Although affective instability has come into increasing prominence in the personality disorder literature as a defining feature of borderline personality disorder, the nature of affective instability in patients with personality disorders has not been well studied. Affective instability was defined in DSM-III-R as “marked shifts from baseline mood to depression, irritability, or anxiety, usually lasting a few hours and only rarely more than a few days” (p. 347). DSM-IV modified the definition slightly, emphasizing that affective instability should reflect a marked reactivity of mood as well (p. 654).
Drawing upon parallels in the phenomenology of groups of axis I and axis II disorders as well as genetic and physiological data, Siever and Davis
(1) proposed that affective instability was a psychobiological dimension of personality disorders associated with borderline personality disorder. Recent studies of the neurochemistry of affective instability in personality disorder patients have added additional support to this hypothesis
(2). Nevertheless, in spite of its clinical prominence and theoretical significance, the phenomenology of affective instability in patients with personality disorders has not been well described.
Two studies have provided quantitative descriptions of affective instability in patients with borderline personality disorder. Cowdry et al.
(3) asked inpatients to rate their general mood twice a day. They found that patients with borderline personality disorder showed greater morning-to-evening mood variability and a more random distribution of morning moods than did patients with major depression or healthy comparison subjects. The second study
(4), which analyzed the day-to-day mood fluctuations of a group of healthy comparison subjects and a group of affectively unstable patients (most of whom met criteria for borderline personality disorder), found that although the affective variability in the comparison subjects was consistent with random fluctuations, the affective variability in the patients was nonrandom, possibly reflecting a systematic underlying process that determined the affective instability.
Understanding in greater detail the nature of affective instability in patients with personality disorders is important for a number of reasons. First, it is possible that some of these disorders might be characterized by rapidly shifting emotions, others by emotional intensity, and others by dyscontrol only of a specific emotion such as anger or depression. It is also not clear whether personality disorder patients with “affective instability” are unstable across all affects or only in selected ones
(5). Differences in which individual affects are unstable could potentially distinguish personality disorders. Better characterizing affective instability might also aid in differentiating bipolar spectrum disorders from affectively unstable personality disorders, lead to greater specificity in the pharmacotherapy of personality disorders, and generate a better understanding of the psychobiology of affective dyscontrol.
We carried out a study of the features of affective instability among a group of research patients with personality disorders. We hypothesized that patients with borderline personality disorder would demonstrate a greater and specific instability in moods that would correspond to the emotions specified in the DSM definition of affective instability (i.e., depression, anger, and anxiety) relative to patients without borderline personality disorder. In addition, we expected the patients with borderline personality disorder to have a greater subjective intensity of affective experience relative to patients without borderline personality disorder.
