A growing number of studies have reported disparities in the quality of medical care received by African American patients, showing that they are less likely to receive standard tests and therapies for a broad range of conditions. These differences persist after controlling for insurance status and severity of illness
(1–
4).
In the mental health field, little research on quality issues and ethnicity has been done, partly because standard treatment protocols have only recently been developed
(5). However, previous studies have shown ethnic disparities in access to and intensity of mental health care. Among those with private insurance (and public insurance, albeit to a lesser extent), African American individuals are less likely than Caucasian individuals to use outpatient mental health services
(6–
8). With respect to intensity and type of care, African American individuals tend to have more emergency room visits but fewer outpatient visits than do Caucasian individuals
(9–
12).
One area in which quality of care for persons with serious mental illness can be examined is psychotropic prescribing patterns in the treatment of disorders for which standards have been developed. Over the past 10 years, atypical antipsychotic medications such as clozapine, risperidone, olanzapine, and quetiapine have been introduced in the U.S. market and are proving to be efficacious in reducing extrapyramidal side effects
(13–
16), which remain a major concern for long-term pharmacotherapy in individuals with schizophrenia
(17). Although not conclusive, studies have suggested that the newer antipsychotic medications have better outcomes than typical antipsychotics in reducing the negative symptoms and cognitive impairments associated with schizophrenia
(18–
21). A consensus has been built recommending the use of atypical antipsychotics in the treatment of first episodes and in cases of relapse
(22,
23). The exception is clozapine, which is used primarily for treatment-resistant cases of schizophrenia because of the risk of potentially fatal agranulocytosis
(24,
25).
Several studies have reported on ethnic disparities in psychotropic prescription patterns. On the basis of recommendations from the Schizophrenia Patient Outcomes Research Team study
(26), antipsychotic treatment conformance was examined in a random sample of patients diagnosed with schizophrenia. The rate of antipsychotic treatment ranged from 89% for inpatients to 92% for outpatients. Antipsychotic prescription rates were found to be similar for African American and Caucasian subjects; however, African American patients were more likely than Caucasian patients to receive higher antipsychotic doses and were less likely to be prescribed antidepressants despite having a similar level of depressive symptoms. Differences between atypical and typical antipsychotics were not examined, since the newer atypical antipsychotics were not on the market during the study period.
In other studies, African American patients have been found to have a higher likelihood of receiving depot antipsychotic medication at inpatient settings
(27), emergency rooms
(28), and outpatient settings
(29). A 1997 APA Practice Research Network study
(30) found that after demographic characteristics, education level, and source of payment were controlled, non-Caucasian patients were less likely to receive newer antipsychotic medications (risperidone or olanzapine). However, the study group size was small (N=146) and did not allow the authors to identify other factors that might have explained variation in medication practice patterns between ethnic groups. A recent study that examined trends in antipsychotic prescriptions for a large group of patients with schizophrenia (unpublished 2001 study of A. Rothbard et al.) confirmed findings from the Wang et al. study
(30) that African American clients were less likely to receive newer antipsychotic medications. The current study examines the extent and type of variation in antipsychotic prescription patterns for patients with schizophrenia as it relates to race and identifies a host of patient demographic characteristics, service utilization patterns, and provider characteristics that may explain the variation.
Method
Subjects were adult Medicaid recipients 18–64 years of age (N=2,515) who were treated for schizophrenia in 1995 with an antipsychotic medication. Medicaid recipients provide an excellent population group to study with respect to mental health treatment and disparity issues, since all study subjects are of similar socioeconomic status and receive comparable insurance benefits through the fee-for-service Medicaid program (which had no formulary restrictions in pharmacy benefits). Also, Medicaid provides medical benefits for a large number of African American individuals (e.g., 25% of African American respondents in the 1996 National Medical Expenditure Survey [6] had Medicaid coverage versus 8% of Caucasian respondents). In addition, Medicaid provides medical benefits for many of those receiving disability (according to the 1994–1995 National Health Interview Survey of Disability
[31], 30% of adults with mental disability were enrolled in Medicaid).
