In contrast to multiple studies of the naturalistic course of bipolar disorder with onset in the late teenage years or adulthood
(1–
4), little is known about the longitudinal outcome of childhood-onset mania
(5,
6). Like follow-up studies of older age groups with mania/hypomania, follow-up of subjects with prepubertal and early adolescent bipolar disorders will be informative for providing prognostic information to families and for developing research on prevention and intervention strategies. For childhood-onset disorders, an additional rationale for naturalistic investigation is to establish continuities and discontinuities between syndromes with onset in childhood and those with onset in adulthood
(5–
7). Diagnostic issues across the age span are important not only for planning treatment, but also for conducting informed etiopathogenetic studies.
Research on childhood-onset bipolar disorders has been beset by substantial controversy over the differentiation of mania from attention deficit hyperactivity disorder (ADHD)
(8–
12). Unlike schizophrenia, which is one of the main differential diagnoses for bipolar disorder, with onset in the late teenage years or adulthood
(13,
14), ADHD has been the major problem in differential diagnosis in prepubertal and early adolescent subjects. This problem stems from the very high prevalence of comorbid ADHD in subjects with childhood-onset bipolar disorder and from the overlap of the DSM-IV criteria for mania and ADHD (e.g., hyperactivity, distractibility)
(8–
12). Although irritability is one of the most frequent symptoms of mania/hypomania at all ages
(12,
15), it is of little utility in differential diagnosis in children because of its ubiquity across the childhood diagnoses (e.g., mania, major depressive disorder, ADHD, oppositional defiant/conduct disorders). Our work has addressed the issue of differentiating childhood-onset mania from ADHD through the use of the following definition for a prepubertal and early adolescent bipolar disorder phenotype
(5–
7,
12): a current episode of DSM-IV mania/hypomania with grandiosity and/or elation as one inclusion criterion. The latter criterion was selected to ensure that diagnoses were not based only on criteria that overlapped with those for ADHD, that subjects had at least one of the two cardinal features of mania (i.e., elation and/or grandiosity), and that the diagnoses were more likely to be continuous with bipolar disorder originating in the late teenage or adult years. The prepubertal and early adolescent bipolar disorder phenotype has been validated by reliable assessment
(16), 6-month stability
(6), and 1-year diagnostic outcome
(5).
Clearly, ethical mandates precluded withholding long-term treatment to study natural history. Nevertheless, naturalistic longitudinal studies of late-teenage- and adult-onset mania have been highly informative about diagnostic outcomes
(1–
4). Naturalistic studies of adult-onset mania have also increased knowledge about the effect of lithium treatment on suicidality, social functioning, and number of hospitalizations (e.g., references
17,
18). Thus, one research question was whether psychopharmacological agents would be predictive of outcome in subjects with a prepubertal and early adolescent bipolar disorder phenotype, in which treatment was provided by the subjects’ own community practitioners.
We hypothesized that antimanic medications (defined as lithium, anticonvulsants, or neuroleptics) would not predict recovery, on the basis of the phenotypic resemblance between prepubertal and early adolescent bipolar disorder group and mixed manic, continuously cycling, psychotic, treatment-resistant bipolar disorder with onset in adulthood
(2,
5,
6,
12,
15). In this regard, poor response to psychotropic drugs has also been reported in late-teenage bipolar disorder subjects who had a history of prepubertal onset of psychopathology
(15).
On the basis of the following considerations, we hypothesized that low maternal warmth would predict relapse after recovery. In a controlled comparison of subjects with the prepubertal and early adolescent bipolar disorder phenotype, subjects with ADHD, and a community contrast group, data on psychosocial functioning showed that significantly more subjects with impaired maternal-child warmth were in the mania group
(19). Furthermore, measures of parental interaction in subjects with adult-onset bipolar disorder have been predictive of relapse
(20–
22).
