A growing literature supports the presence of cerebellar vermal abnormalities in patients with schizophrenia. In the majority of earlier studies, the area of the cerebellar vermis was measured only in the midsagittal plane
(1–
6). However, there have been several MRI volumetric studies of the vermis in schizophrenia (e.g., references
7,
8), and the results have been controversial, with increased
(7), decreased
(4,
9), or unchanged vermal volume reported in patients with schizophrenia relative to healthy subjects
(8). The more recent studies have reported decreased volume of the cerebellar vermis in schizophrenia (e.g., references
10,
11). A previous study from our group showed that the volume of the posterior superior vermis was reduced in men with chronic schizophrenia
(12). In none of the aforementioned studies were volumes of the vermian subregions measured separately in women with schizophrenia. To test the hypothesis that the volume of the vermis is reduced in both male and female patients with schizophrenia, we used magnetic resonance imaging (MRI) to measure and compare volumes of vermian subregions in men and women with schizophrenia and healthy men and women.
Method
The protocol was approved by the Institutional Review Board at the Karolinska Hospital, Stockholm. All subjects gave written informed consent.
Subject Characteristics
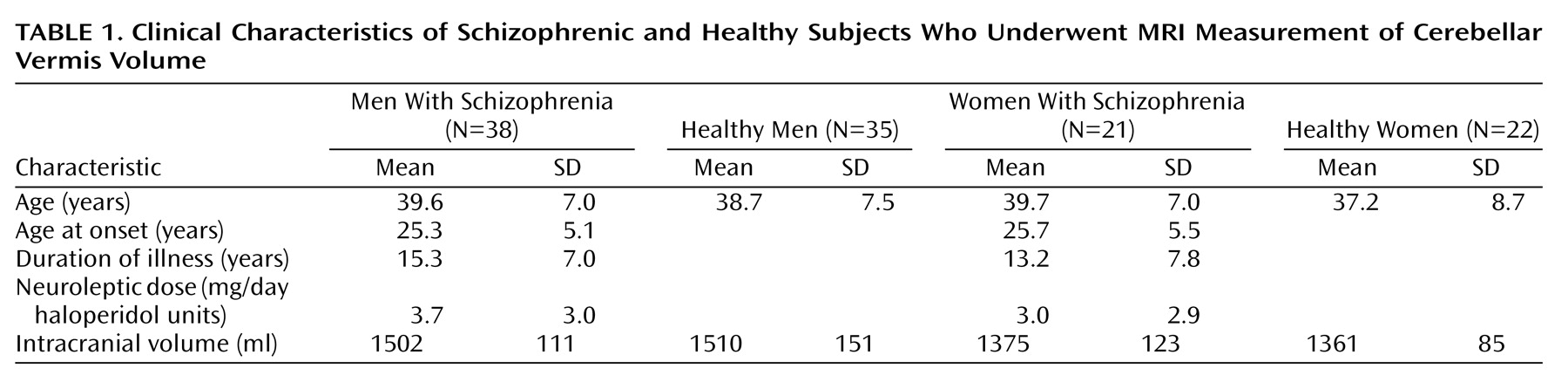
Fifty-nine patients (38 men and 21 women) with chronic schizophrenia according to DSM-IV criteria and 57 healthy volunteers (35 men and 22 women), all Caucasians, were included in this study (
Table 1). All subjects lived within the area of northern Stockholm. They were recruited at the Karolinska Hospital Department of Clinical Neuroscience, where they were investigated between August 1999 and April 2002. At the time of the investigation, 37 of the male and 19 of the female patients were receiving antipsychotic medication. Dose of current neuroleptic treatment was converted into haloperidol units
(13). All subjects were found to be healthy according to physical examination and blood and urinary tests. All subjects underwent a psychiatric interview (Structured Clinical Interview for DSM-III-R—Non-Patient Version)
(14) to confirm schizophrenia in the patients and a lack of mental disorder in the comparison subjects. The interview was conducted by an experienced psychiatrist well trained in the administration of this instrument. Exclusion criteria for the healthy volunteers were current or past treatment for a psychiatric disorder or any history of alcohol or drug addiction, head trauma with loss of consciousness for more than 5 minutes, or severe somatic disorder.
Magnetic Resonance Scans
The subjects were examined with a 1.5-Tesla GE Signa (Milwaukee) system at the MR Research Center, Karolinska Hospital, Stockholm. T1-weighted images, using a spoiled gradient/recall acquisition in the steady state sequence, were acquired with the following parameters: 1.5-mm coronal slices, no gap, flip angle=35°, TR=24 msec, TE=6.0 msec, number of excitations=2, field of view=24 cm, acquisition matrix=256×192. T2-weighted images were acquired with the following parameters: 2.0-mm coronal slices, no gap, TE=84 msec, TR=6000 msec, number of excitations=2, field of view=24 cm, acquisition matrix=256×192. From visual inspection, all scans were judged to be excellent without any obvious motion artifact. We rated the scan according to motion artifact and did not find a difference between patients and comparison subjects. All scans were found to lack gross clinical pathology as evaluated by a neuroradiologist. The quantitative analysis was performed blind to subject diagnosis and gender until the final statistical analysis.