Subjects with a diagnosis of schizophrenia who used a psychiatric service in a general hospital, specialty mental health service agency, or office-based practice site were identified by using mental health claims records. The first antipsychotic prescription filled in 1995 was considered the index event. To ensure the completeness of the service and prescription data, the study subjects were required to have continuous enrollment in the fee-for-service Medicaid program during the 12-month period following the index prescription. Data on service use and provider setting were also examined during that period.
Demographic characteristics and Medicaid eligibility status information for each patient were derived from Medicaid beneficiary records. Data on use of psychiatric, substance abuse, and health care services were obtained from service claims records, which indicate diagnosis, date of service, type of service, and type of provider for each service by patient. Filled prescription records were obtained from the pharmacy claims data files; these files contained demographic information as well as prescription date, medication type, dose, and national drug codes by patient and medication type. Generic names of medications were identified from the state Medicaid databases by using the national drug codes. Secondary claims data were used in all the analyses.
Antipsychotic medications were categorized as traditional (e.g., haloperidol, fluphenazine, thioridazine) versus atypical (clozapine, risperidone). Among traditional medications, depot antipsychotics (fluphenazine decanoate and haloperidol decanoate) were examined as a subcategory. With respect to atypical antipsychotics, clozapine was also singled out because of its specialized use patterns involving treatment-resistant patients. Olanzapine and quetiapine were not included, since they did not come on the market for broad use until after 1995. A dichotomous variable was created to identify receipt of antipsychotic medication monthly by type (i.e., clozapine, risperidone, traditional antipsychotics, and depot antipsychotics). A similar variable was constructed to denote monthly mental health service type (i.e., inpatient, intensive case management, partial hospitalization, emergency room service). Outpatient provider setting was operationalized according to the provider that the subject had the most frequent mental health contacts with during the study period. Specialty mental health provider settings were categorized as community mental health centers (CMHCs), hospital outpatient departments, other specialty mental health agencies, and office-based psychiatrists. If a subject had no contact with an ambulatory specialty mental health provider, the provider type assigned was one of the following, in the sequence listed: general physician, psychiatric hospital, or emergency room, in the sequence listed. Thus, if patients had no specialty provider but a general physician visit during the study period, they were assigned the physician provider type regardless of whether they had a psychiatric hospital or emergency room contact. This was done to identify their ambulatory provider type, which was the variable of greater interest.
Antipsychotic prescription patterns for Caucasian and African American subjects were compared by using both univariate and multivariate analysis. The percentage of subjects prescribed antipsychotics by racial group was examined by type of medication, duration of the initial treatment, and receipt of depot antipsychotics. To identify possible explanatory variables of prescription patterns, a series of univariate analyses was carried out on demographic characteristics, service use, and provider setting. Chi-square tests for categorical variables and t tests for numerical variables were employed.
The study hypothesis was that an analysis of prescription patterns in which other influences were controlled would show that variation in prescription of atypical antipsychotics was influenced by race. A multivariate logit analysis was employed to test the effect of ethnic membership on the likelihood of receiving either clozapine or risperidone during the follow-up year, with demographic and service use characteristics as control variables. Service use variables were coded as 1 for subjects who received each type of service (e.g., psychiatric inpatient, emergency room visit, intensive case management, etc.) during the follow-up year. Dichotomous variables indicating female gender and receipt of Supplemental Security Income (SSI) were entered as well in the logit model. A four-category age variable was created that coded age ranges as 1 (ages 18–30), 2 (ages 31–40), 3 (ages 41–50), or 4 (ages 51–64).