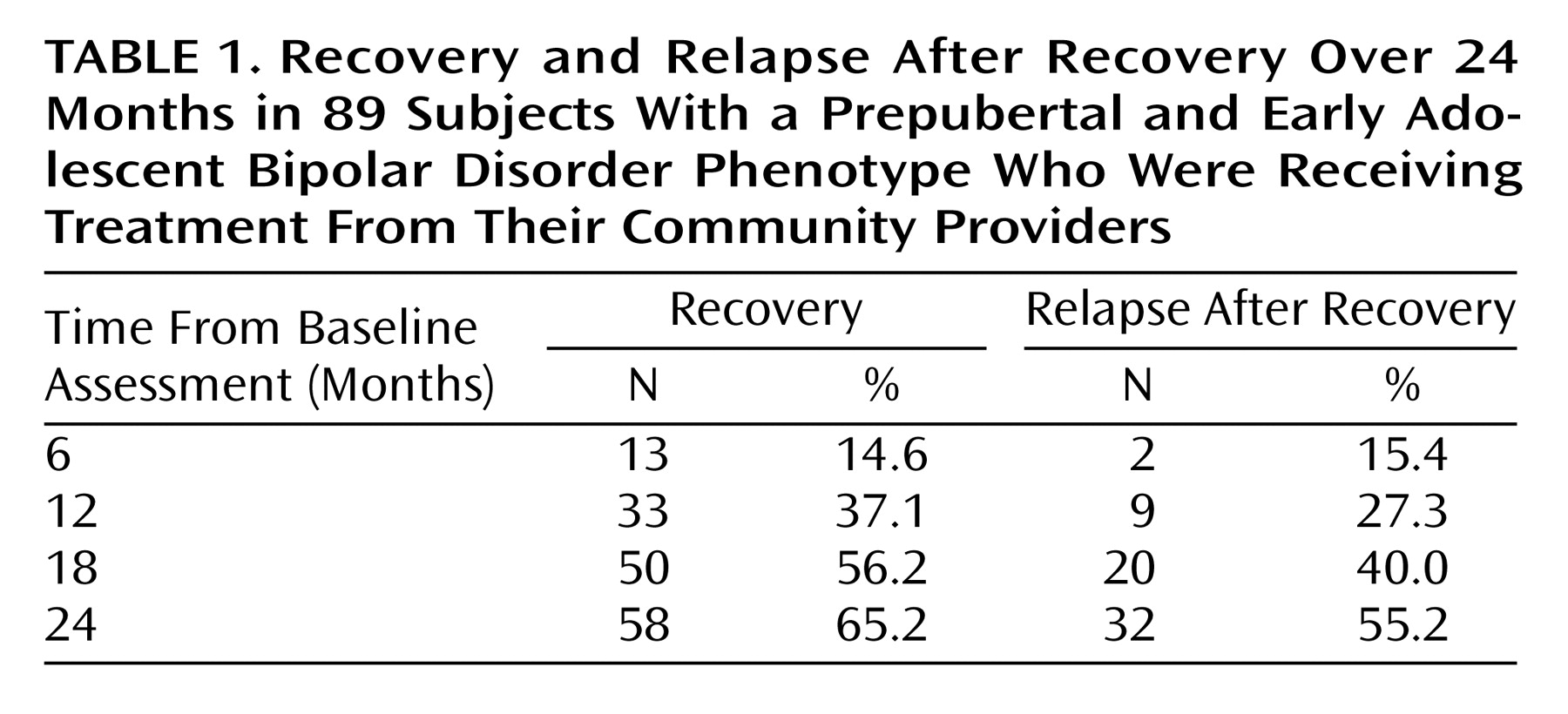
To our knowledge this is the first 2-year prospective follow-up of subjects ascertained for a prepubertal and early adolescent bipolar disorder phenotype. This communication adds to the published data on 1-year outcome
(5) because the increase in the proportion of recovered subjects between the 12- and 24-month follow-up (from 37.1% to 65.2%) provided a powerful basis for examining predictors of recovery and relapse.
