Method
Patients were eligible to participate in this outpatient trial if they 1) successfully completed inpatient treatment (defined as achievement of at least 90% of ideal body weight based on the 1959 Metropolitan Life Insurance Tables for a minimum of 2 weeks, normalization of eating, and resolution of acute medical problems) and 2) lived within commuting distance of the hospital. During the recruitment period, 43 women met these eligibility criteria, and 33 were randomly assigned to treatment. Of the 10 women who did not enter the study, four were referred to long-term inpatient or day treatment programs because of severe comorbid psychopathology, and six returned to prehospitalization therapists.
The 33 study participants were between the ages of 18 and 45 years, had DSM-IV diagnoses of anorexia nervosa, and had successfully completed inpatient hospitalization at New York State Psychiatric Institute. The study was explained to potential participants, and written informed consent was obtained at the time of random assignment to treatment. This study was approved by the New York State Psychiatric Institute institutional review board.
The cognitive behavior therapy and nutritional counseling in this trial consisted of 50 individual sessions delivered over the 1 year after hospitalization. The goals of both interventions were maintenance and consolidation of gains achieved on the inpatient unit, continued improvement and recovery, and relapse prevention.
Cognitive behavior therapy is widely implemented in anorexia nervosa treatment; however, we have found no empirical data for its application to adult anorexia nervosa. Given the well-documented efficacy of cognitive behavior therapy for bulimia nervosa
(5), in this study we evaluated a manual-based method (available on request from Dr. Pike) consistent with recommendations specific to cognitive behavior therapy for anorexia nervosa
(6). Cognitive behavior therapy for anorexia nervosa focuses on cognitive and behavioral features associated with the maintenance of eating pathology and uses a schema-based approach to address a range of issues related to self-esteem, self-schema, and interpersonal functioning.
The nutritional counseling intervention was a manual-based treatment (available on request from Dr. Pike) built on well-established principles of nutritional education and food exchanges
(7,
8). Nutritional counseling is psychoeducational and supportive, and it focuses on specific dietary analyses and balanced meal planning. Nutritional counseling was used as the comparison treatment because, in the absence of scientifically established treatment standards, it is a credible clinical intervention that is a standard component of anorexia nervosa treatment
(9).
Cognitive behavior therapy and nutritional counseling were conducted by four doctorate-level licensed, experienced psychologists. The therapists in both modalities participated in extensive training and supervision and met competency criteria, and all sessions were audiotaped. Senior supervisors (G.T.W., K.V., and J.B.) evaluated a portion of the tapes for integrity and adherence to treatment protocols and conducted bimonthly supervision. On-site supervision was conducted weekly.
The participants were randomly assigned to their treatment conditions immediately before their first session in the outpatient trial, which was scheduled within 1 week of successful completion of hospitalization. Random assignment to treatment condition was based on an adaptive stratification procedure
(10) to control for possible effects of duration of illness
(2), illness subtype
(11), and medication status at time of discharge. Eighteen women were randomly assigned to cognitive behavior therapy, and 15 were assigned to nutritional counseling.
Study physicians met with the patients monthly to monitor their medical condition. If treatment with antidepressant medication was initiated in the hospital because of a continuing mood disorder despite weight restoration, it was continued throughout the outpatient trial and monitored by the study physician. No psychopharmacological interventions were initiated during the randomized trial.
Study participation was terminated if 1) the subject’s weight fell below a body mass index of 17.5 kg/m2 (approximately 80% of ideal) for more than 10 days; 2) medical status was compromised by exacerbation of anorexia nervosa pathology to the extent that alternative, inpatient care was required (e.g., laxative overdose resulting in an emergency hospitalization); or 3) exacerbation of non-eating-disorder psychopathology (e.g., attempted suicide) required alternative care.
At randomization and end of treatment, eating pathology was assessed by interview with the Eating Disorder Examination
(12). The complete Structured Clinical Interview for DSM-IV Axis I Disorders (SCID)
(13) was administered at the prehospitalization evaluation. A modified SCID was administered at randomization and end of treatment to assess current comorbid psychopathology. Height and weight were measured at the time of initial evaluation. Weight was measured weekly during the trial to calculate body mass index.
At the end of session 1, four self-report questions about treatment credibility and expectancy were completed by using a 15-point visual analogue scale.