Results
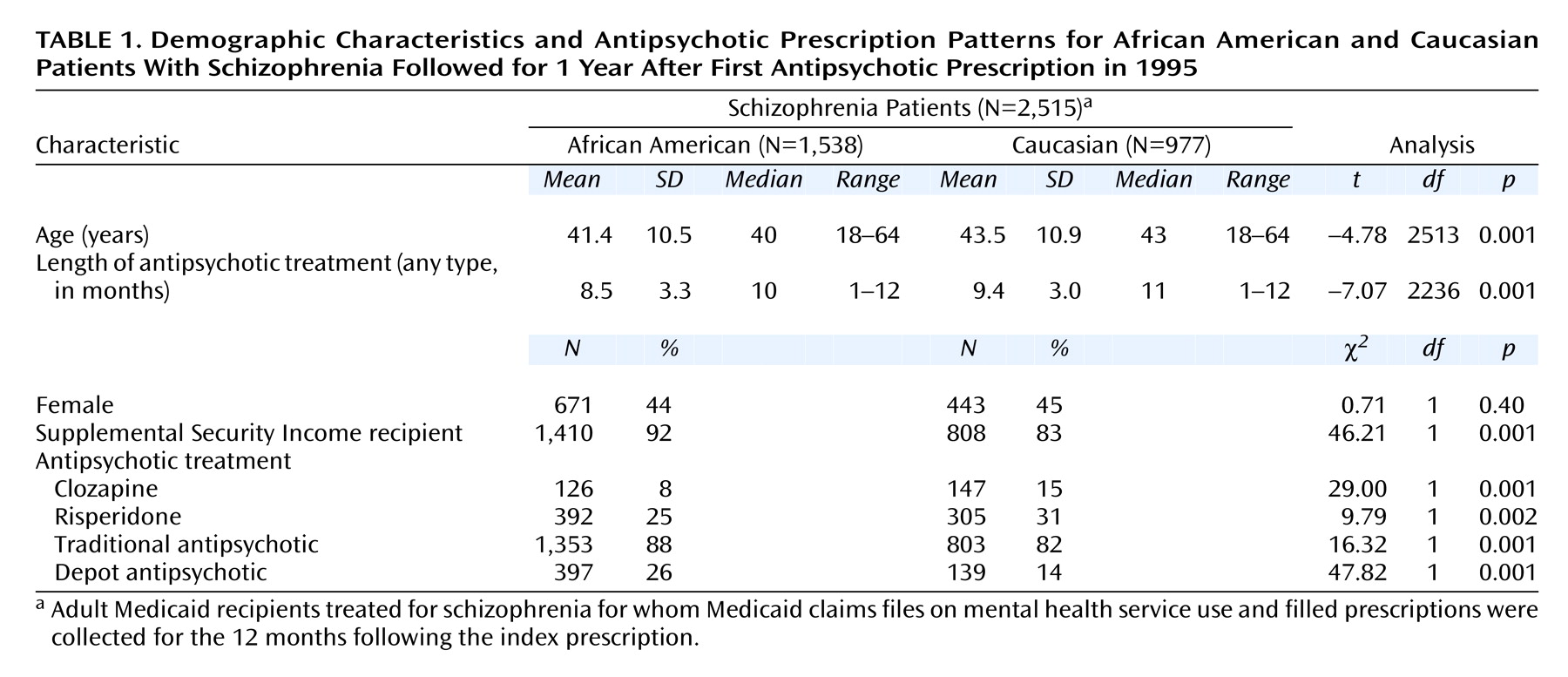
The demographic characteristics and antipsychotic prescription patterns of the 2,515 study subjects are presented in
Table 1. Sixty-one percent of the subjects were African American, and 39% were Caucasian. African American subjects were significantly younger than the Caucasian subjects, and a significantly higher percentage of African Americans patients received SSI in the year following their index prescription (
Table 1).
Antipsychotic Prescription Patterns
Significant differences between African American and Caucasian subjects were also found in the type of prescription filled during the study period. Clozapine and risperidone were given more often to Caucasian subjects, whereas depot antipsychotics were given more often to African American subjects. In general, African American subjects were more likely to receive traditional antipsychotic medications. In terms of the number of months receiving any type of antipsychotic medication, African American subjects had significantly shorter treatment durations than did Caucasian subjects (
Table 1).