Results
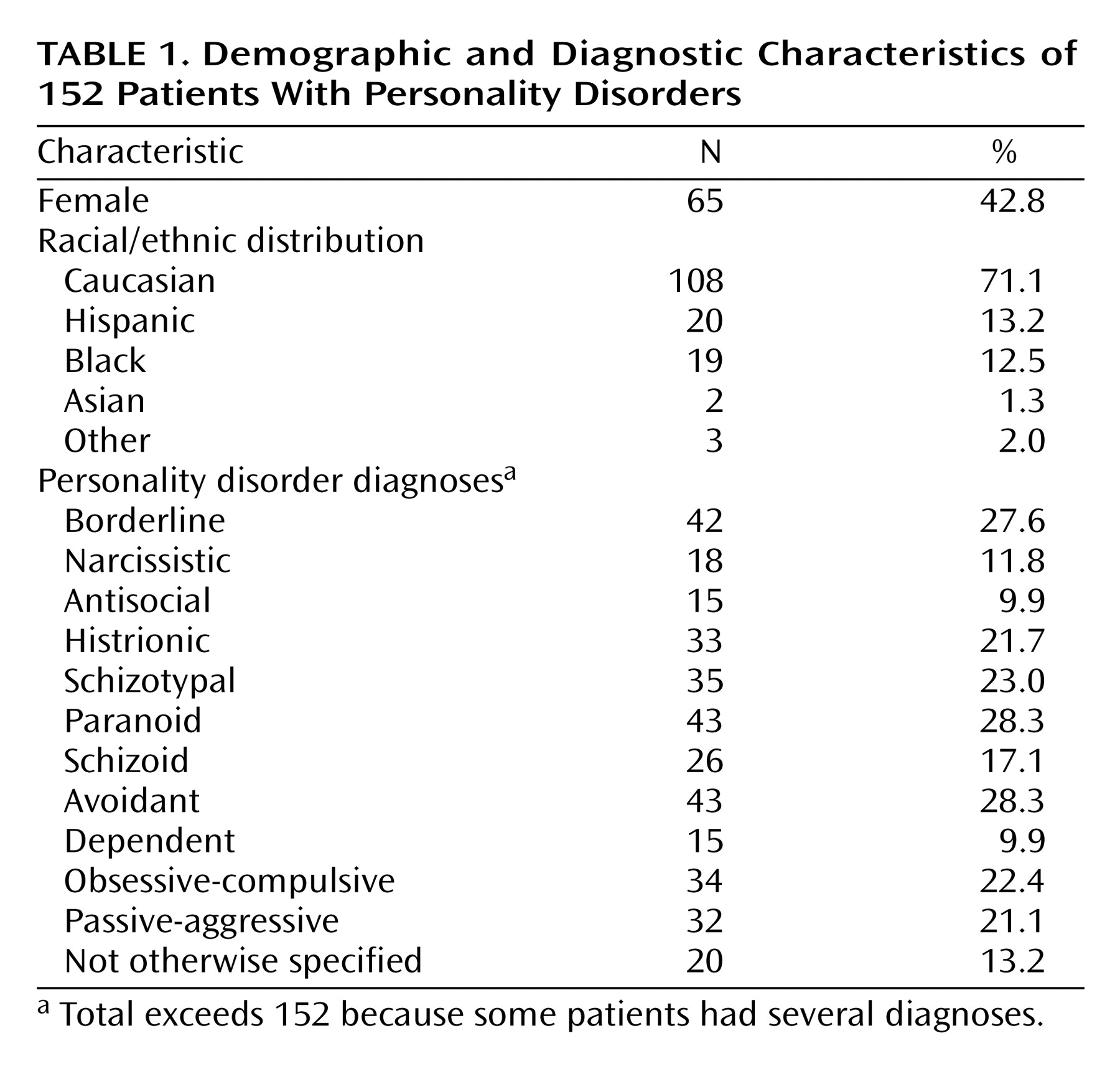
The mean age of the 152 patients was 37.6 years (SD=10.3), and the subjects had a mean of 2.3 (SD=1.5) personality disorders. Other demographic features of the study group and the frequencies of the individual personality disorder diagnoses are shown in
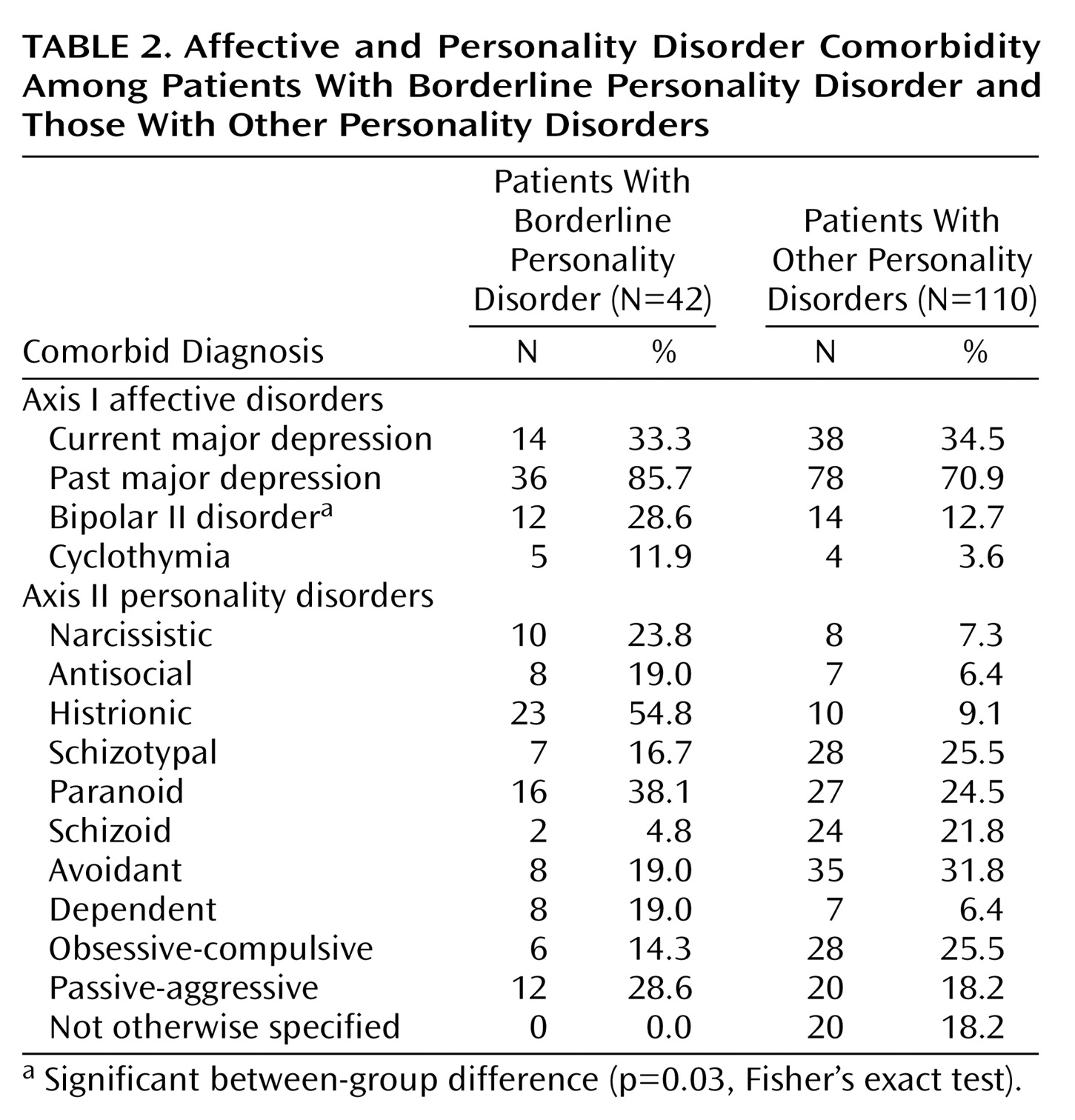
Table 1. A higher percentage of patients with borderline personality disorder (60%, N=25 of 42) than those with other personality disorders (37%, N=41 of 110) were female (p<0.02, Fisher’s exact test). The borderline personality disorder patients were younger (mean=34.0 years [SD=8.3] versus mean=39.0 [SD=10.6]; t=2.76, df=150, p=0.007) but did not differ in their ethnic composition. Data for the rate of current major depression, past major depression, bipolar II disorder, cyclothymia, and the other personality disorders in the patients with borderline personality disorder and those with other personality disorders are presented in
Table 2. Only the prevalence of bipolar II disorder differed significantly between the two groups (p=0.03, Fisher’s exact test). One-third of both the borderline personality disorder group and the other personality disorders group met criteria for major depression at the time of the study.
As a test of the validity of the Affective Lability Scale for this population, we calculated the correlation between the overall Affective Lability Scale score and the rating of affective instability by interviewers who used DSM-III-R criteria. The correlation was significant (rs=0.44, N=152, p<0.001). Affect Intensity Measure score was also significantly correlated with DSM-III-R affective instability (rs=0.40, N=152, p<0.001).
