Preschool-age children come to mental health clinics for services, manifest serious and sometimes harmful behavior, and demonstrate impaired functioning as a result of behavioral and emotional problems
(1). Yet currently there is no widely endorsed method for assessing clinically significant disruptive behavior problems in preschool children. This is a serious impediment to the goals proposed by the Surgeon General in the recent conference on children’s mental health, which include identifying early indicators for mental health problems, supporting research in developmental psychopathology that will clarify diagnoses, and encouraging early identification of mental health needs in preschool, education, and other systems
(2).
Although DSM-IV is the most widely used nosologic system for children, the majority of the fieldwork conducted for the DSM-IV was based on samples of school-age children and adolescents
(3). Emerging research has demonstrated the clinical significance of disruptive behavior problems in preschool children, but debate continues about whether such behaviors should be considered within a diagnostic framework at all. Some scientists have argued that the atypical behaviors of preschool children should not be labeled abnormal because they are often transient developmental perturbations
(4). Others have suggested that atypical behaviors in young children should not be considered a disorder of the child but rather a disturbance of the parent-child relationship
(5,
6). Other developmental psychopathologists have recommended norm-referenced assessments of a variety of behaviors and emotions in young children rather than evaluation with a diagnostic system
(7).
In summary, there is a lack of consensus about the conceptualization and measurement of disruptive behavior in preschool children. The empirical support for the validity of behavior disorders in this group needs to be examined. In this article, we 1) examine developmental issues that must be considered in regard to diagnosis; 2) summarize and synthesize research on the content, convergent, and predictive validity of preschool disruptive behavior problems, as defined by DSM oppositional defiant disorder and conduct disorder; and 3) propose a research agenda to address the current gaps in our knowledge about valid assessment of disruptive behavior problems in young children.
Developmental Issues
There is no question that the preschool period (ages 3–5) can be a difficult and challenging time for children and caregivers. Several major sociobehavioral and cognitive shifts occur during this period, including the development of self-control and the capacity to tolerate frustration. Most toddlers engage in some form of aggression and noncompliance and then learn to inhibit these behaviors and/or develop other strategies for achieving goals as they reach the end of the preschool period
(8). Given that rates of aggression and noncompliance are relatively high during the preschool period, the first question with regard to establishing the validity of DSM disruptive disorders is whether one can meaningfully and reliably distinguish typical and atypical behavior in preschool children.
There has been significant concern about the validity and appropriateness of making a diagnosis of oppositional defiant disorder and conduct disorder in young children. These concerns have centered on 1) whether clinical disorder can be reliably distinguished from normative developmental perturbation during this period, 2) whether young children are developmentally capable of engaging in the behaviors that characterize the disorder, and 3) whether functional equivalence of behaviors exists across time. We propose that a developmental approach to diagnosis has the potential to address such concerns.
A developmental approach to diagnosis assumes that the broad types and patterns of behaviors are coherent across development. This approach also requires that the assessment of behaviors and symptoms occur within the context of normative development during this period, a requirement that applies to any symptom or behavior assessed at any age. For example, sleep disturbance is evaluated in the context of normative sleeping patterns, which vary across development from infancy to geriatric populations. Similarly, although noncompliance with adult requests may be normative for toddlers and adolescents, pervasive and persistent defiance is not. A developmental approach also takes into account the effect of physical constraints on the manifestation of symptoms. For example, most preschool children are not likely to have access to firearms or knives, but they may use rocks or sticks to hurt someone. Older children may attempt to steal video equipment or cars, whereas preschool children are more likely to steal candy, money, or toys. Temper tantrums in young children may include falling down on the floor, whereas in older children a temper tantrum may involve pushing over desks. Thus, a developmental approach is one in which the symptoms or constructs are the same across development (e.g., using an object to harm someone, stealing, temper tantrums), but the manifestation of that symptom may vary.
