The majority of data from epidemiology and clinical studies suggest that generalized anxiety disorder and major depression co-occur more frequently than would be expected by chance
(1–
3). The co-occurrence of these two disorders is associated with significantly greater psychiatric comorbidity, social and occupational impairment, and suicidal ideation and suicide behavior compared with either disorder without the other
(4–
7). Previous evidence suggests that the onset of generalized anxiety disorder occurs before the onset of major depression in the majority of cases
(8–
10) and that in some cases, generalized anxiety disorder may be a precursor to the onset of major depression
(1,
2,
4–
6,
8).
Despite the well-documented finding that most people with one mental disorder will develop at least one other disorder in their lifetime, there remain relatively few data on the feasibility of the prevention of secondary comorbidity and even less that describe effects associated with specific types of treatment. The goal of the current study was to determine the association between the treatment of generalized anxiety disorder and the risk of depression among adults in the community.
Method
The National Comorbidity Survey is based on a national probability sample of individuals 15–54 years of age in the noninstitutionalized population
(11). Fieldwork was carried out between September 1990 and February 1992. There was an 82.4% response rate. The total sample includes 8,098 interviewed respondents. The data were weighted for differential probabilities of selection and nonresponse. Weights are described in detail elsewhere
(11,
12).
The group under study consisted of respondents with diagnoses of generalized anxiety disorder (lifetime prevalence) (N=219), either with depression (with onset occurring after onset of generalized anxiety disorder) or without depression. Diagnoses were generated from a modified version of the World Health Organization (WHO) Composite International Diagnostic Interview, a structured interview designed for use by lay interviewers
(13). WHO field trials and National Comorbidity Survey clinical reappraisal studies have documented acceptable reliability and validity for these diagnoses
(13–
15).
For the diagnostic sections that assessed symptoms of generalized anxiety disorder, respondents were asked whether they had ever seen a mental health specialist (defined as a psychiatrist, psychologist, or social worker) regarding these symptoms, been prescribed a medication for treatment of the symptoms, and whether they had taken medication for the symptoms at least four times or more. Psychopharmacologic treatment was defined as respondents who endorsed having taken psychotropic medication for generalized anxiety disorder at least four times.
Data were analyzed first using independent F-based test statistics to determine sociodemographic differences between respondents with generalized anxiety disorder and subsequent onset of major depressive disorder and those with generalized anxiety disorder and no lifetime major depressive disorder. A Cox proportional hazards model was then used to calculate adjusted hazards ratios (with 95% confidence intervals [CIs]) estimating the effect of each specific type of treatment for generalized anxiety disorder on the risk of major depressive disorder. Separate models were run with the following entered as the predictor variable: 1) treatment by a mental health specialist, 2) prescription of medication, and 3) pharmacologic treatment. Adjusted hazards ratios were produced that controlled for differences in sociodemographic characteristics (i.e., age, gender, race, education, marital status, and income), age at onset of generalized anxiety disorder, and comorbid mental disorders (lifetime).
Results
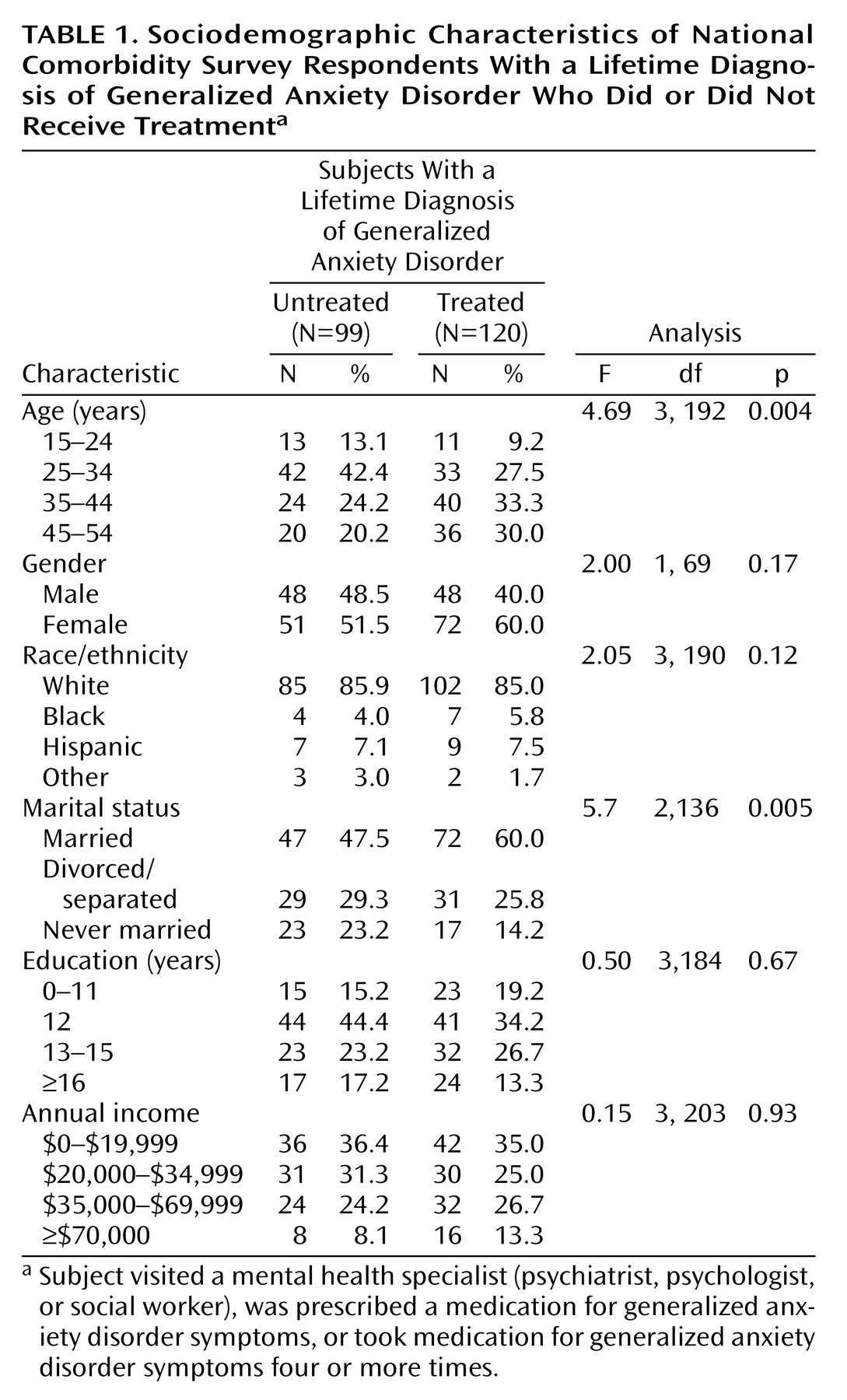
Among the survey respondents with a lifetime diagnosis of generalized anxiety disorder, there were several demographic differences between those who did and did not receive treatment for their disorder (
Table 1). Individuals who were treated were significantly older and significantly more likely to be married than were those who did not obtain treatment. Treated individuals were also more likely to be female, although this difference did not reach statistical significance.