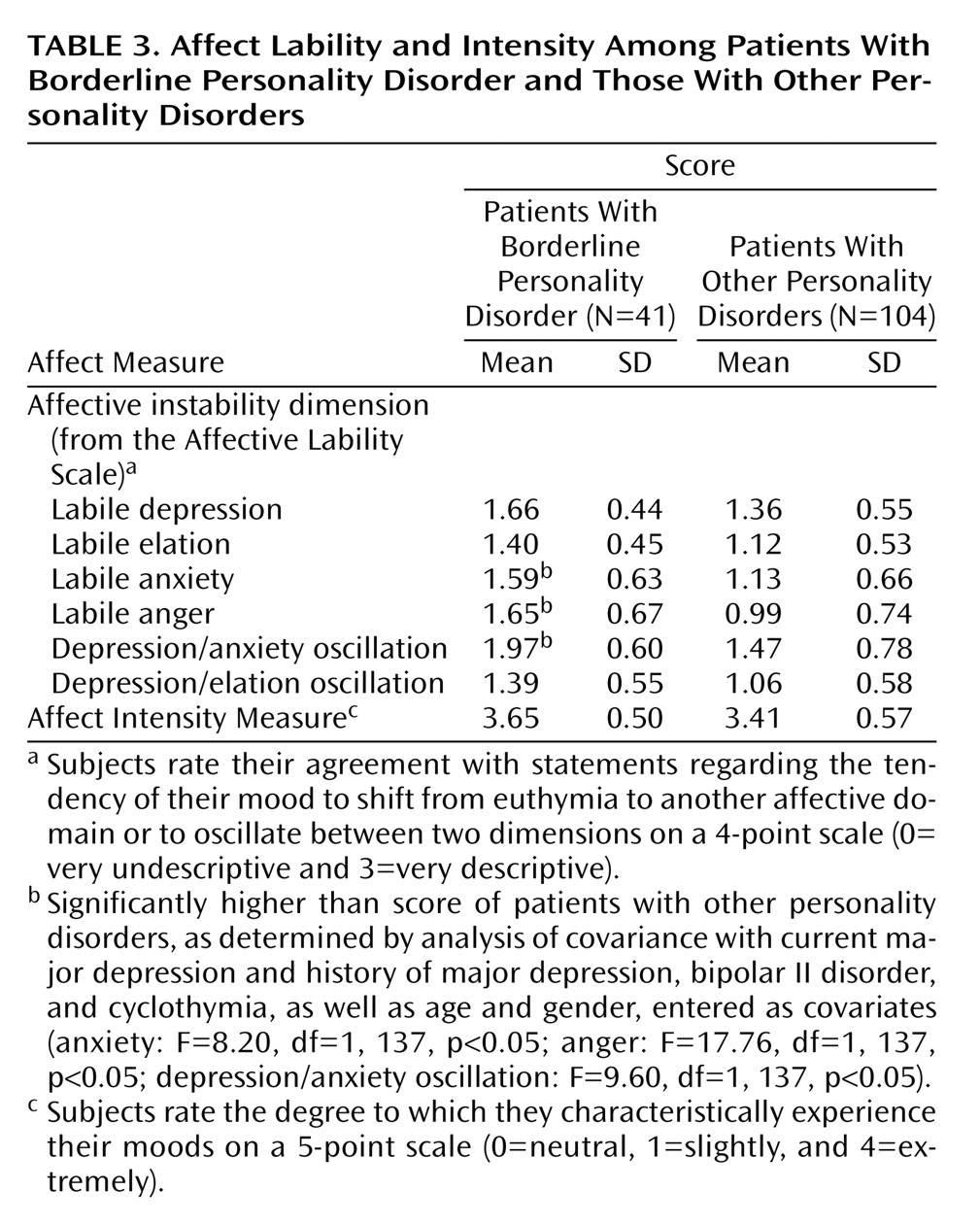
The mean scores on each of the Affective Lability Scale subscales and the Affect Intensity Measure for patients with borderline personality disorder and those with other personality disorders were compared by t tests. Differences were considered significant at the 0.05 level (the more conservative two-tailed value was used) because of our a priori hypothesis that patients with borderline personality disorder would score higher on three of the Affective Lability Scale subscales (depression, anger, and anxiety) and on the Affect Intensity Measure. Patients with borderline personality disorder had significantly higher scores on all the Affective Lability Scale subscales and on the Affect Intensity Measure (Affective Lability Scale subscales: all t>3.00, df=150, all p<0.004; Affect Intensity Measure: t=2.35, df=150, p=0.02). It is possible that since the patients with borderline personality disorder subjectively experienced their moods more intensely, their Affective Lability Scale ratings could be elevated for that reason. To rule out this possibility, separate analyses were carried out in which we entered Affect Intensity Measure score as a covariate in analyses of covariance for each Affective Lability Scale subscale comparing the patients with borderline personality disorder and those with other personality disorders. All Affective Lability Scale differences remained significant (all F>4.28, df=1, 149, all p<0.04). The covariate effect was also significant for each Affective Lability Scale (all F>6.99, df=1, 149, all p<0.009). The possible contribution of current major depression or past history of bipolar II disorder, cyclothymia, or major depression to the Affective Lability Scale and Affect Intensity Measure measures were next controlled by entering these diagnoses (as categorical variables) as covariates in a single analysis of covariance. The group differences for each Affective Lability Scale subscale and Affect Intensity Measure remained significant (all F>4.27, df=1, 139, all p<0.04), while significant covariate effects were seen for current major depression on depression/anxiety oscillation (F=8.72, df=1, 139, p=0.004), history of major depression on depression/anxiety oscillation (F=10.88, df=1, 139, p=0.001), and cyclothymia on both labile elation (F=5.08, df=1, 139, p<0.03) and depression/elation oscillation (F=8.92, df=1, 139, p=0.003). Finally, an analysis of covariance that compared borderline personality disorder patients with other personality disorder patients was carried out for each Affective Lability Scale subscale and the Affect Intensity Measure