Method
Participants
To enhance generalizability, subjects were obtained by consecutive new case ascertainment from outpatient pediatric and child psychiatric sites. Inpatient units at these sites were closed before the start of the study. Inclusion criteria were age 7–16 years old, good physical health, DSM-IV mania with a duration of ≥2 weeks or hypomania with a duration of ≥2 months, and clinically significant impairment indicated by a Children’s Global Assessment Scale score of ≤60
(23,
24). Both male and female subjects were included. Exclusion criteria were IQ <70, major medical or neurological illness, pervasive developmental disorders, pregnancy at baseline, and substance use disorder at baseline. Age 7 was used as the lower limit of the age range to ensure that subjects could understand the assessment questions. The conservative durations of mania/hypomania were chosen because of the controversies in the field, and elation and/or grandiosity was used as one criterion for the reasons given earlier. Although adult-onset bipolar disorder II and hypomania have been shown to have different longitudinal courses and family history validators
(25–
29), these diagnoses were included in our study for the following reasons. To our knowledge, no systematic data were available on the relative prevalences of hypomania versus mania in the prepubertal and early adolescent age group, so there was no a priori reason to exclude hypomania. Furthermore, it was not known if hypomania in children had the same longitudinal course characteristics as hypomania in older teenagers and adults
(4,
25–29). Finally, hypomania in the prepubertal and early adolescent age group might be an anlage to mania or might be partially remitted mania.
The rationales for baseline exclusion criteria were to ensure that subjects had a high enough IQ to understand the interviews, to avoid confounding mental status by other medical conditions (e.g., epilepsy, pregnancy), and to avoid confusion of mania with substance effects. After baseline, subjects continued to be followed regardless of the development of substance use disorders, medical conditions, or pregnancy.
The diagnostic homogeneity of the prevalence of manic symptoms and course features among bipolar disorder subjects from prepubertal and from early adolescent age groups has been reported
(12), providing the rationale for combining these age groups in our analyses.
During this naturalistic study, treatments were provided by participants’ own clinicians in the community and not in any way by the research personnel who conducted the baseline and 6-, 12-, 18-, and 24-month assessments. Therefore, subjects received treatments exactly as if they were not participating in a longitudinal research study.
Assessments
Assessments were comprehensive and were administered separately to mothers about their children and to the children about themselves. Information from either informant was used in accordance with published procedures
(30). Subjects were reassessed every 6 months for 2 years (i.e., at 6, 12, 18, and 24 months). At baseline the time frame covered by the assessment was current and lifetime. At the postbaseline follow-up assessments, the time frame was the prior 6 months. Psychopathology was assessed with the Washington University in St. Louis Kiddie Schedule for Affective Disorders and Schizophrenia (WASH-U-KSADS), which includes a template for substance use disorders
(16,
31). This instrument includes all DSM-IV diagnoses that occur during the prepubertal and early adolescent years except for pervasive developmental, infant feeding, mental retardation, and personality disorders. The WASH-U-KSADS has excellent reliability
(16). Because the WASH-U-KSADS has onset and offset items for all occurrences of every symptom and syndrome, weekly increments of psychopathology were available for life table analyses. Time frames during the child interviews were established by using birthdays, Christmas, Easter, Thanksgiving, other holidays, school term starts, and school term ends as reference points. Mixed mania was defined as overlapping time periods of mania/hypomania and major depressive disorder. Degrees of rapid cycling were classified with modifications of the definitions proposed by Kramlinger and Post
(32): rapid cycling as four episodes per year, ultrarapid cycling as five to 364 episodes per year, and ultradian cycling as ≥365 episodes per year. Symptom severity was assessed with the Children’s Global Assessment Scale. Interviews were performed by experienced research nurses with established interrater reliability
(16) who were blind to the subjects’ diagnostic group at baseline. The blinded baseline assessment was possible because the bipolar disorder group and two contrast groups were assessed in a random order, as described elsewhere
(11,
19).
Psychosocial assessments were obtained with the Psychosocial Schedule for School-Age Children—Revised
(33) administered separately to mothers about their children and to children about themselves by the research nurses who administered the WASH-U-KSADS and who were blind to group status at baseline. The Psychosocial Schedule for School-Age Children—Revised has been shown to have good psychometrics
(33). Measurements of maternal-child and paternal-child warmth and of maternal-child and paternal-child tension/hostility are included in this instrument. Impairments reported by either informant (i.e., mother or child) were included in the analysis. For example, if one informant reported maternal distance and the other informant reported maternal warmth, the overall rating was maternal distance.
Socioeconomic status was assessed with the Hollingshead Four-Factor Index
(34).
Medication use and psychosocial therapies were coded with the treatment section of the Longitudinal Interval Follow-Up Evaluation
(35), which includes codes for the type and dose of each medication and the type and frequency of psychosocial therapy. This instrument also includes codes for duration of and level of compliance with medications and psychosocial treatment. The Longitudinal Interval Follow-Up Evaluation was modified to weekly increments to match the weekly time frames of the WASH-U-KSADS symptom and syndrome measures.