Service Use Characteristics
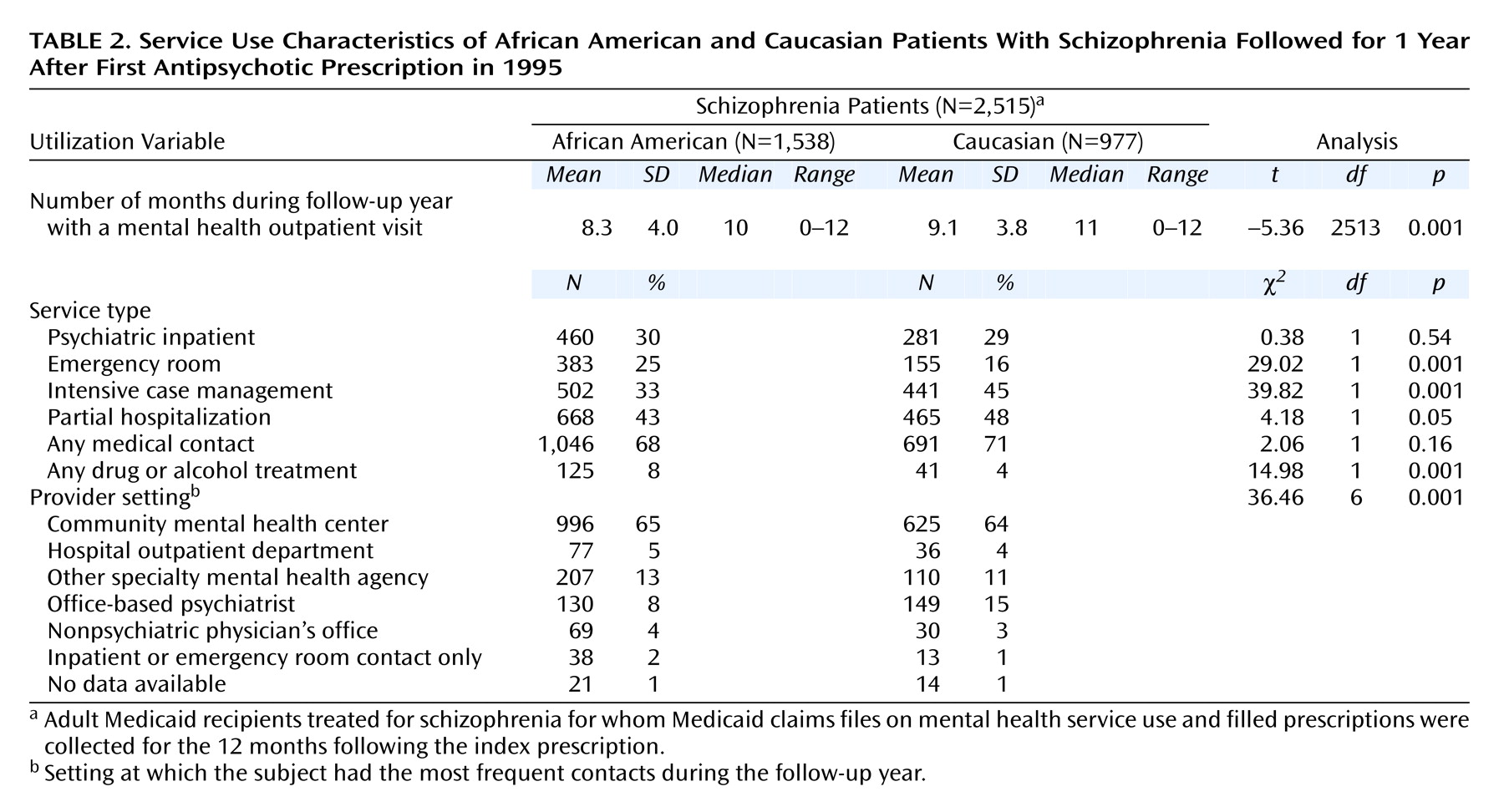
As seen in
Table 2, significant differences were seen in mental health service use, with Caucasian subjects receiving mental health services more often and over a longer time period than African American subjects. Service type differed as well, with African American patients less likely than Caucasian patients to receive intensive case management or partial hospitalization and more likely to have an emergency room contact (
Table 2). These patterns, consistent with previous reports on differential service use patterns between African American and Caucasian subjects
(9–
12), indicate that African American subjects are not as engaged in the more continuous and intensive type of services associated with persistent mental health problems.
