After catastrophic trauma, 14% to 25% of individuals develop posttraumatic stress disorder (PTSD)
(1), and about 26% of individuals who experience trauma subsequently develop depression
(2). Each of these disorders increases the risk for suicidal behavior
(3,
4). Studies of the risk of suicidal behavior in patients with diagnoses of both PTSD and major depressive episode
(1,
5–7) suggest a synergistic effect on suicidal behavior.
A computer-assisted literature review identified no studies of PTSD and suicidal behavior in adults with depression. We hypothesized that depressed patients who also had the diagnosis of PTSD would show more suicidal behavior. We examined the contribution of the following risk factors for suicidal acts: aggression, history of childhood abuse, and cluster B personality disorders.
Method
Patients consecutively admitted to the hospital for biological studies of major depressive episode (bipolar or unipolar) (N=156) were given tests measuring depression, hopelessness, substance abuse, aggression, impulsivity, suicidal ideation, suicidal intent, and medical damage secondary to attempted suicide. Past or current PTSD was diagnosed on the basis of the Structured Clinical Interview for DSM-III-R.
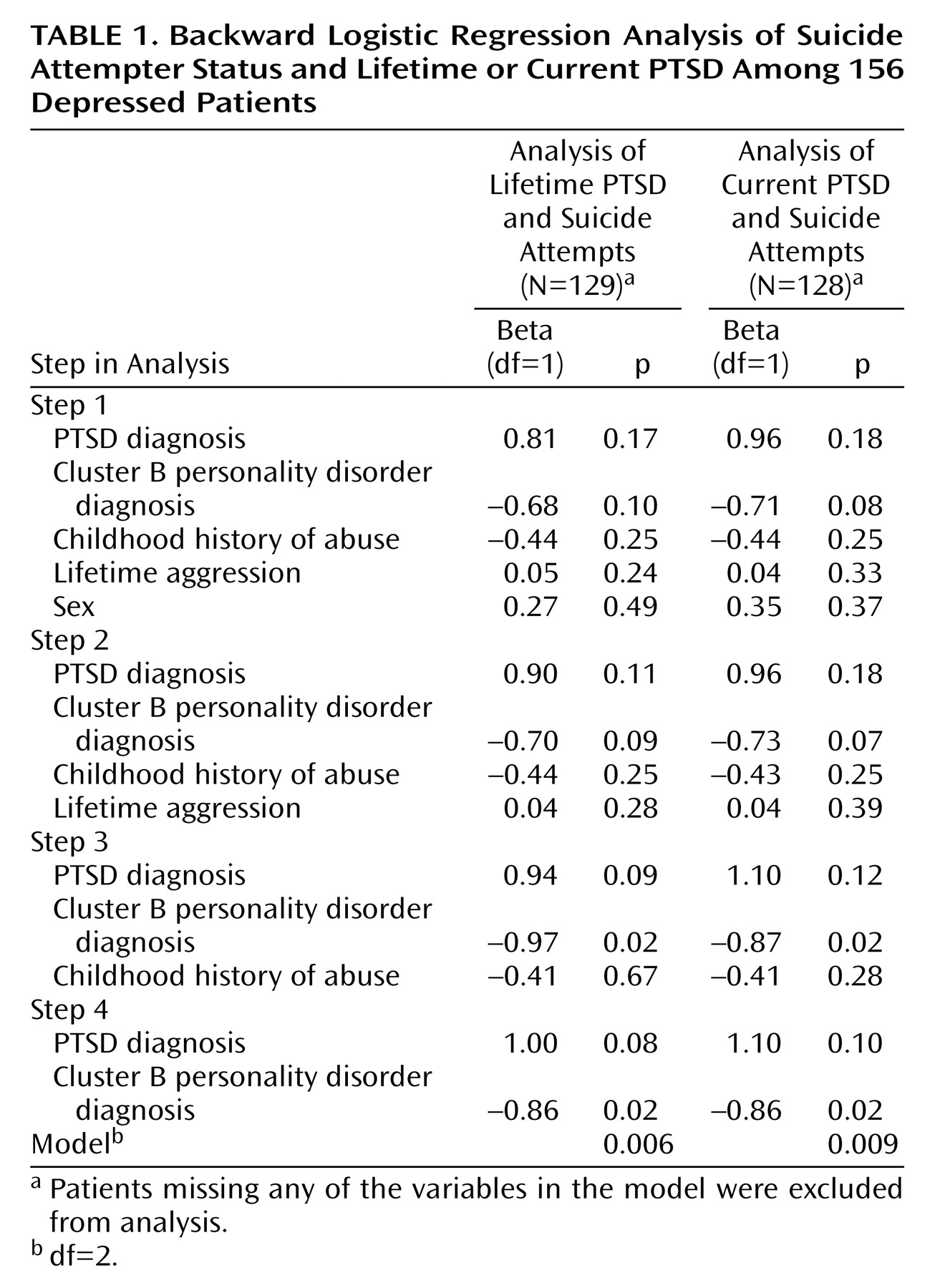
Clinical and demographic variables were examined by using Student’s t tests and chi-square tests or Fisher’s exact tests. Backward stepwise logistic regression, a data-driven method that eliminates the variable with the lowest significance (highest p value) at each step, generated models containing the independent variables that best predicted the dependent variable (having made a suicide attempt). The first model examined the relationship between suicide attempt status (dependent variable) and sex, lifetime PTSD, cluster B personality disorders, history of childhood physical or sexual abuse, and aggression. A similar model examined the relationship between suicide attempt status and current diagnosis of PTSD.