Consensus conferences were held for each subject at each assessment to establish final diagnoses from all available material, which included the narrative documentation next to each WASH-U-KSADS item (to ensure that the severity rating matched the narrative)
(7,
16); parent, pediatrician, and teacher reports; and videotaped interviews at baseline.
After complete description of the study was provided to parents and children, written informed consent was obtained from the parents and written assent was obtained from the children.
Data Analyses
Rates of relapse and recovery were estimated with the Kaplan-Meier statistic by using the weekly increments from the WASH-U-KSADS data. Weekly increments were calculated as the number of weeks between the onset and offset time for each symptom assessed with the WASH-U-KSADS. Duration of a diagnosis was calculated as the number of weeks between onset and offset of diagnostic criteria (i.e., symptoms) that overlapped in time. Data from the 6-, 12-, 18-, and 24-month assessments were used in the Kaplan-Meier estimates. Daily or weekly logs or diaries were not obtained. The effect of covariates was analyzed by using Cox proportional hazards modeling, with significance set at <0.05. Baseline characteristics, Psychosocial Schedule for School-Age Children—Revised items, and medication categories were examined as predictors. In our previous analyses of 6-month and 1-year outcome data
(5,
6), rates of recovery were very low (
Table 1) and recovery was defined as no syndromal DSM-IV mania or hypomania for at least 2 weeks. For examining 2-year outcome, recovery was defined as at least 8 consecutive weeks without meeting DSM-IV criteria for mania or hypomania. Remission was defined as 2–7 weeks without meeting DSM-IV criteria for mania or hypomania. These definitions were adapted from Frank et al.
(36) to provide comparability across outpatient pediatric and adult studies. Relapse after recovery was defined as 2 consecutive weeks of meeting DSM-IV criteria for mania or hypomania with clinically significant impairment evidenced by a Children’s Global Assessment Scale score ≤60.
Two-tailed two-by-two contingency tables were used to compare baseline characteristics between recovered and unrecovered subjects. The p values were adjusted for the 12 comparisons by using the Bonferroni correction.
Analyses of medication effects were performed by combining data for drugs of a similar class or action (i.e., lithium, any anticonvulsant, any neuroleptic, any antidepressant, any stimulant) and by a category of any antimanic drug (defined as lithium, any anticonvulsant, or any neuroleptic). Medications needed to be administered for at least two consecutive weeks to be counted. For analyses of recovery, the time frame for medications was the number of weeks between baseline and recovery (or the 24-month time point for subjects who did not recover). The medication use time frame for analyses of relapse after recovery was the number of weeks between recovery and relapse (or the 24-month time point in the nonrelapsed). Mean doses and mean durations were reported in detail elsewhere and were within the range of commonly accepted regimes for adequate therapy in adult-onset mania
(6). Data-reduction methods for analyses of medications were necessary due to the very wide variety of psychotropic medications. For example, subjects were administered 25 different psychotropic medications between baseline and the 6-month assessment point
(6). Psychopharmacology interventions have been predictive of naturalistic outcome in adult-onset bipolar disorder (e.g., references
2,
17,
18) and were included in our recovery and relapse models in spite of the paucity of controlled data on their efficacy or effectiveness in prepubertal and early adolescent bipolar disorder
(15,
37,
38).
Psychotherapy categories that occurred were individual and family. To enter the analyses, there needed to be ≥4 sessions within a consecutive 8-week period.
The maternal-child and paternal-child warmth and maternal-child and paternal-child tension/hostility items were based on the family of residence and were taken from the Psychosocial Schedule for School-Age Children—Revised. Details on the construction of categories of parental-child warmth and parental-child tension/hostility were previously reported
(19). In the Cox proportional hazard modeling, a category of high maternal-child warmth (or high paternal-child warmth) was compared to a combined category of somewhat distant and distant/cold mother-child (or father-child) interactions. The category of mother-child (or father-child) tension/hostility was analyzed by comparison of a category of low tension/hostility to a combined category of somewhat tense/hostile and very tense/hostile interactions.
The category of living in an intact biological family (i.e., living in the same household as both biological parents) on the Psychosocial Schedule for School-Age Children—Revised was contrasted to a combined category of all other living situations.