score, with the following variables entered as covariates: history of major depression, bipolar II disorder, or cyclothymia; current major depression; and gender (all entered as categorical variables) along with age. Seven of the 152 cases were not included in this analysis because of missing data. In this most conservative analysis, patients meeting criteria for borderline personality disorder reported significantly greater lability in terms of anger, anxiety, and oscillation between depression and anxiety (
Table 3). To determine whether there were gender differences in subscale scores within the borderline personality disorder group, male and female patients with borderline personality disorder were compared by t tests; there were no significant differences.
In order to determine the relative importance of these three Affective Lability Scale variables in the discrimination of patients with borderline personality disorder and those with other personality disorders, a forward entry discriminant functional analysis was employed. The three Affective Lability Scale variables were entered into the analysis, with only one of the variables entering the equation at a significant level. Labile anger significantly discriminated the two groups at the first step in the analysis (F=23.39, df=1, 143, p<0.001). Overall classification accuracy in diagnostic group (borderline personality disorder versus other personality disorder) was 72.4% with this equation, with 76% of the group with borderline personality disorder and 91% of the group with other personality disorders successfully classified.
In our study group, there was substantial comorbidity among personality disorders (mean=2.3, SD=1.5). To determine whether or not the presence of additional comorbid personality disorders accounted for the differences in the lability and intensity scores for the borderline personality disorder patients, we compared, by t tests, mean scores on the Affective Lability Scale subscales and the Affect Intensity Measure score between borderline personality disorder patients with and without comorbid cluster A (schizotypal, schizoid, or paranoid), cluster B (histrionic, narcissistic, antisocial), and cluster C (avoidant, dependent, obsessive-compulsive, passive-aggressive) personality disorder diagnoses. There was a significant difference in only one of the 21 t tests: borderline personality disorder patients with a cluster C diagnosis had a lower Affect Intensity Measure score than those without cluster C comorbidity (t=2.68, df=40, p=0.01). This one difference would not have been significant with the application of the Bonferroni correction.