In DSM-IV, the disruptive behavior disorders comprise oppositional defiant disorder and conduct disorder. Although historically attention deficit hyperactivity disorder (ADHD) has been included within the broader rubric of behavior problems, DSM-IV differentiates disruptive behavior (i.e., oppositional defiant disorder and conduct disorder) from problems with attention and overactivity. This distinction is supported by research that has shown different correlates, developmental pathways, and patterns of comorbidity for the two types of problems
(9). This review focuses on the disruptive behavior disorders.
Oppositional Defiant Disorder
Oppositional defiant disorder is characterized by a persistent pattern of negativistic, irritable, and noncompliant behavior (per the DSM-IV criteria). Symptoms include being argumentative and defiant, being easily annoyed by others, and frequently losing one’s temper. Symptoms such as these can be easily identified as problematic at school age, since loss of temper is infrequent and cooperation with rules and routines is expected and necessary for activities of daily life. Thus, the presence of disruptive behaviors per se is reason for clinical concern. During the preschool period, however, the distinction between normative and problematic behavior is much less clear-cut, in large part because developmental changes during this period are associated with behavioral upheaval. The emergence of increasingly sophisticated verbal skills, self-awareness, motor dexterity, and goal-directed behavior contribute to a strong push for independence on the part of the child. At the same time, parents begin to impose rules and limits, both in response to the child’s newfound autonomy and as a natural part of the socialization process. These simultaneous processes contribute to frequent clashes between the child’s self-assertions and the parents’ limit setting, leading to frequent episodes of frustration and upset.
At any developmental period, however, determination of abnormality rests on establishing that the behavior is causing “clinically significant distress or impairment in social, occupational, or other important areas of functioning” (DSM-IV, p. 7). Within this framework, oppositional or defiant behavior during the preschool period is considered clinically significant if it interferes with normal developmental functioning. Since milder forms of oppositionality are frequent during this period, qualitative and quantitative aspects of the behavior, such as its pervasiveness, intensity, and intransigence, are critical to making the distinction between oppositional defiant disorder and typical assertions of autonomy and expressions of frustration.
Conduct Disorder
The essential feature of conduct disorder is a persistent pattern of violation of rules and the rights of others, including aggressiveness and destructiveness. Two fundamental concerns about the validity of a conduct disorder diagnosis in the preschool period have been identified. First, as with oppositional defiant disorder, several behaviors that characterize conduct disorder are common during this period. In particular, aggression is a relatively common response to frustration
(8). Here, the same principles of determining clinical significance for symptoms of oppositional defiant disorder would apply to conduct disorder. A second concern is that the diagnosis of conduct disorder rests on the assumption that a child
knowingly violates rules, a supposition that requires both knowledge of the rules and intent to break them. Most preschool children are able to understand the concept of rules and can control their behavior accordingly. Preschool children have an emerging conscience and internalizations that enable them to inhibit behavior and follow rules
(10). The cognitive ability to generate hypothetical alternatives also emerges during this period
(11). Lewis and colleagues
(12) demonstrated that children as young as age 3 can deliberately engage in deception when asked about rule violation. Thus, although young children may not be fully aware of the long-term implications of their behavior, there is evidence that they have a basic understanding of the impact of their behavior on others and can control their behavior on the basis of internalized social norms.
Validity of Disruptive Behavior Disorders in Preschool Children
Over the past decade, emerging research has provided preliminary but consistent evidence of the validity of clinically significant behavior problems in preschool children. Many previous studies supported the validity of broadly defined preschool behavior problems in preschool children (for a review, see Campbell
[13]). More recent research has been focused on the DSM disruptive behavior disorders. This section reviews results from six independent programs of research testing the validity of DSM disruptive behavior disorders in preschool children. These studies were selected on the basis of the following criteria: 1) DSM-III-R or DSM-IV oppositional defiant disorder and/or conduct disorder were assessed, 2) the majority of the sample was of preschool age (3–5 years), and 3) the content, convergent, and/or predictive validity of the DSM disruptive behavior disorders in preschool children were examined.