Results
Baseline Characteristics
At baseline, there were 93 subjects. At 2-year follow-up, four subjects (who did not differ demographically from the continuers) had discontinued participation in the study. The 89 subjects followed from baseline to 2 years were 95.7% of the baseline group. Subjects at baseline had a mean age of 10.9 years (SD=2.7), 36 (40.4%) were female, 51 (57.3%) were prepubertal, and 79 (88.8%) were Caucasian. Their mean socioeconomic status was in the second highest of five classes.
The mean age of onset of illness was 7.3 years (SD=3.5), and the mean duration of the baseline episode was 3.6 years (SD=2.5). Subjects’ mean score on the Children’s Global Assessment Scale was 43.3 (SD=7.7), in the moderate and severe range of impairment. Twenty-seven subjects (30.3%) were ascertained from pediatric sites, and 62 (69.7%) were from psychiatric sites. There were 48 subjects (53.9%) with mixed mania, 53 (59.6%) with psychosis (defined as impairing hallucinations and/or delusions), 37 (41.6%) with no lifetime or current major depressive disorder, 22 (24.7%) with suicidality, 77 (86.5%) with comorbid ADHD, and 67 (75.3%) with comorbid oppositional defiant/conduct disorders. Sixty-nine subjects (77.5%) had ultradian cycling (at least one cycle per day) with a mean number of episodes per day of 3.7 (SD=2.1); thus, they were essentially continuously cycling. No subject had four episodes per year. High maternal-child warmth was present in 40 subjects (44.9%), and 51 (57.3%) lived in an intact biological family.
After correction for multiple comparisons, there were no significant differences in baseline characteristics between the 58 subjects (65.2%) who had recovered and the 31 subjects (34.8%) who had not recovered.
Raw Recovery and Relapse Data
Table 1 shows the numbers and percentages of subjects who recovered from mania and who relapsed after recovery at the 6-, 12-, 18-, and 24-month time points. Only one subject’s illness remitted, and this subject was included in the group of recovered subjects for the analyses. There were no differences in rates or predictors of recovery by including this subject with the recovered or unrecovered group.
Rate of Recovery
At 2 years, 58 (65.2%) of the 89 subjects had recovered from mania. The Kaplan-Meier estimate of the rate of recovery was 65.2% (95% confidence interval [CI]=55.3%–75.1%). The mean time to recovery was 36.0 weeks (SD=25.0).
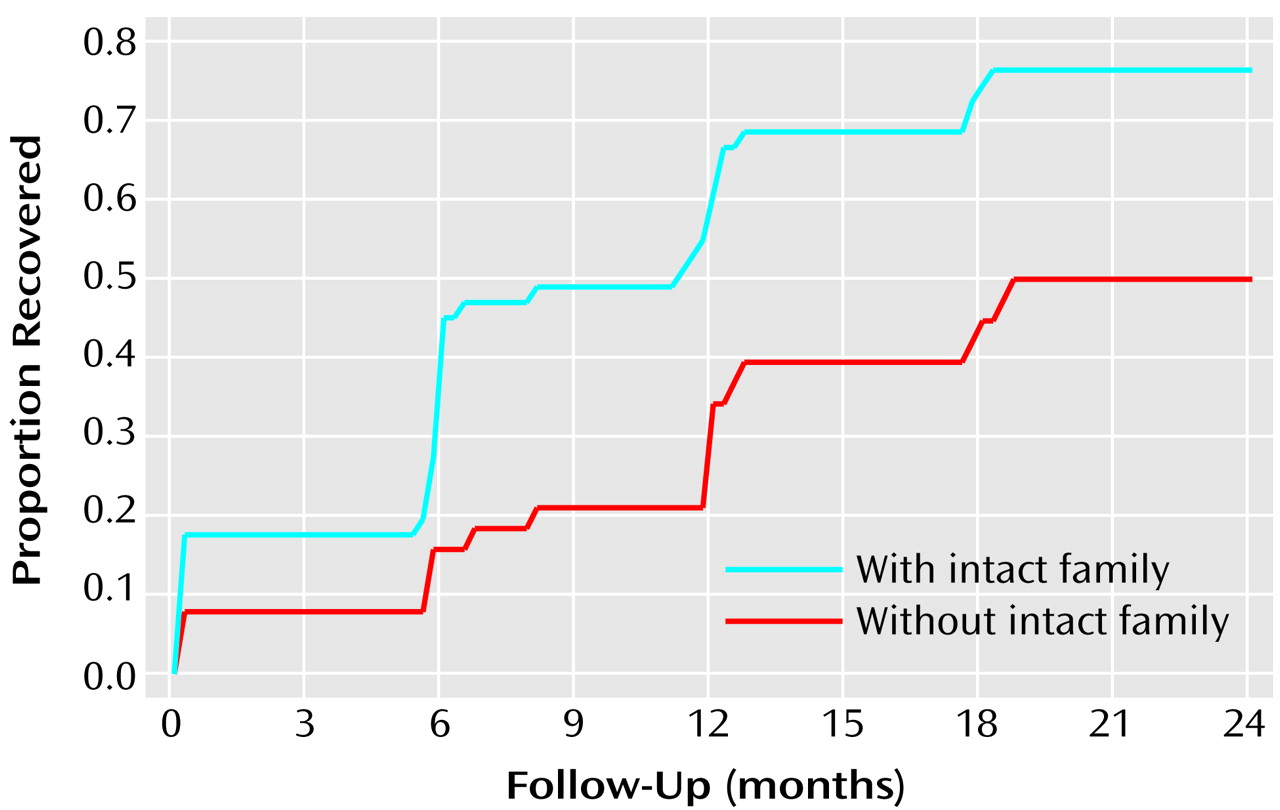
