Advanced paternal age has been proposed as a risk factor for the later development of schizophrenia in the offspring
(1,
2). However, one study in which social factors were taken into account did not show such an association
(3). Recently, in a methodologically stronger study of a birth cohort from Jerusalem
(4), a higher risk for schizophrenia among subjects with older fathers was once again shown. De novo mutations arising in paternal germ cells were suggested as the underlying mechanism. The study included 658 cases of schizophrenia and related nonaffective psychosis (ICD-10 codes F20–F29) from the psychiatric registry. Unfortunately, there was no information available on the validity of the diagnoses or on the proportion of subjects with schizophrenia. In the Swedish inpatient register, cases of broad schizophrenia (ICD-9 code 295) constitute approximately 55%–60% of the treated patients with those diagnoses. In this article we present the results from a population-based case-control study including 524 cases of broad schizophrenia in which we were able to take several possible confounding factors into account.
Method
We used the Stockholm County inpatient register
(5) to identify all people born in Stockholm during 1960–1977 who had received a diagnosis of schizophrenia syndrome (ICD-8 and ICD-9 code 295, corresponding to ICD-10 codes F20, F21, F23.1–F23.2, F25) between 1971 and 1994 (N=648). Deceased individuals (N=51) and those who did not reside in Stockholm (N=32) were excluded. The parishes of birth of the remaining 565 subjects were obtained from taxation offices, and the birth hospitals were then located; 37 (6.5%) of the birth records could not be retrieved.
Each of the subjects with schizophrenia was matched with two subjects from the parish register who 1) were born immediately after the subject with schizophrenia, 2) were matched for sex and hospital of birth, and 3) resided in Stockholm at the time the cases were selected. For 87 (7.7%) of the 1,130 matched comparison subjects, birth records could not be retrieved. Four subjects with schizophrenia lacked comparison subjects because of the low number of births in the parish, and they were excluded, leaving 524 subjects with schizophrenia and 1,043 comparison subjects.
The records contain information on parental date of birth, occupation, marital status, and obstetric complications. The 1,567 birth records were copied in the archives and given code numbers to conceal each subject’s status (schizophrenia or comparison). The records were randomly assembled and given in batches to a midwife, who extracted data according to a protocol.
A socioeconomic index
(6) was estimated from data on parental occupation and was based on the highest socioeconomic status in the family: group I (socioeconomic index 54–87) included upper-level executives and the self-employed, group II (socioeconomic index 33–47) included assistant nonmanual employees, and group III (socioeconomic index 11–22) included unskilled and skilled employees in goods and service production.
Through a linkage with the national inpatient register, we identified mothers who had been admitted to hospitals during 1971–1996 with psychotic illness (ICD-8 codes 295–299, ICD-9 codes 295–298).
Odds ratios and 95% confidence intervals (CIs) for schizophrenia in relation to paternal age were calculated by using conditional logistic regression and were adjusted for possible confounders, i.e., maternal age (<20, 20–24, 25–39, ≥40 years), parity (1, 2 or 3, ≥4), marital status (married, unmarried, or divorced), socioeconomic index, maternal psychotic illness, and any of the following obstetric complications: preeclampsia, gestational age <33 weeks, small for gestational age, signs of asphyxia (complications expected to yield an Apgar score less than 7 at 1, 5, or 10 minutes), and hyperbilirubinemia (>15 mg/dl).
Results
There was information about paternal age in the birth records of 420 (80.2%) of the 524 subjects with schizophrenia and 857 (82.2%) of the 1,043 comparison subjects. Thus, the distribution of dropouts was even.