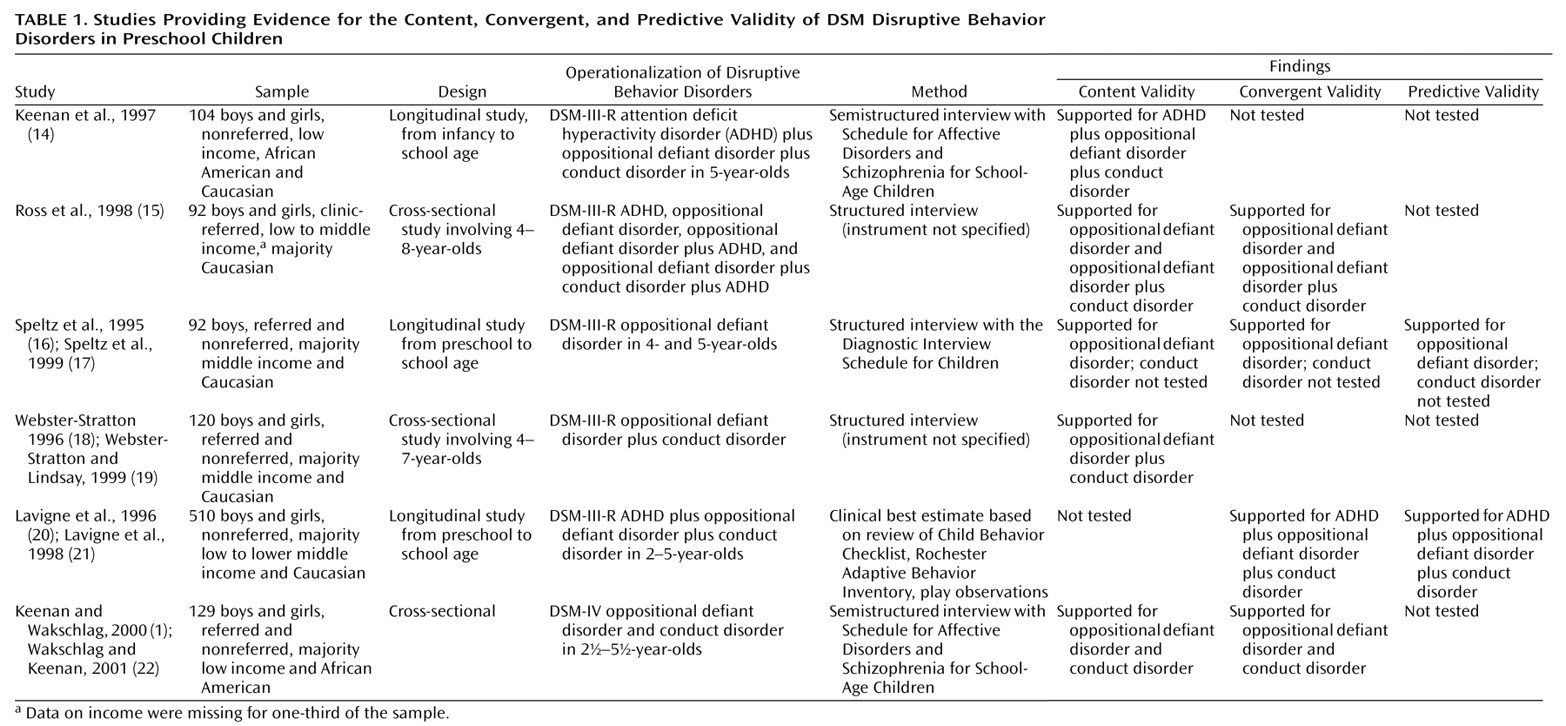
As shown in
Table 1, most of the studies tested content and convergent validity. The biggest limitation of the existing research is the lack of systematic assessment of the validity of oppositional defiant disorder and conduct disorder separately. Additional limitations include the dearth of population-based studies, underrepresentation of girls and minority groups in the samples, and lack of data on predictive validity, especially for conduct disorder. In addition, the samples in two of the six studies included school-age children. Thus, the validity data from those studies are not specific to preschoolers. Despite these limitations, these studies can be used to critically examine the existing knowledge about the validity of oppositional defiant disorder and conduct disorder in preschool children.