Figure 1 presents the rates of recovery of subjects living in an intact biological family and those in other living situations. Living with an intact biological family significantly predicted recovery after the analysis controlled for the effects of puberty status, gender, mixed mania, and maternal-child warmth (χ
2=7.40, df=1, p=0.007). According to the hazard ratio estimated with Cox proportional hazards modeling, subjects living with their intact biological families were 2.2 times (95% CI=1.2–3.8) more likely to recover than those in other living situations.
No other baseline characteristics (e.g., major depressive disorder, Children’s Global Assessment Scale score, mixed mania, continuous cycling, psychosis, oppositional defiant/conduct disorders) predicted recovery.
Forty-two subjects (47.2%) received at least one antimanic medication between baseline and time of recovery (or the 24-month time point in unrecovered subjects). The only significant difference in baseline characteristics between subjects who did and did not receive an antimanic medication was a higher prevalence of psychosis in subjects who received an antimanic drug (χ2=6.71, df=1, p=0.01). There was no significant difference in rate of recovery for subjects who did and did not receive lithium or an anticonvulsant drug.
Subjects who received a neuroleptic drug between baseline and recovery (or the 24-month time point) (N=36 [40.4%]) were significantly less likely to recover than those who did not receive a neuroleptic drug (χ2=13.27, df=1, p=0.0003). Subjects who received a neuroleptic drug were also significantly more likely than those who did not to have baseline psychosis (χ2=5.99, df=1, p=0.01), oppositional defiant/conduct disorders (χ2=6.02, df=1, p=0.014), and lifetime or current major depressive disorder (i.e., bipolar I disorder or bipolar II disorder) (χ2=4.73, df=1, p=0.03).
Subjects who received individual and/or group therapy between baseline and recovery (or the 24-month time point) (N=48 [53.9%]) were significantly less likely to recover (χ2=13.74, df=1, p=0.0002) than those who did not received these interventions. Subjects who received individual and/or group therapy were also significantly more likely than those who did not to be ascertained at a psychiatric site (χ2=4.45, df=1, p=0.03) and to have baseline psychosis (χ2=5.51, df=1, p=0.02). Family therapy, received by 19 of the 89 subjects (21.3%) did not predict recovery.
Rate of Relapse After Recovery
Thirty-two of the 58 subjects who had recovered within the 24-month time frame relapsed after recovery. The Kaplan-Meier rate of relapse after recovery was 64.0% (95% CI=48.9%–79.0%). The mean time between recovery and relapse was 28.6 weeks (SD=13.2).