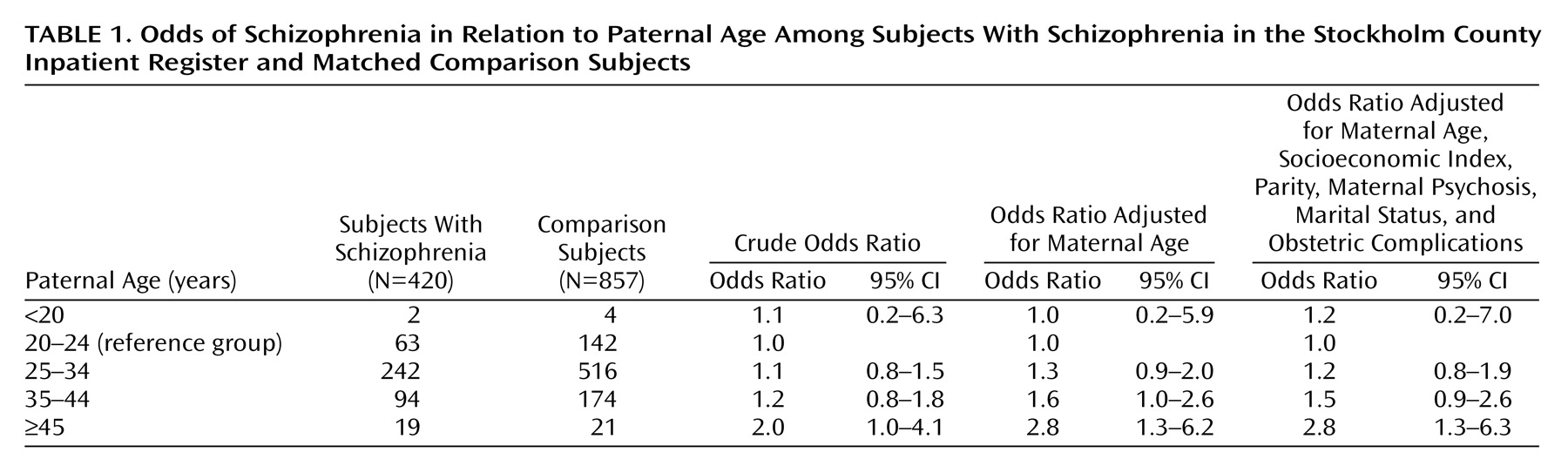
There was an increased risk of schizophrenia associated with advanced paternal age (
Table 1). Having a father aged 45 years or older was associated with a doubled risk for schizophrenia. Since the age of the father is expected to be associated with the age of the mother, we adjusted for this factor, which increased the odds ratio to 2.8. Finally, we also adjusted for parity, social factors, maternal psychotic illness, and obstetric complications. This procedure did not substantially alter the results.
Higher or lower maternal age was not associated with increased risk for schizophrenia; for mothers 40 years old or older the odds ratio was 0.6 (95% CI=0.2–1.7), and for those younger than 20 years the odds ratio was 1.2 (95% CI=0.7–2.2).
Discussion
This study confirms the results from the Jerusalem study
(4). Thus, there seems to be an association between advanced paternal age and the later development of schizophrenia. There was no association with greater maternal age. After adjustments for maternal age, the risk estimates increased, which indicates that the father’s age is the factor of interest in this study, not maternal age. The association was not affected when we controlled for social factors or obstetric complications.
In this study we investigated the impact of paternal age in a large sample of persons with schizophrenia. The information was collected at birth without knowledge of future disease status, thus decreasing the risk of bias. The diagnoses of the Stockholm inpatient register have been validated and proved to be of good quality. Approximately 80% of the ICD diagnoses in the register fulfilled the DSM criteria for schizophrenia
(5). A limitation of the study is the lack of data on paternal psychiatric illness, which is a possible confounder. Another drawback is that 20% of the birth records lacked information on paternal age. The lack of information was evenly distributed among subjects with schizophrenia and comparison subjects, and we cannot find any reason to suspect any systematic bias regarding this factor, especially since social factors did not seem to have an impact on the results.
What are the possible underlying mechanisms? As proposed by Malaspina et al.
(4), de novo mutations arising in paternal germ cells may be an explanation, since the rate of these mutations increases with advancing age and they have been shown to be related to disease
(7,
8). Having an older father may be associated with early parental loss, which may be a risk factor for schizophrenia. On the other hand, this is to some extent contradicted by the fact that having an older mother was not associated with the risk of schizophrenia. There is also the possibility of a specific biological parental trait leading to delayed childbearing and schizophrenia.
In conclusion, our results support previous findings of an association between advanced paternal age and the risk of schizophrenia. The findings may be of interest for further studies on the genetic mechanisms behind schizophrenia.