Content Validity
Content validity is the extent to which a test or measure covers a representative sample of the behavior domain to be measured
(23). For oppositional defiant disorder and conduct disorder in preschool children, content validity has been demonstrated by examining the association of DSM oppositional defiant and conduct disorders diagnoses with other developmentally validated measures of behavior problems, such as Child Behavior Checklist scores, observations of child behavior during standard parent-child interaction tasks, and measures of impairment. Five of the six studies have examined some form of content validity.
In a nonreferred sample of 5-year-olds living in low-income environments, Keenan and colleagues
(14) found that children who met the criteria for either DSM-III-R ADHD, oppositional defiant disorder, or conduct disorder were more likely to have externalizing scores in the clinical range on the Child Behavior Checklist. Children with these disorders were also significantly more impaired than children without disruptive or attention deficit disorders.
Ross et al.
(15) examined scores on the Eyberg Child Behavior Inventory and Child Behavior Checklist among several different diagnostic groups of preschool children, including those with ADHD only, oppositional defiant disorder only, oppositional defiant disorder plus ADHD, and oppositional defiant disorder plus conduct disorder plus ADHD. Scores on both measures fell within the clinical range for all groups. Children with a diagnosis of oppositional defiant disorder and oppositional defiant disorder plus conduct disorder had higher Child Behavior Checklist scores than children with ADHD only.
Speltz and colleagues
(16,
24) reported on a sample of 25 clinic-referred 3–6-year-old preschool boys who met the DSM-III-R criteria for oppositional defiant disorder and scored at the 98th percentile on the aggression scale of the Child Behavior Checklist. Conduct disorder was not assessed. These clinic-referred boys were compared to 25 nonreferred comparison subjects. The differences between the two groups included a higher level of observed noncompliance in the clinic-referred boys
(16).
Webster-Stratton and Lindsay
(19) examined the relation of disruptive behavior problems to social competence in a sample of 120 4–7-year-olds, half of whom were clinic-referred. Disruptive behavior problems were assessed by using a structured interview with the parent and laboratory observation and were defined as aggression, impulsivity, and oppositionality. Diagnostic specificity was not examined in this study, and rates of specific DSM disorders were not reported. Children with significant disruptive behavior were significantly impaired in social problem solving and prosocial skills with parents and peers.
Lavigne and colleagues
(20) assessed the prevalence of psychiatric disorders in preschool children in a pediatric primary care sample weighted to generate population estimates. In this study, DSM-III-R diagnoses were assigned to preschool children on the basis of several sources of information, including an adaptive behavior inventory, the Child Behavior Checklist, and play observation. Thus, all measures that typically would have been used to test concurrent validity were incorporated into the dependent measure of DSM-III-R oppositional defiant disorder, resulting in an inability to test concurrent validity independently.
To our knowledge, only one study has used a diagnostic framework to provide preliminary data on the concurrent validity of both oppositional defiant disorder and conduct disorder in preschool children. Keenan and Wakschlag
(1) tested the concurrent validity of DSM-IV oppositional defiant disorder and conduct disorder in a sample of 79 clinic-referred preschool children (2 ½ – 5 ½ years of age) living in low-income environments. These children were referred specifically for aggression, noncompliance, and severe temper tantrums. Parents were administered an established, semistructured diagnostic interview that was modified for developmentally appropriate usage. The children with a diagnosis of conduct disorder had significantly lower Children’s Global Assessment Scale ratings than the children who did not meet criteria for a disruptive behavior disorder. Both oppositional defiant disorder and conduct disorder were associated with elevated scores on the Child Behavior Checklist externalizing factor. Compared to a group of nonreferred children from similar demographic backgrounds, the children with a diagnosis of conduct disorder were more noncompliant, destructive, and aggressive in interactions with their mothers, but the children with a diagnosis of oppositional defiant disorder did not differ from the comparison subjects
(22).