Results
According to two-tailed t tests, the group receiving cognitive behavior therapy did not differ significantly from the group receiving nutritional counseling on any baseline characteristic: the mean ages were 26.1 (SD=6.2) and 24.3 (SD=6.9) years, respectively, the mean ages at illness onset were 17.4 (SD=5.2) and 16.5 (SD=3.1) years, the mean durations of illness were 7.6 (SD=5.9) and 7.3 (SD=5.8) years, the mean numbers of previous hospitalizations were 1.8 (SD=2.6) and 1.1 (SD=1.2), the mean body mass indexes at evaluation were 16.0 (SD=2.1) and 15.2 (SD=1.5) kg/m2, the highest body mass indexes at the subjects’ current heights were 22.1 (SD=3.8) and 21.1 (SD=2.6), and the lowest body mass indexes at the current heights were 13.9 (SD=2.4) and 14.4 (SD=1.4). The rates of the restricting subtype were 56% (10 of 18) and 40% (six of 15), respectively, and were not significantly different (χ2=0.79, df=1, p<0.37).
The patients receiving cognitive behavior therapy did not differ significantly (according to Mann-Whitney t tests) from those receiving nutritional counseling on any of the four measures of treatment credibility or expectancy: the mean scores for treatment logic were 11.18 (SD=3.0) and 10.61 (SD=3.3) for cognitive behavior therapy and nutritional counseling, respectively. The mean scores for treatment relevance were 10.6 (SD=3.6) versus 10.0 (SD=2.8), the mean scores for expectation of success were 10.2 (SD=3.0) versus 11.6 (SD=2.5), and the mean scores for treatment response were 11.1 (SD=2.0) versus 11.7 (SD=1.3) for cognitive behavior therapy and nutritional counseling, respectively.
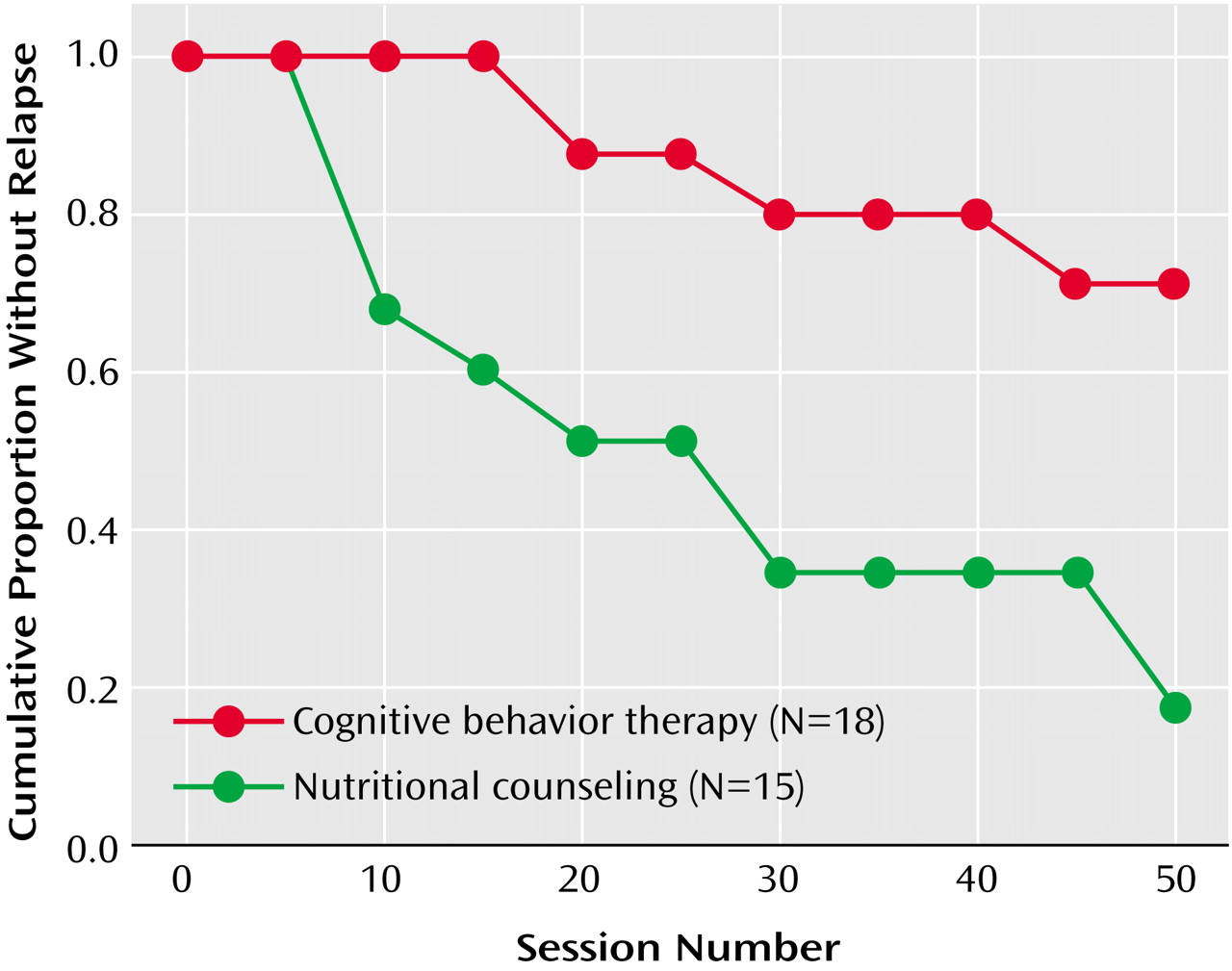
A Kaplan-Meier survival analysis (
Figure 1) comparing the time to relapse for the two treatment groups indicated a significant difference (long-rank statistic=8.39, p<0.004). Those receiving cognitive behavior therapy remained in treatment significantly longer without relapsing (mean session=43.79, SD=2.9) than those receiving nutritional counseling (mean session=27.21, SD=5.9).
