There have been consistent reports of a greater incidence of schizophrenia among certain immigrant groups to Western Europe (1). These groups include, among others, first- and second-generation Caribbean immigrants to the United Kingdom (2), first- and second-generation Surinamese and Moroccan immigrants to the Netherlands (3, 4), and East African immigrants to Sweden (5). According to the Norwegian psychiatrist Ødegaard (6), reports of a higher incidence of schizophrenia among migrants is explained by selective migration of people who are genetically predisposed to develop the disorder. In 1932 he examined the biographies of Norwegian immigrants who had developed schizophrenia in the United States. Impressed by their histories of poor social adaptation in Norway, he reasoned that these patients would have also developed the disorder had they stayed in their home country.
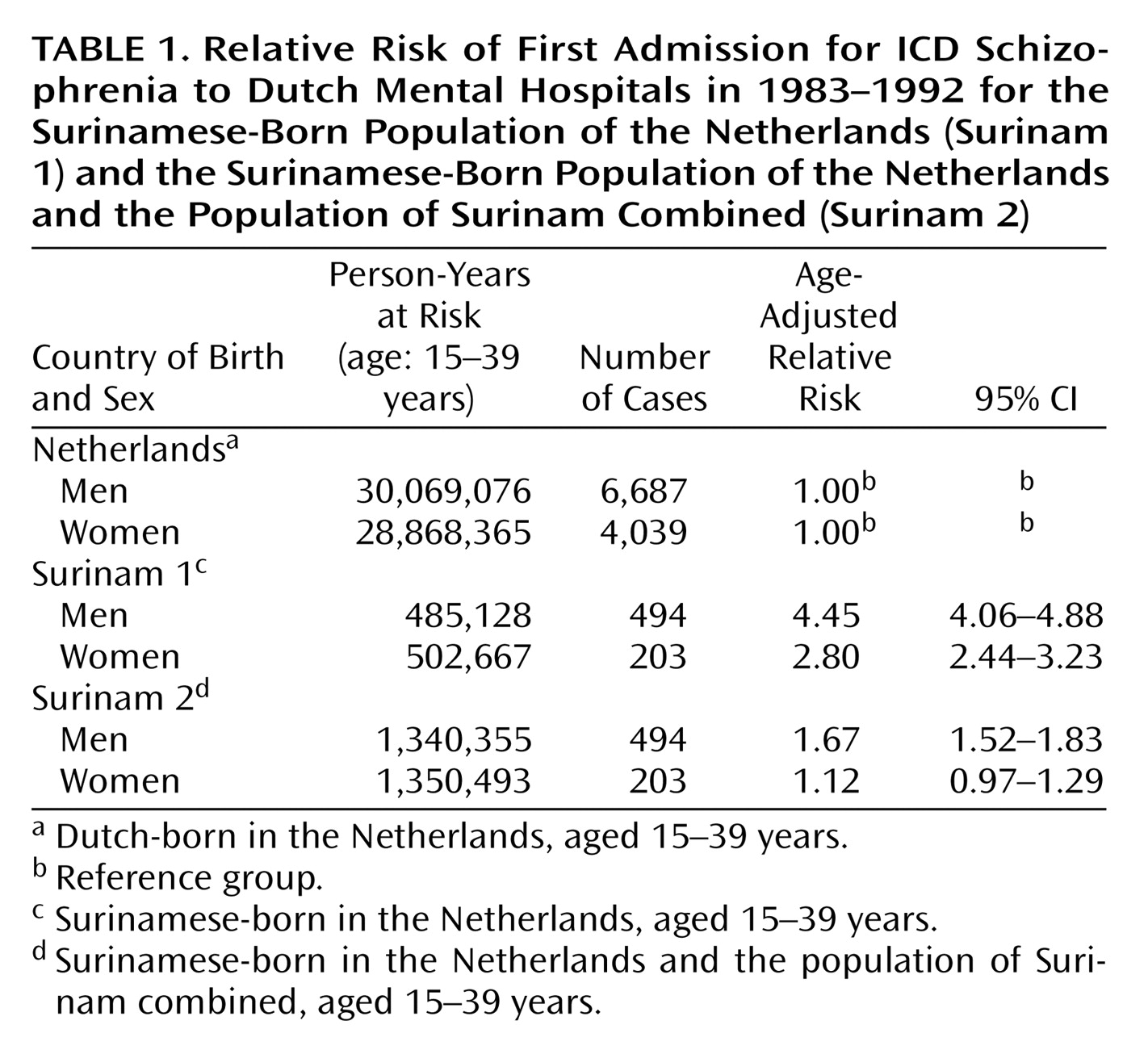
The Dutch colony of Surinam gained independence in 1975, and doubts about the future caused more than one-third of its population to migrate to the Netherlands, particularly during the periods 1971–1975 and 1979–1981 (7). In a study of the Dutch psychiatric registry (3), we found that the risk of a first psychiatric hospital admission for schizophrenia for male immigrants from Surinam was four to five times higher than that for their Dutch-born peers and that the risk for female immigrants was two to three times higher. A first-contact study of incidence showed that these findings were not due to misdiagnosis or to a lower threshold for hospital admission (4).