Thus, there is adequate support for the content validity of disruptive behaviors problems broadly defined. Few studies, however, have systematically assessed DSM oppositional defiant disorder and conduct disorder separately.
Convergent Validity
Convergent validity is the extent to which a test or measure correlates highly with other variables with which it should theoretically correlate
(23). Convergent validity has been demonstrated by establishing that the correlates of disruptive behavior disorders in preschoolers are consistent with those established for disruptive behavior disorders in older youth. Only a few studies have examined convergent validity, and these have generally focused on parenting and family correlates. Ross and colleagues
(15) found that the level of parental stress was higher for children diagnosed with both oppositional defiant and conduct disorders than for children diagnosed with ADHD plus oppositional defiant disorder plus conduct disorder. Speltz et al.
(16) reported that both lack of positive involvement and harsh parenting were associated with preschool oppositional defiant disorder.
Lavigne and colleagues
(20,
21) compared correlates of DSM externalizing disorders in two groups of preschool children matched on age, gender, and ethnicity. Father absence, family size, family conflict, and maternal psychopathology did not differ between preschoolers who were and were not classified as having ADHD, oppositional defiant disorder, or conduct disorder. The level of negative life events was actually lower in the children with disruptive behavior disorder and/or ADHD than in the group without disorder.
In a study comparing 79 clinic-referred preschoolers to 50 nonreferred comparison subjects who were matched on ethnicity, sex, and family income, Wakschlag and Keenan
(22) assessed five primary risk domains: sociodemographic characteristics, parental psychopathology, child characteristics, family environment, and parenting. The children who met the criteria for oppositional defiant disorder or conduct disorder were more likely to have been exposed to cigarette smoke prenatally and were reported to have been more difficult to soothe as infants. There were no significant differences between children who did and did not meet criteria for oppositional defiant disorder or conduct disorder on any of the sociodemographic factors or family environment factors. A history of maternal incarceration was the only parental psychopathology variable that distinguished the children with oppositional defiant disorder or conduct disorder from the comparison subjects. Significant differences were found on several parenting factors, including rates of maternal stress, maternal report of mother-child verbal and physical aggression, and observed lack of maternal responsiveness. Two family risk factors distinguished preschool children with conduct disorder from children with oppositional defiant disorder: younger maternal age at the birth of the first child and absence of the father.
Thus, the risk profile for disruptive behavior disorders in preschool children appears to be similar to that for older children. Infant characteristics and parenting factors were identified as the strongest correlates of oppositional defiant disorder and conduct disorder, relative to the other primary domains of risk measured in the study, especially in samples of children living in predominately low-income environments.
Predictive Validity
Predictive validity, the extent to which a measured construct demonstrates a predictive relation to the same or a similarly measured construct
(23), has been tested in two longitudinal studies. Speltz et al.
(17) examined the 2-year diagnostic stability of oppositional defiant disorder in a sample of 92 preschool boys. The vast majority of the children (76%) continued to have oppositional defiant disorder, oppositional defiant disorder plus ADHD, or ADHD alone. Conduct disorder was rare in this group (3%). The authors raised the possibility that oppositional defiant disorder in preschool children may not be a stepping-stone to conduct disorder, as has been documented for older children
(25). The question of the longitudinal course of oppositional defiant disorder, which has clear implications for the etiology of conduct disorder, needs to be tested empirically in a more diverse sample.
Lavigne et al.