During the 1-year trial, the criteria for relapse were met by 53% of the patients in the nutritional counseling group (eight of 15) and 22% of those in the cognitive behavior therapy group (four of 18) (χ2=3.42, df=1, p<0.06). In the cognitive behavior therapy group, three women relapsed because of weight loss and one relapsed because of both weight loss and increased suicidality. In the nutritional counseling group, five women relapsed because of weight loss and three were referred to alternative care because of severe depression, including active suicidal ideation in two participants.
In the survival analysis, individuals who voluntarily dropped out of treatment were not considered to have had relapses. The number of early dropouts, defined as patients who discontinued treatment before session 10, was higher for nutritional counseling (three of 15, 20%) than for cognitive behavior therapy (N=0) (χ2=3.96, df=1, p<0.05).
Overall treatment failure represents both individuals who relapsed and those who dropped out of treatment within the first 10 sessions. A chi-square comparison revealed a significantly lower overall treatment failure rate for cognitive behavior therapy (22%, four of 18) than for nutritional counseling (73%, 11 of 15) (χ2=8.62, df=1, p<0.003).
A significantly higher percentage of individuals in the cognitive behavior therapy condition (44%, eight of 18) than in the nutritional counseling group (7%, one of 15) met modified Morgan-Russell criteria
(1,
2) for “good outcome” (χ
2=5.89, df=1, p<0.02). However, a limitation of these criteria is that they do not cover related psychological and behavioral variables that are core criteria of anorexia nervosa. As a result, an individual could meet the criteria for good outcome but still be symptomatic in terms of weight concerns, shape concerns, and eating behavior. Following the practice in other studies
(1,
3), we established an operational definition of “full recovery” by using the Eating Disorder Examination interview. Patients had to meet the criteria for good outcome
and 1) eating attitudes and weight concerns had to be less than one standard deviation above the mean of a comparison group without eating disorders and 2) binge eating or purging behaviors had to be absent. These criteria for full recovery were met by 17% (three of 18) of the cognitive behavior therapy group and none of the individuals in the nutritional counseling group (χ
2=2.75, df=1, p<0.10).
At the time of random assignment, 17 participants were taking antidepressant medication (fluoxetine: N=13, venlafaxine: N=2, fluvoxamine: N=1, paroxetine: N=1). All medications were initiated on the inpatient unit because significant mood disturbance continued despite weight restoration, and four patients continued to meet criteria for mood disorder despite medication.
The primary purpose of this clinical trial was not to examine medication effects, so adaptive stratification procedures accounted for medication status in the assignment of patients to the treatment conditions. However, given that 17 of the 33 patients were taking medication during the clinical trial, exploratory analyses were conducted to ascertain whether medication appeared to affect outcome at this stage of treatment. A chi-square analysis of medication status by outcome status (“good” versus “fair,” “poor,” and “other” combined) was conducted for each treatment condition. No significant medication effects were identified for nutritional counseling (χ2=0.71, df=1, p<0.39). The findings for cognitive behavior therapy suggested a medication effect: seven of the eight patients who met the criteria for good outcome were receiving medication, compared to four of the 10 who did not meet the criteria for good outcome (χ2=4.21, df=1, p<0.04).
Chi-square analyses indicated that subtype did not have a significant impact on outcome for the overall study (χ2=0.08, df=1, p<0.78) nor when examined by treatment condition (cognitive behavior therapy: χ2=0.18, df=1, p<0.67; nutritional counseling: χ2=0.71, df=1, p<0.39).