Prescription Patterns by Provider Setting
Mental health provider setting was also found to differ by ethnic group (
Table 2). In general, subjects had the most frequent contact with CMHC providers. Similar percentages of African American and Caucasian patients used hospital outpatient departments and other specialty mental health agencies, but 15% of Caucasian subjects had their most frequent contact with an office-based psychiatrist (compared with only 8% of African American subjects).
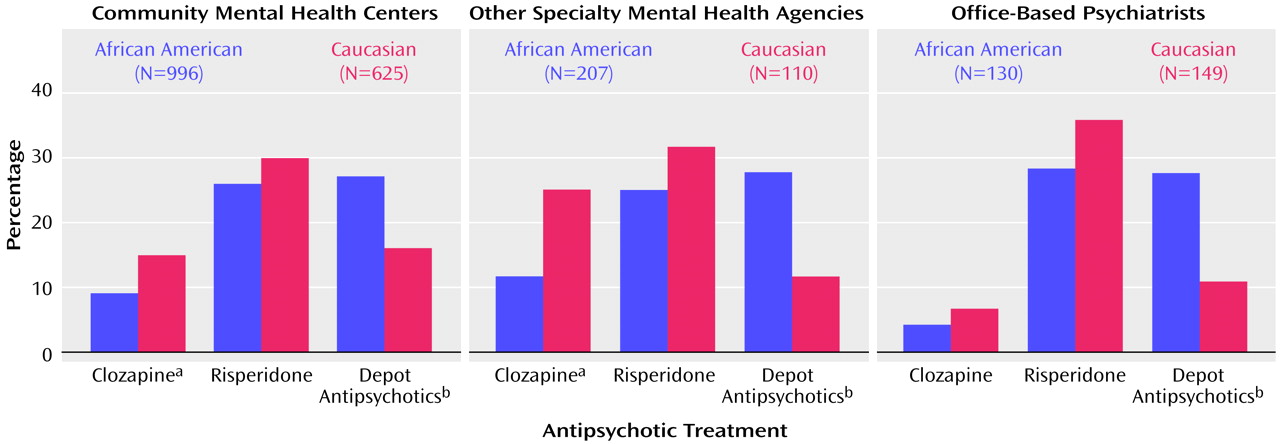
Figure 1 shows the relationship between prescription type (clozapine, risperidone, depot antipsychotic) and provider setting (CMHC, specialty mental health agency, office-based psychiatrist) by ethnic group. The analysis was done to ascertain if the racial differences in the prescription rates of clozapine, risperidone, and depot antipsychotics found in
Table 1 were associated with provider setting. The results showed that across all provider settings, African American subjects were less likely to receive clozapine and risperidone and were significantly more likely to receive depot antipsychotics, but the differences by provider setting were not statistically significant.