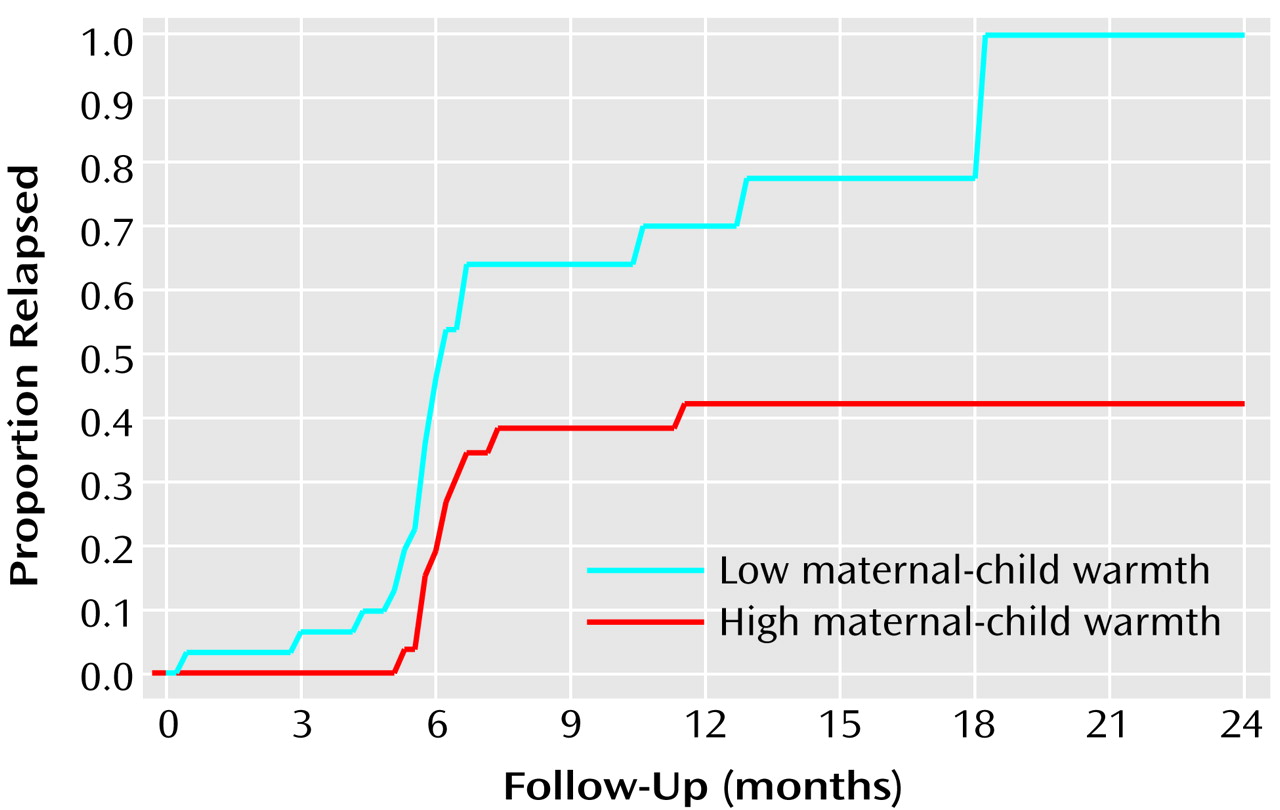
Figure 2 shows the rates of relapse after recovery by level of maternal-child warmth. Low maternal warmth significantly predicted relapse after recovery, after the analysis controlled for the effects of puberty status, gender, mixed mania, and living with an intact biological family (χ
2=9.84, df=1, p=0.002). According to the hazards ratio estimated with Cox proportional hazards modeling, subjects with low maternal-child warmth were 4.1 times (95% CI=1.7–10.1) more likely to relapse after recovery than subjects with high maternal-child warmth.
No other baseline characteristics (including paternal warmth) or medications and psychotherapies received between recovery and relapse predicted relapse.
Other Outcome Findings
Neither antidepressant drugs (administered to 26 subjects [29.2%]) nor stimulant medications (administered to 53 subjects [59.6%]), with or without concomitant antimanic drugs, predicted recovery or relapse.
Twelve subjects recovered again after relapsing. This number was too small for additional analyses.
Eight of the 10 subjects with hypomania at baseline developed mania during the 24-month follow-up. Eight subjects with baseline hypomania recovered, and four of these eight relapsed after recovery. The number of hypomanic subjects was too small for separate analyses.