(26) reported that the stability of disruptive behavior disorders (defined as oppositional defiant disorder, conduct disorder, ADHD, or a combination of those disorders) from baseline to follow-up (an average of 2 years later) was moderate. Fifty percent of 2–3-year-old children and 65% of 4–5-year-old children with a baseline diagnosis of disruptive behavior disorder had a disruptive behavior disorder diagnosis at follow-up. However, no data were reported for separate diagnostic categories. The majority of children with a disruptive behavior disorder diagnosis had oppositional defiant disorder (82%).
The results of these two studies provide preliminary evidence that DSM-based disruptive behavior disorders can persist into school age. In addition, a substantial body of literature supports the persistence of a broad range of problem behavior, including temperamental difficultness and aggression, from as early as toddlerhood to school age
(27). What remains to be tested is whether there is specificity of prediction to school age for both DSM oppositional defiant disorder and conduct disorder in preschool children in clinic-referred and nonreferred study groups that include both sexes and that are ethnically and sociodemographically diverse.
Agenda for Future Research
Converging evidence suggests that preschool children manifest clinically significant disruptive behavior problems and that a DSM-based diagnostic framework has the potential to generate clinically and scientifically meaningful data about disruptive behaviors in this age group. The existing studies are all limited in their ability to provide evidence for the validity of oppositional defiant disorder and conduct disorder in preschool children. Only one program of research tested the convergent validity of oppositional defiant disorder and conduct disorder separately. Most researchers have tended to combine oppositional defiant disorder and conduct disorder in their analyses or even combine the disruptive behavior disorders and attention deficit disorders. In addition, given the small number of studies, little attention has been paid to differences in the diagnostic validity of oppositional defiant disorder and conduct disorder between the sexes and among ethnic and sociodemographic groups. Finally, except for the work of Lavigne and colleagues
(20, 26), studies of preschool oppositional defiant disorder and conduct disorder have been limited to clinic-referred samples. Testing the validity of the disruptive behavior disorders in clinic-referred samples is a reasonable first step, but once oppositional defiant disorder and conduct disorder have been validated as clinically meaningful constructs, their validity will need to be tested in a larger, community-based study.
In addition to the issues of sample limitations and the lack of specificity of the diagnoses of oppositional defiant disorder and conduct disorder, several issues related to the developmental level of preschool children must be addressed before further research testing the validity of these diagnoses in this age group is conducted. These issues include the need to test systematically the developmental modifications of the symptom criteria, to develop more clinically sensitive observational methods, and to assess children’s developmental level.
Standardizing Developmental Modifications
The majority of the studies reviewed here used structured or semistructured DSM-based interviews that were designed for school-age children and adolescents. Demonstrating that standardized psychiatric interviewing methods can be reliably used for preschool populations has been an important preliminary step. However, nonstandardized modifications of assessment instruments appear to have been used to address the lack of face validity and to establish the clinical significance for many symptoms, particularly for conduct disorder symptoms, such as “use of a weapon.” The studies typically present few or no data on how they assessed oppositional defiant disorder or conduct disorder symptoms in preschool children.
Thus, the development and validation of standardized modifications is a critical next step for the validation of behavior disorders in preschool children specifically and early childhood psychopathology in general. Developmental modifications must be designed to enable the systematic gathering of data that can be used to establish thresholds of clinical significance during the preschool period and to identify the functional equivalence of preschool manifestations of particular symptoms. Since the clinical significance of the symptoms of oppositional defiant disorder and conduct disorder during this period does not merely rest on the presence or absence of a specific behavior, both qualitative and quantitative aspects of the behavior must be assessed to establish symptom thresholds. Additional research is needed to systematically assess dimensions, such as frequency, severity, and pervasiveness to develop empirically based thresholds.