Use of a psychotropic medication (at least four times) was associated with a lower risk of depression, with an adjusted hazards ratio of 0.52 (95% CI=0.21–0.84; p=0.001) (18.9% versus 5.73% [F=17.8, df=1, 78, p<0.0001]). Prescription of a medication for generalized anxiety disorder was not significantly associated with the risk of depression (adjusted hazards ratio=1.02, 95% CI=0.55–1.89; p=0.90) (65.4% versus 60.0% [F=0.1, df=1, 80, p=0.71]) nor was use of specialized mental health services (adjusted hazards ratio=1.10 (95% CI=0.62–1.97; p=0.70)(63.4% versus 57.9% [F=0.69, df=1, 80, p=0.41).
Discussion
Results of this study suggest that pharmacologic treatment of generalized anxiety disorder is associated with a lower risk of depression among adults in the community. This association is consistent with previous findings showing that treatment of panic attacks is associated with a lower risk of depression
(16). These results also contribute further to our understanding of the relationship between generalized anxiety disorder and depression by demonstrating specificity in the association between type of treatment for generalized anxiety disorder and the risk of depression.
The mechanism of this association is not clear, but there are several possible explanations. First, if generalized anxiety disorder is indeed a risk factor for depression, then treatment that alters or eliminates symptoms of generalized anxiety disorder should in effect eliminate a risk factor for depression, resulting in a lower risk of depression. The specificity of the association between pharmacologic treatment and lower risk of depression is in fact suggestive of a neurochemical pathway, in that pharmacologic treatment may be effective at decreasing symptoms that are depressogenic, whereas seeking help from a mental health specialist or simply receiving a prescription for medication does not appear to confer a comparable effect. This is plausible given the overlap in recommended pharmacologic treatments for generalized anxiety disorder and major depression
(7,
17,
18). Moreover, that an environmental influence (i.e., treatment) has a significant impact on who among those with generalized anxiety disorder will develop major depression is also consistent with evidence showing that despite common genetic influences for generalized anxiety disorder and major depression, environmental factors impact the expression of one or both of these disorders
(3).
Limitations of this study should be noted. First, the vague description of the specific treatment received by each respondent, as well as the timing, is a considerable shortcoming. Specifically, there is no information on the type of pharmacologic treatment that was used or on the time frame within which individuals used medication. Second, some of the covariates (education, marital status, and income) evaluated are time-dependent and may not be the same at the time of disorder onset or treatment. Third, it is possible that a third factor, such as a personality trait or personality disorder, could explain the relationship between lack of use of treatment for generalized anxiety disorder and higher risk of depression, and we were not able to examine the role of these factors in the analysis because they were not measured in this study, with the exception of antisocial personality disorder.
Future studies that further investigate the mechanism of the association between treatment of generalized anxiety disorder, other anxiety disorders, and the risk of depression will help to advance our understanding of the degree to which early intervention among those with anxiety may decrease the risk of depression. Generalized anxiety disorder is common in the general adult population
(19) and is even more prevalent in primary care
(20) and psychiatric clinical settings
(21), providing potential opportunities for clinical intervention. Replication of these findings with data on specific types of interventions used to treat generalized anxiety disorder and the risk of depression may help to make clearer the mechanism of the observed association and provide information on more specific pathways for prevention of major depression. In light of recent projections that depression will confer the greatest burden of disease worldwide in 2020
(22), the public health significance of efforts to identify routes for effective prevention of secondary comorbidity of depression cannot be overestimated.