The Bureau for Statistics in Surinam makes available yearly population data; this enabled us to test Ødegaard’s hypothesis with a thought experiment. We imagined that the entire population of Surinam had emigrated to the Netherlands and that all the hypothetical additional migrants, consisting of those who in reality had stayed behind, contributed to the Netherlands no new cases of schizophrenia. We repeated the study of the Dutch psychiatric registry and enlarged the denominator for the Surinamese-born population by adding the entire age-correspondent resident population of Surinam during the years in question. We reasoned that the selection hypothesis could be rejected if the risk of schizophrenia for Surinamese-born people remained significantly higher, because this enlargement precluded any possibility of selection.
Method
The Dutch psychiatric registry provided data for all Dutch- and Surinamese-born patients who had been discharged with an ICD-8 or, after 1978, an ICD-9 diagnosis of schizophrenia in the period 1970–1992.
The Bureau for Statistics in the Netherlands provided yearly totals for the Surinamese- and Dutch-born populations in the Netherlands, stratified by sex and 5-year age categories. The Bureau for Statistics in Paramaribo, Surinam, provided corresponding data for the population of Surinam. The yearly figures for Surinam are based on the 1980 census and on subsequent counts of live births, deaths, emigrants, and immigrants. The 1980 census showed that the previous counts by this bureau had been highly reliable: the census reported a total of 355,240 inhabitants of Surinam; the bureau gave the total as 355,252. According to information from the bureau, the counting methods after 1980, if anything, have only improved. As some individuals who migrate from Surinam to the Netherlands do not report their emigration to the authorities in Surinam, the bureau collaborates closely with the Bureau for Statistics in the Netherlands.
We calculated the risk of a first hospital admission for schizophrenia over the 10-year period (1983–1992) by dividing the number of patients by the number of person-years. We divided patients into 5-year age groups according to age at relevant admission, not at discharge, and confined our analyses to persons aged 15–39 years. We derived person-years at risk for schizophrenia during the 10-year period by adding the yearly population figures. For the Surinamese-born group, this was done by adding the person-years contributed by the populations of the Netherlands and of Surinam. We compared the risk for each sex and 5-year age category in the Surinamese-born group to that for the corresponding category in the native-born group. Sex- and age-adjusted relative risks were calculated by Poisson regression analysis.
Results
The age- and sex-adjusted relative risk for Surinamese-born individuals was calculated as 1.46 (95% confidence interval [CI]=1.35–1.57). When the results were considered separately for men and women, the age-adjusted relative risk was significantly higher for men but not for women (
Table 1).
Discussion
After enlargement of the denominator by adding the resident population of Surinam, the risk of a first hospital admission for schizophrenia among immigrants from Surinam remained significantly higher than that for their Dutch-born peers. Consequently, it is highly unlikely that negative selection is the sole explanation for the higher incidence of schizophrenia in these immigrants.
This conclusion is supported by the observation that not all people who carry genes predisposing them to schizophrenia migrated from Surinam to the Netherlands. A study at one of three outpatient clinics in Surinam (8) found 144 first contacts for psychosis in the period 1984–1990. The mean annual rate of first admissions for schizophrenia or schizophreniform disorder (DSM-III-R criteria) in 1992 and 1993 was found to be 1.61 per 10,000 among people aged 15–54, which falls within expected norms from other studies (9). If the greater incidence of schizophrenia in the migrants was due to selective migration, one would expect that the gene pool for schizophrenia among the population remaining in Surinam would be significantly depleted and that the incidence of schizophrenia in Surinam would be very low.
One might speculate that the greater incidence of schizophrenia in Surinamese immigrants to the Netherlands is caused by mass emigration from a country with a greater prevalence of schizophrenia. However, there is no evidence of a higher incidence or prevalence of the disorder in Surinam or surrounding countries (10). Second, clinical experience and research findings demonstrate that most Surinamese immigrants who are treated in the Netherlands for schizophrenia developed the disorder in the Netherlands. Furthermore, the median age of migration of the patients who participated in the first-contact study of incidence in the Netherlands was 9 years (4). Finally, Bogers et al. (8) showed that subjects who had already developed a psychotic disorder in Surinam were significantly less likely to migrate to the Netherlands than others. We have no explanation for the somewhat different results for men and women in the present study. The literature does not point to a consistent sex difference in the risk of schizophrenia for immigrants (11).
One previous study directly tested Ødegaard’s hypothesis. Rosenthal et al. (12) compared the emigration rates for adopted children born to a biological parent with a schizophrenia spectrum disorder to the emigration rates for children born to nonschizophrenic parents and found that the rates for the first group were lower than those for the second.
We conclude that selection factors cannot entirely account for the greater incidence of schizophrenia among immigrants to the Netherlands from Surinam. Thus, questions remain concerning the nature of the putative underlying mechanism. A problem from the standpoint of a purely biological interpretation is the greater risk for schizophrenia for both first- and second-generation immigrants from this country (4). One could speculate, for instance, that the excess of schizophrenia among first-generation immigrants could be due to an impaired immunity to a neurotropic virus found in Western Europe. However, this hypothesis cannot readily explain the higher risk seen among second-generation immigrants, who are exposed to the same physical environment as their Dutch peers. It is more likely, therefore, that some experiences associated with the process of migration (e.g., breakdown of social bonds, racial discrimination), which are stressful for both generations, precipitate the disorder in those who are genetically at risk for psychoses. As such notions have yet to receive empirical confirmation, it may be too early to think in terms of possible intervention programs.