Observational Methods
There is no lack of developmentally appropriate rating scales for testing content validity, including the Child Behavior Checklist, Eyberg Child Behavior Inventory, Children’s Global Assessment Scale, and other reliable and valid measures of preschool children’s functioning at school and with peers. However, observational methods for establishing content validity have not been fully explored. Observations of the child both within and outside of the parent-child context may be particularly useful for differentiating problems in parenting from disordered child behavior
(28). Thus, standardized observations of child behavior must be included in future validation studies.
Several investigators have incorporated observations of parent-child tasks into their assessments of oppositional defiant disorder and conduct disorder in preschool children
(1, 16). In general, the tasks were originally designed to document normative changes in development. As such, these methods have yielded broadly relevant information (e.g., ratings of noncompliance), but they do not appear to be adequately discriminative. Thus, there is a need for standardized observational methods designed specifically to quantify fine-grained manifestations of disruptive behavior in preschool children (e.g., ignoring, defiance, provocation), as well as qualitative dimensions of behavioral dysregulation (e.g., intensity, rate of escalation, lability). Such methods are likely to enhance the diagnostic utility of methods that use parental reports, both in terms of discriminative validity and assessment of the degree of impairment.
Assessing Developmental Level
Assessing symptoms in the context of the child’s developmental level, while important at any age, is particularly key in making valid diagnoses in the preschool years because many relevant skills emerge during this period and the pace of their emergence varies widely among children
(29). We propose that a standardized developmental assessment is necessary in any study of the validity of disruptive behavior disorders in preschool children. The child’s comprehension of social rules is fundamental to establishing the clinical significance of many symptoms of disruptive behavior disorders, particularly conduct disorder, in which many behaviors (e.g., stealing, lying) are considered symptoms only if they involve “deliberate rule violation.” Clearly, for the child to meet criteria for such symptoms, it must be established that the child
understands the concept of rules in general and
intentionally broke the rules. Consideration of the child’s levels of language ability and social awareness is fundamental to establishing intentionality. Similarly, children cannot lie or be argumentative if they have not yet developed phrase speech. Routine assessment of language ability in validation studies will provide empirical data for establishing specific developmental thresholds.
Conclusions
Can valid diagnoses of DSM oppositional defiant disorder and conduct disorder be made in preschool children? The evidence we reviewed indicates that they can. Typical and atypical behavior problems can be differentiated in the preschool period, and the DSM framework, with some adaptation to account for the child’s developmental level, can be used effectively to identify children whose disruptive behavior is impairing. However, an affirmative response must be qualified because much of the evidence has been derived from study groups that combine subjects with oppositional defiant disorder and conduct disorder or with oppositional defiant disorder, conduct disorder, and ADHD. The diagnostic validity of conduct disorder in preschool children is still unclear.
Whether the behaviors associated with oppositional defiant disorder and conduct disorder that are measured in preschool children are functionally equivalent to those measured in school-age children is not yet known. Establishing functional equivalence will be a critical component of future efforts to valid these diagnoses in preschool children. We believe that continued testing of the validity of a DSM-based approach is a fruitful method for identifying clinically significant behavior problems early in life and linking them meaningfully to disruptive behavior disorders in older children. Moreover, a valid diagnostic system that extends to the preschool period would provide a framework for generating information that is critical for mental health research and service delivery, including the prevalence of impairing disorders in young children, the factors associated with onset, and the data needed to design approaches to prevention based on developmental level.
The efficacy of treatment for disruptive behavior disorders will be enhanced by addressing treatment efforts to the earliest manifestation of the disorders, not only because the early behavior may be more malleable, but also because secondary deficits and impairments have not yet been accumulated. Thus, establishing reliable and valid methods for identifying the phenotypes of oppositional defiant disorder and conduct disorder in preschool children will be essential to the implementation of established and developing interventions. Such interventions are likely to include ways of identifying vulnerabilities that precede the manifestation of psychopathology. For psychiatry to continue exploring methods for identifying genetic risk and the environmental profiles that exacerbate underlying genetic risk, developmentally informed nosologic systems that capture atypical behavior early in life must be established.