, Saitama; Teikyo University Hospital, Tokyo; Mizonokuchi Hospital, Teikyo University, Kawasaki; Michinoh Mental Hospital, Nagasaki; Hokkaido University Hospital, Sapporo; and Shiga University Hospital, Shiga. Written informed consent was obtained from all patients.
The typing of HLA-DR specificity was performed by means of polymerase chain reaction-based microtiter plate hybridization, except in a small portion of the patients who had been studied by means of the sequence specific polymerase chain reaction method
(5). Details of the polymerase chain reaction-based microtiter plate hybridization method have been described elsewhere
(7,
8).
Clinical and demographic data, including season of birth, sex, and age at onset, were compared between the patients with and the patients without HLA-DR1. Data were collected from clinical records and, when available, by interviewing the patients and/or their family members. The onset of the disease was defined as the time the psychotic symptoms first appeared. Regarding the season of birth, frequencies of the subjects born in February and March were compared between the patients with and the patients without HLA-DR1. This was in light of a recent large epidemiological study
(10) that clearly showed the highest risk of schizophrenia for births in these 2 months, with the peak at the beginning of March. Statistical analyses were conducted by means of the chi-square method for gender and season of birth and Welch’s t tests for age at onset.
Results
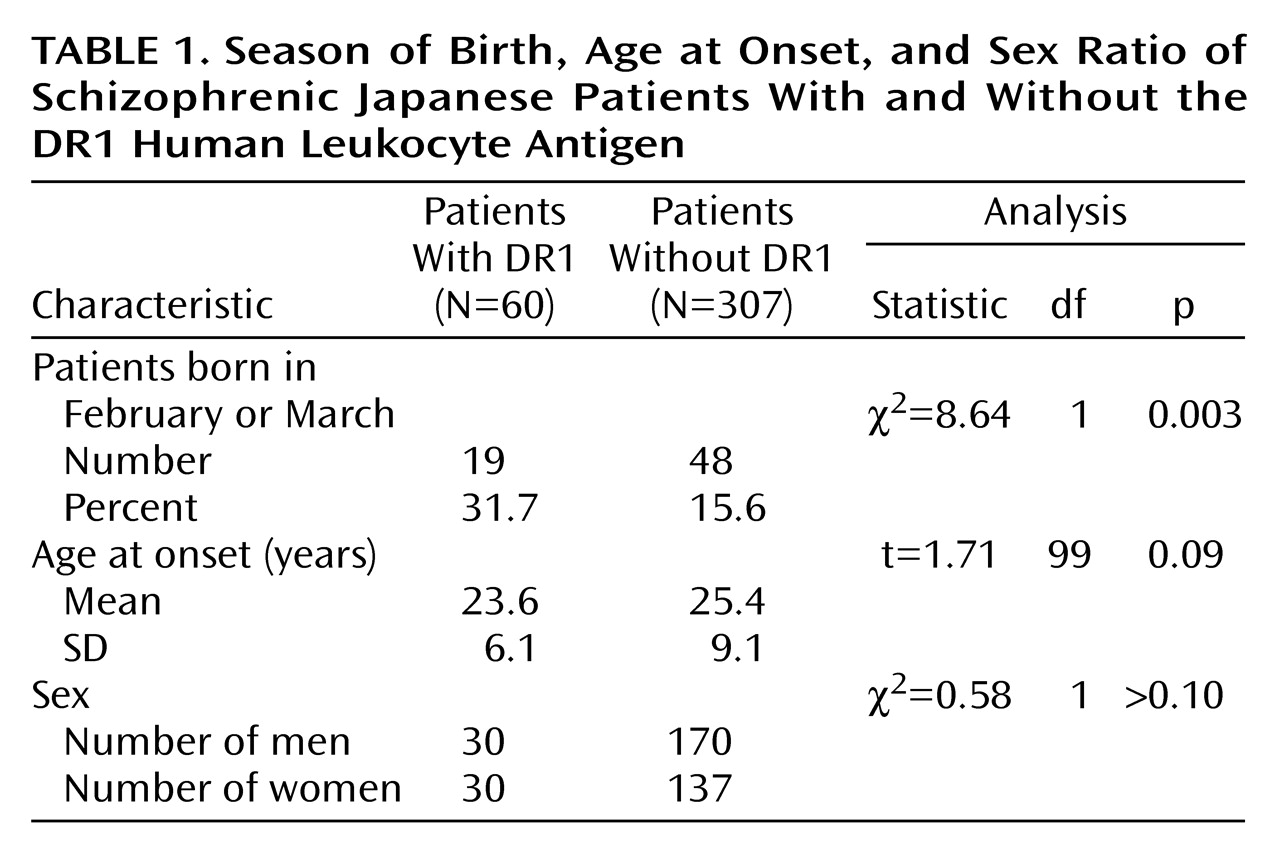
As summarized in
Table 1, a significantly greater incidence of births in February and March was observed in patients with than in patients without HLA-DR1 (χ
2=8.64, df=1, p=0.003). No significant association was observed between the presence of HLA-DR1 and other variables, including gender and age at onset.
Discussion
Consistent observations in Japanese studies have indicated a positive association between schizophrenia and the presence of HLA-DR1 in ethnic Japanese. In the present study, a significantly greater prevalence of births in February to March was observed in the patients with than in those without HLA-DR1 (χ2=8.64, df=1, p=0.003), whereas no association was observed between the presence of HLA-DR1 and other variables. Although this result is preliminary, it suggests that an interaction between HLA-DR1 and a factor associated with winter births might be related to the development of schizophrenia. The factor is not yet specified; however, an infection during the gestation or perinatal period is a candidate. The stress of cold temperatures during winter is another candidate.
Several limitations should be borne in mind in the interpretation of the present result. A number of initially “significant” genetic associations in schizophrenia have proved false positive. The present result is preliminary and could be a chance observation. We focused on births in February and March in light of a recent clear result, which observed, in an elaborate experimental setting, the highest risk of schizophrenia for births in these months, with the peak at the beginning of March
(10). The study
(10) was from a Danish population; therefore, our result, in ethnic Japanese patients, should be cautiously interpreted. If we consider this controversial element in previous studies, the peak of risk might be slightly different between populations or ethnic groups, although several studies have provided support for risk in those months
(9,
10). When other winter months (November to January) were added to the analysis in light of this issue, an association (χ
2=3.60, df=1, p=0.06) was observed between the presence of HLA-DR1 and births during the winter season (November through March).
Nonetheless, our finding is of great interest. It suggests that, at least in the Japanese population, a genetic factor (a specific type of HLA) may play a role in the development of schizophrenia by interacting with a factor that is related to winter birth. This result might provide a clue to future etiological studies of schizophrenia. Also, if an interacting factor is unique to certain populations or ethnic groups, it might account for inconsistent results between different populations or ethnic groups in genetic studies of schizophrenia
(2,
8). Further investigations are highly recommended.