Discussion
The affective instability characteristic of borderline personality disorder does not appear to involve all affects, nor is it explained simply by an increase in the subjective intensity of affective experience. When we controlled for the presence of other comorbid personality disorders, age, sex, and affective spectrum diagnoses of cyclothymia, bipolar II disorder, and past or current major depression, borderline personality disorder was associated with greater lability in terms of anger, anxiety, and oscillation between depression and anxiety. There was no significant difference between male and female borderline personality disorder patients in the Affective Lability Scale scores on these subscales. An association of borderline personality disorder with lability in these affect domains is consistent with the DSM-IV characterization of affective instability in borderline personality disorder, which specifies mood shifts from baseline to irritability, anxiety, and depression. While we found greater lability in terms of depression/anxiety oscillation, we did not find a significant association of borderline personality disorder with greater lability in terms of depression alone. This may be because controlling for the contribution of the affective spectrum disorders (cyclothymia, bipolar II disorder, and major depression) removed the effect. This conclusion is supported by the results of the analyses in which cyclothymia, bipolar II, and major depression were not controlled, where borderline personality disorder patients also demonstrated significantly greater lability in terms of depression, elation, and depression/elation oscillation. We have reported elsewhere
(12) that bipolar II disorder in this study group was associated with greater lability in terms of depression, elation, and depression/elation oscillation than was borderline personality disorder. Among the three Affective Lability Scale subscales associated with a borderline personality disorder diagnosis, a discriminant function analysis showed that labile anger alone was sufficient to predict diagnosis of borderline personality disorder versus another personality disorder with a 72% accuracy.
Contrary to expectation, affective intensity as measured by the Affect Intensity Measure was not associated with borderline personality disorder. Moreover, the greater lability in terms of anger, anxiety, and depression/anxiety oscillation in the patients with borderline personality disorder relative to those with other personality disorders were not explained simply by a higher subjective experience of emotion by the borderline personality disorder group.
There are a number of limitations in the present study. Although the Affect Intensity Measure and Affective Lability Scale have been shown to have suitable psychometric properties, they have not been widely validated for use with personality disorder populations. We did, however, find significant correlations between these scales and our raters’ independent measure of affective instability (rated according to DSM-III-R criteria), which lends support to the validity of these instruments in this study. Our instruments provided retrospective assessments of affective instability. This has the advantage of supplying a long-range perspective on a personality trait but is also subject to retrospective distortion. Nevertheless, the Affective Lability Scale and Affect Intensity Measure are self-report instruments and are subject to the subjective reporting limitations of such instruments. For these reasons it would be desirable to complement our approach with one that obtained daily (or more frequent) contemporaneous ratings by self-report and observer-report of each specific affect over a period of weeks. Because of the high comorbidity among personality disorders and with affective disorders
(13), we used statistical methods to control for these factors. It would be desirable to replicate this study in a larger group in which personality disorder patients with and without comorbid affective disorders could be directly compared. Although the average age of the borderline personality disorder patients was 34, placing them in the decade of life when borderline personality disorder symptoms begin to be less florid (DSM-IV-TR, p. 709), we believe the study group is otherwise representative of outpatients with borderline personality disorder. The rates of comorbid affective disorders in our borderline personality disorder group were comparable to those reported in the literature
(13), and about one-half of the patients had prior treatment with psychiatric medication, a rate somewhat lower than that described in contemporary clinical samples
(14) but consistent with treatment practice in the mid 1990s during our recruitment period
(15).
By separating affective instability into its components, this study provides a finer-grained perspective upon affect in patients with borderline personality disorder. The results of this study suggest that the presence of greater lability in terms of anger, anxiety, and depression/anxiety oscillation characterizes borderline personality disorder, while suggesting that the subjective sense of high affective intensity is present in this population but does not explain these other affective phenomena. Oscillation between elation and depression was not significantly associated with borderline personality disorder. Study of the instability of individual affects in personality disorder patients may help in better understanding the mechanisms of affective instability and possibly in distinguishing borderline personality disorder patients from bipolar spectrum patients. It may also help in the development of new pharmacotherapeutic approaches for stabilizing affects in patients with borderline personality disorder.