The proportions of recovered subjects who had ADHD, oppositional defiant/conduct disorders, and/or major depressive disorder at any time during recovery were 32.8%, 24.1%, and 29.3%, respectively. No subject developed a substance dependency disorder during the 2-year follow-up.
Discussion
Limitations of these findings are that the results may not generalize to other phenotypes or to studies with subjects from lower socioeconomic status classes.
The low rate of recovery from mania and the high rate of relapse after recovery, compared to data on adult-onset mania
(2,
15), were consistent with the phenotypic resemblance of the prepubertal and early adolescent bipolar disorder subjects to their adult counterparts with treatment-resistant, mixed/cycling bipolar disorder
(2,
5,
6,
12,
15). Thus, the study hypothesis of relatively poor outcome, compared to reports in adult-onset bipolar disorder, was supported. An important question is whether the group with prepubertal and early adolescent bipolar disorder phenotype will continue to have a clinical picture that includes mixed mania and continuous rapid cycling as they age. If they do, as adults they will resemble the patients with the continuously cycling/mixed features found in <20% of cases of adult-onset bipolar disorder
(15). If they do not, will they resemble their modal adult counterparts, who have discrete episodes of mania or depression of 2–9 months’ duration with relatively well periods between episodes
(15)? Future longitudinal study of subjects with the prepubertal and early adolescent bipolar disorder phenotype can address these issues. In this regard, the recent National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder
(39) noted a consensus in the field that prepubertal children with bipolar disorder frequently have continuous cycling, without the intervening well periods reported for the modal, typical adult presentation.
Several authors have reported that high levels of expressed emotion predict relapse after recovery from adult-onset bipolar disorder
(20–
22). Ideally, assessment of expressed emotion would have been conducted, but this was outside the scope of the follow-up study. Measurements of maternal warmth from the Psychosocial Schedule for School-Age Children—Revised, which are akin to those of expressed emotion, predicted relapse after recovery in the hypothesized direction. On the basis of this finding, future research on expressed emotion and psychosocial intervention for subjects with childhood-onset bipolar disorder is warranted.
The significant effect of residence with the intact biological family was an unexpected finding. One question raised by this finding is the potential effect of a sick child on divorce. In this regard, a survey of 1,126 families of medically disabled individuals aged 12–20 did not find higher rates of divorce than those in a normal comparison group
(40). Controlled follow-up studies of unaffected offspring of parents with bipolar disorder can prospectively examine whether divorce is temporally related to the onset of bipolar disorder during childhood and, conversely, whether early onset of bipolar disorder is temporally related to divorce
(41).
Our group is conducting an ongoing study of psychopathology in first-degree relatives of the probands in this communication. When these data become available, the relationships of family diagnoses to outcome and to family intactness can be examined.
Interpretation of medication data collected in naturalistic studies is limited because the medication is administered by community practitioners and not in a treatment research setting. It is especially problematic to interpret naturalistic psychopharmacology data in subjects with prepubertal and early adolescent bipolar disorder owing to the paucity of treatment studies in this age group
(15,
37,
38). There are too few data to establish efficacious classes or dosing of mood stabilizers in prepubertal and early adolescent mania. The following speculations are given with these provisos in mind. The lack of significant relationships between lithium or an anticonvulsant drug and recovery or relapse may reflect relative treatment resistance to these agents across the lifespan in subjects with a mixed/cycling presentation
(2). Another speculation is that the efficacy of lithium or anticonvulsants (for psychiatric indications) varies with the age of the subjects. Differential effects of drugs in pediatric versus adult age groups have been established for other medications. An example is the lack of proven efficacy of tricyclic antidepressants in children or adolescents with major depressive disorder
(42,
43).
The negative effects on recovery of receiving neuroleptic drugs or individual psychotherapy were most likely based on the symptom severity of subjects who received these modalities (e.g., these subjects had a higher prevalence of psychosis).
As discussed previously
(5,
6), the low proportion of subjects who received any antimanic drug (47.2%) may be due to underdiagnosis of child-onset mania by practitioners.
Overall these findings powerfully argue for research on psychosocial and psychopharmacological strategies and on pathogenetic mechanisms for mania during the prepubertal and early adolescent years.