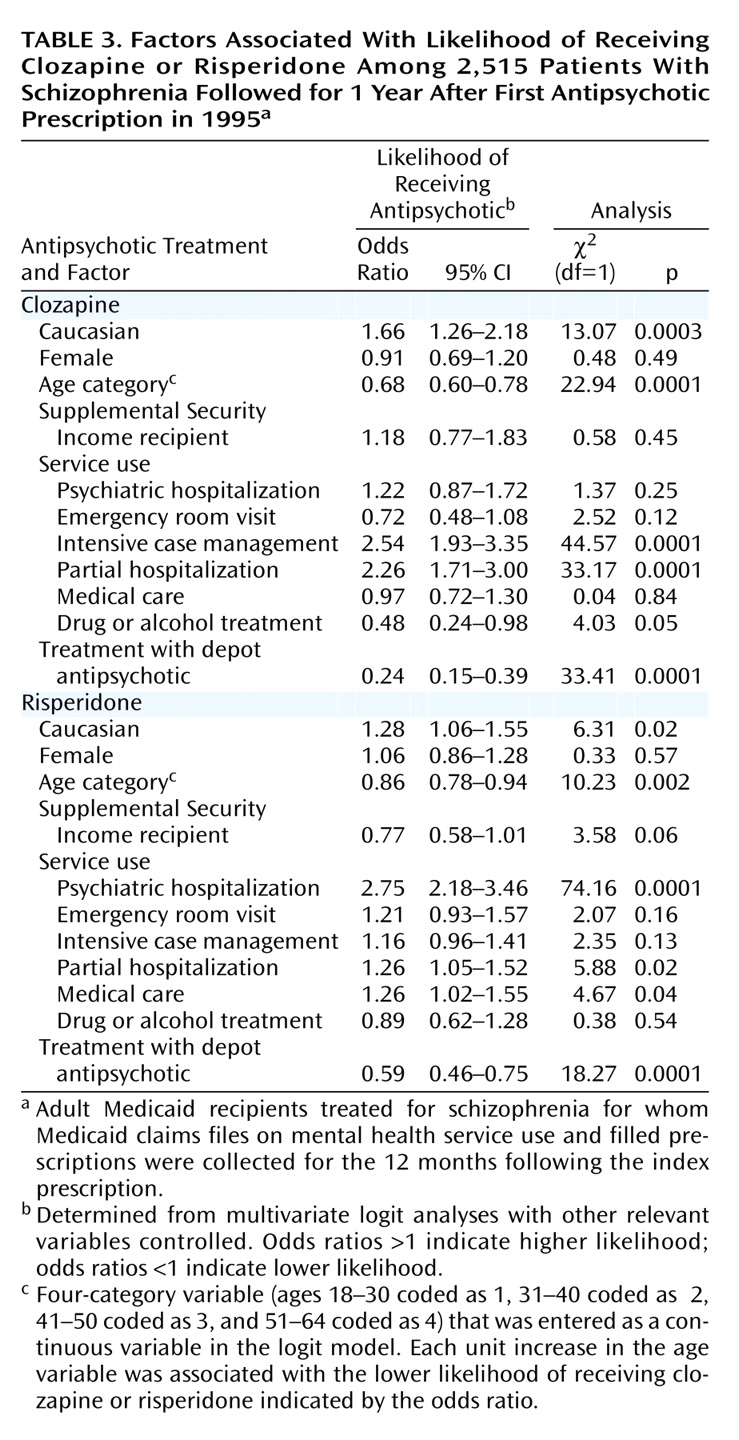
Multivariate Analyses
The results from the logit analyses are presented in
Table 3. The dependent variable for the first model was whether a client received clozapine during the year following their index prescription, and the second model examined the use of risperidone. Dichotomous variables indicating whether subjects received SSI; underwent psychiatric hospitalization or an emergency room visit; or received intensive case management, partial hospitalization, drug or alcohol treatment, any medical care service, or a depot antipsychotic during the follow-up year were entered as control variables in both models, as were gender and age category.
As in the univariate analysis, Caucasian subjects were still significantly more likely to receive clozapine than African American subjects after we controlled for other relevant variables. Several variables significantly related to lower likelihood of receiving clozapine included older age, having received depot antipsychotics, and having received drug or alcohol treatment. Receiving intensive case management or partial hospitalization were related to higher likelihood of receiving clozapine (
Table 3).