Results
Depressed patients with lifetime (N=24) or current (N=15) PTSD did not differ in age, race, income, education, presence of cluster B personality disorders, history or age at onset of childhood abuse, impulsivity, hopelessness, or depression from those without PTSD (data not shown). However, women outnumbered men by a ratio of 6:1 in the group with depression and current PTSD and 10:1 in the group with depression and lifetime PTSD. Furthermore, among the 62 subjects who reported abuse (40% of the study group, regardless of PTSD status), more women than men had lifetime PTSD (ratio=8:1), although the distribution of men and women was even in abused subjects without lifetime PTSD (p<0.04, Fisher’s exact test). Among the 24 patients with any PTSD, reported traumata precipitating PTSD were physical threat to the patient (N=9 [38%]), physical abuse (N=6 [25%]), sexual abuse (N=4 [17%]), and unknown (N=5 [21%]).
More of the depressed patients with lifetime PTSD were suicide attempters than those without PTSD (N=18 [75%] versus N=63 [54%]) (χ2=6.39, df=1, p≤0.01), and more of the depressed patients with current PTSD were suicide attempters than those without PTSD (N=12 [80%] versus N=63 [54%]) (χ2=5.89, df=1, p≤0.02). However, suicide attempters with diagnoses of major depressive episode and PTSD had similar numbers of suicide attempts, suicidal intent, age at first suicide attempt, and medical damage from suicidal acts as suicide attempters who had a diagnosis of major depressive episode but not PTSD. Patients with current PTSD plus major depressive episode had higher scores on the measures of suicidal ideation (mean=19.4, SD=9.5) and aggressivity (mean=20.4, SD=6.3) than patients with major depressive episode alone (mean=12.5, SD=9.4, and mean=17.3, SD=4.9, respectively) (t=–2.25, df=138, p<0.03, and t=–2.43, df=137, p<0.02, respectively). Patients with depression plus lifetime PTSD had more suicidal ideation and aggressivity than those with depression alone, but not statistically significantly so.
Each regression analysis yielded a model with cluster B personality disorders and PTSD as predictors of suicide attempt status (
Table 1).
Discussion
More depressed patients who also had PTSD than depressed patients without PTSD had attempted suicide, and PTSD and cluster B personality disorders were independent predictors of attempter status.
Consistent with the findings of Marshall et al.
(8), we found that suicidal ideation was most severe in the depressed patients who had current PTSD and, therefore, more symptoms, suggesting that suicidal ideation lessens in major depressive episodes once PTSD subsides. Although PTSD did not influence suicidal intent, age at first attempt, or the number of attempts or medical damage caused by the attempts, depressed patients with current PTSD had more aggressivity. An association between suicidal behavior and aggressivity has been reported in borderline personality disorder
(9) and major depression
(10). Higher levels of aggression, including autoaggression, have been reported in PTSD
(6,
11,
12). However, in our study group, PTSD and cluster B personality disorders, not aggression, predicted attempter status. It may be that the relationships among aggression, cluster B personality disorders, and PTSD obscure the effect of aggression on suicidal acts.
A third of those who report childhood abuse or neglect develop PTSD
(13), and the presence of childhood abuse doubles the odds of developing major depressive episode
(14). In our group of depressed patients, 41% reported abuse during childhood, although not all of these patients developed PTSD. Frequency of childhood abuse was similar in the groups of depressed patients with and without PTSD, and abuse history did not predict suicide attempter status.
In depressed youth, PTSD is reportedly more prevalent if there is a history of sexual abuse, but suicide attempts and depression severity are not influenced by abuse history
(15). Further studies may clarify how childhood abuse is related to the development of major depressive episode, cluster B personality disorders, and PTSD, and whether it affects rates of suicidal behavior by predisposing individuals to these disorders.
The higher prevalence of PTSD in women and their greater risk for suicidal acts may explain the preponderance of women in the group with major depressive episode plus PTSD, which had more suicide attempters. However, the regression models did not find sex to be a predictor of attempter status. Whether women are exposed to more traumata or are biologically vulnerable to developing PTSD after trauma are important considerations, since more women than men in our group of inpatients reported abuse in childhood and developed PTSD.
Retrospective data in this small group of patients cannot elucidate the temporal relationship between onset of PTSD and suicidal behavior. In addition, only certain types of trauma and severity of PTSD may influence the risk for suicidal behavior (8), and our study did not evaluate trauma severity. Nevertheless, the greater risk of suicide attempts in patients with PTSD plus major depressive episode underscores the need to assess depressed patients for PTSD to ascertain accurate risk for suicidal acts.