After demographic and service use characteristics were controlled, ethnic membership was also a significant factor in receiving risperidone. Caucasian subjects had a higher likelihood of receiving risperidone compared with African American subjects. Subjects who received a depot antipsychotic during the year were significantly less likely to have received risperidone, as were older subjects. Other factors associated with having a higher likelihood of receiving risperidone included psychiatric hospital admission, partial hospitalization, and medical care contact (
Table 3).
Discussion
Consistent with prior studies that have shown differential treatment patterns by race for mental health services, this study found ethnic disparities in antipsychotic prescription patterns among a large number of publicly insured clients treated for schizophrenia. The study subjects were continuously enrolled in Medicaid, which controls for equal reimbursement opportunities. The results show that African American subjects were less likely to receive atypical antipsychotic medications after controlling for the difference in the percentage of subjects receiving SSI income support (which can be used as a proxy for chronic and persistent mental health problems) and the differences in service use characteristics. The odds ratios for the higher rate of Caucasians receiving clozapine (1.66) and risperidone (1.28) indicate a small effect size
(32). Nonetheless, implications and reasons for these discrepancies require further inquiry to ensure equal quality of care for vulnerable populations.
One of the limitations of this study is the lack of clinical information at the time subjects received their medication, which limits our ability to explain the disparity, particularly if clinical symptoms differed between African American and Caucasian clients. This information would allow us to assess if disparities in the likelihood of receiving atypical antipsychotics continue to exist for those with similar clinical features (i.e., presenting symptoms, past treatment response, side effects, medical and substance abuse comorbidity, and history of medication noncompliance). A pilot study is currently in progress to assess clinical symptoms at the time of prescribing.
The disparity in use of clozapine in African American patients is of special concern because of the favorable outcomes clozapine has had for patients with refractory schizophrenia. A special feature of clozapine treatment is a requirement of weekly leukocyte counts to monitor the risk of agranulocytosis. Although to our knowledge no supporting empirical data have been found, it can be speculated that clinicians may think that African American clients are more likely to be noncompliant with the regular monitoring procedures and hesitate to switch African American patients to clozapine. Also, Lawson
(33) has reported that the normal leukocyte range of African American patients can extend well below the normal laboratory value range. Thus, overly cautious clinicians may choose not to give otherwise physically healthy African American patients a medication with such a risk.
The fact that a higher percentage of Caucasian subjects saw office-based psychiatrists may have accounted for some of the variation in higher risperidone prescription rates. However, the majority of study subjects were treated at CMHCs and other specialty mental health agencies at which similar disparities in prescription patterns between African American and Caucasian subjects were found. These agencies generally have several psychiatrists doing medication evaluations.
Given the study findings, it is of great importance to examine factors associated with provider and patient characteristics that lead to decisions regarding switching from traditional to newer types of atypical medications as well as choosing atypical antipsychotics as the initial pharmacological treatment, as recommended by practice guidelines
(22,
23). Practice variations may exist at the individual provider level within an agency as well as between the CMHCs because of variability in provider skills, knowledge, and preference as well as variability in patient attitude and practice context (e.g., time spent in treatment, length and quality of client-clinician relationship). Clinician decisions may also be affected by demanding family members and activists
(34) as well as by preference of clients. Pharmaceutical marketing strategies by geographical area may also affect physician decision making. Unfortunately, Medicaid claims do not identify individual providers in specialty clinic settings or tell us about preference and practice context, marketing strategies, and other exogenous factors that affect both clinicians and patients.
It is important to note that olanzapine and quetiapine were not examined in this study because they were introduced in the U.S. market after the study period. Another atypical medication, ziprasidone, was approved by the Food and Drug Administration in early 2001. Given the rapidly changing pharmacological treatment environment, our study findings on ethnic disparities have significant implications for differential quality of care for African American and Caucasian patients with schizophrenia. Although administrative databases like Medicaid are extremely useful in identifying trends and differential prescription patterns of large numbers of patients in naturalistic settings, future studies employing patient and provider characteristics are urgently needed to test alternative explanations for ethnic disparities. Answers to these questions can lead to intervention strategies that will result in better quality of care.