Automated Segmentation
MRI data analysis was performed with BRAINS software
(15,
16). Detailed information about the segmentation procedure and evaluation of validity has been described by Harris et al.
(17). Reproducibility and reliability of the segmentation procedure have also been ascertained previously
(17,
18).
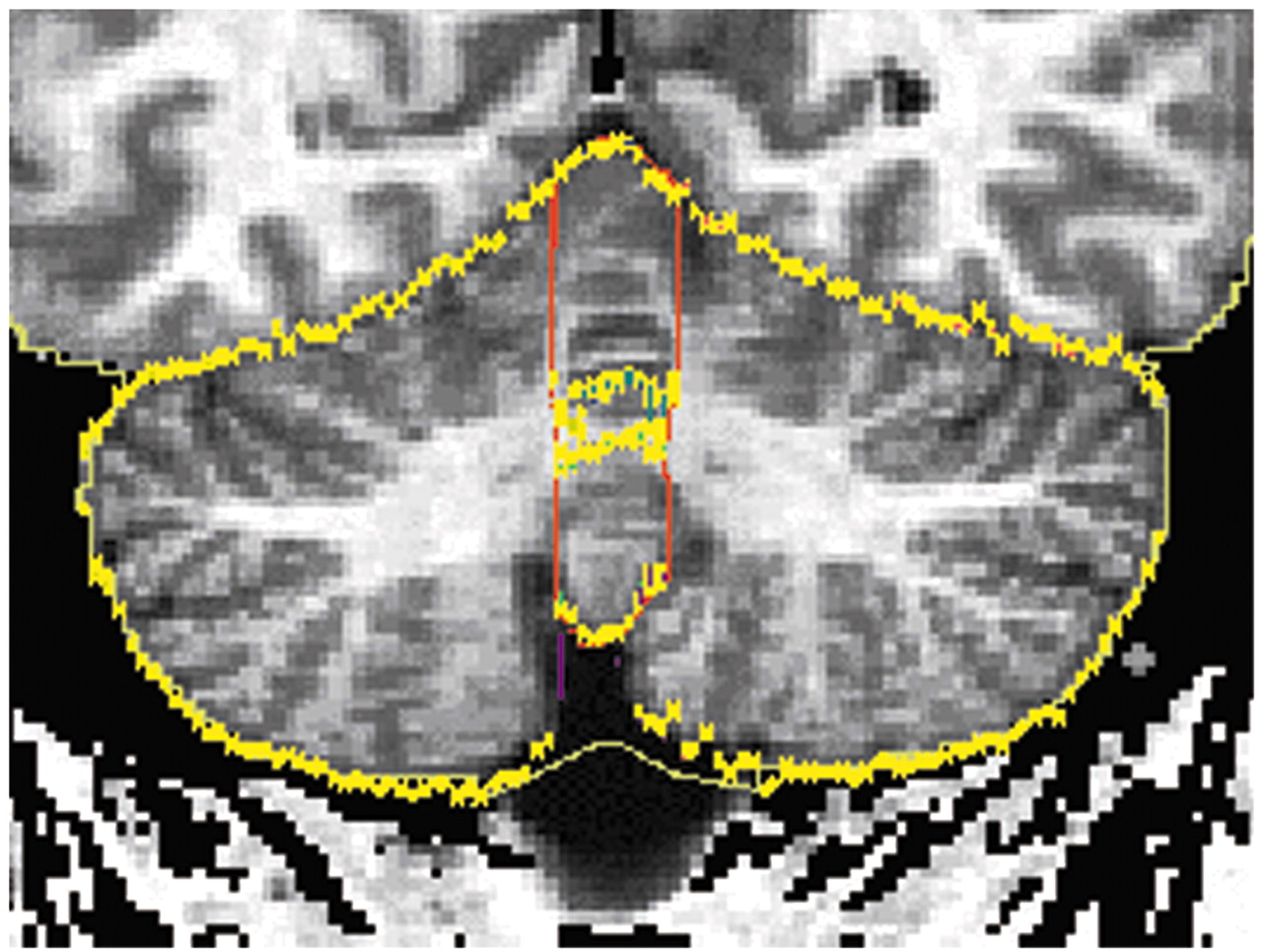
Tracing of Cerebellar Structures
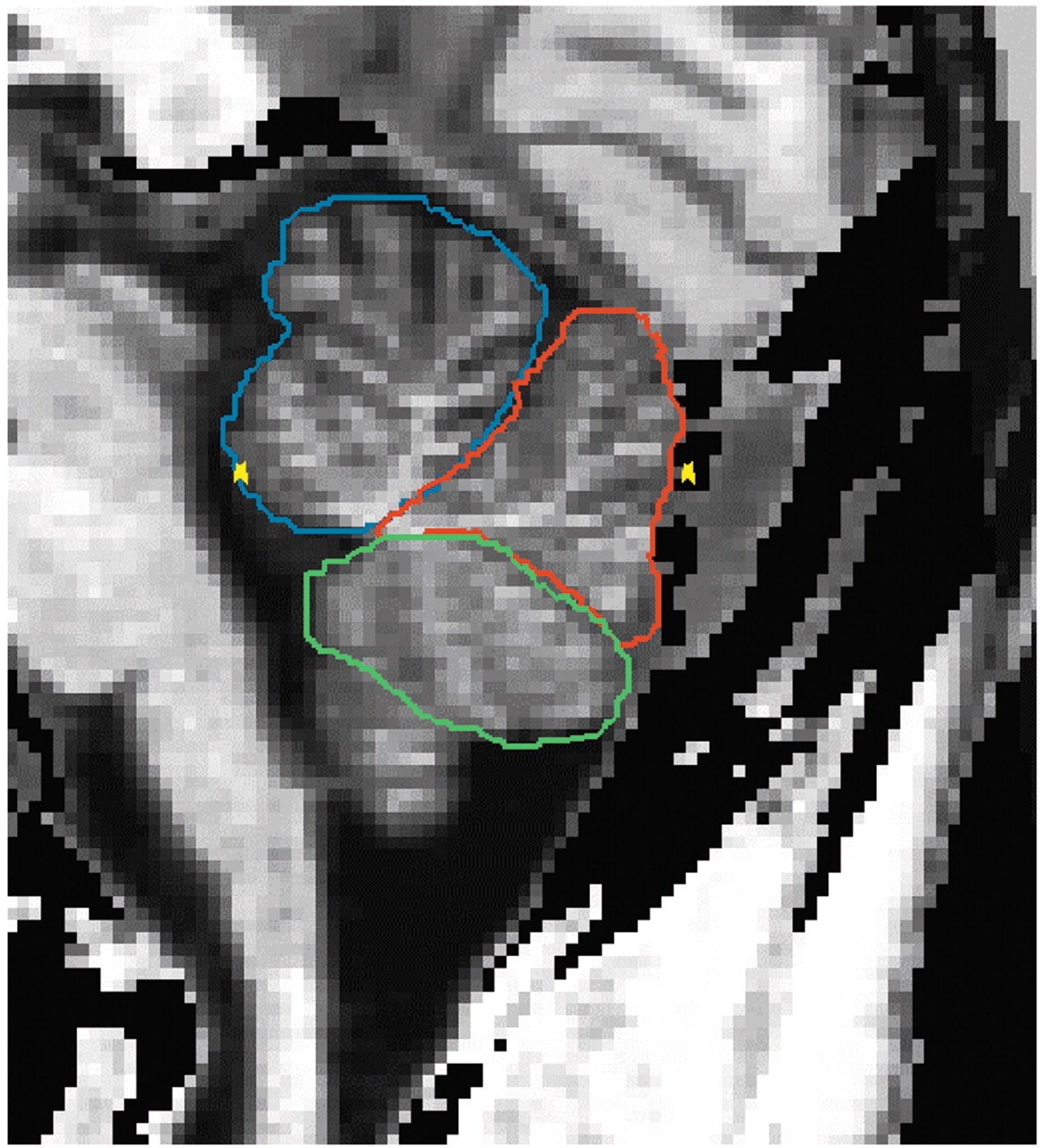
The detailed delineation of the cerebellar structures was described in the previous report
(12). The cerebellar vermis was manually parcellated into anterior vermis (lobules I–V), posterior superior vermis (lobules VI–VII), and posterior inferior vermis (lobules VIII–X) in sagittal planes on the segmented images (
Figure 1). The lateral extent of the vermis was determined in the following way. The vermian subregions were delineated from the sagittal slice in which the vermian subregions appeared and until the slice where the anterior vermis, posterior superior vermis, or posterior inferior vermis disappeared. The outer contour of the total vermis on a coronal projection is shown in
Figure 2.
Cerebellar hemispheres and cerebellar tonsils were traced manually on all sagittal slices. The volume estimate of the cerebellar hemispheres included the cerebellar hemispheres and the tonsils but not the vermis.
Statistical Analysis
Ten scans were randomly selected and evaluated blindly for inter- and intraoperator reliability. Intraclass correlation coefficients
(19) were used to establish reliability to measure volumes of the cerebellar hemispheres, anterior vermis, posterior superior vermis, and posterior inferior vermis.
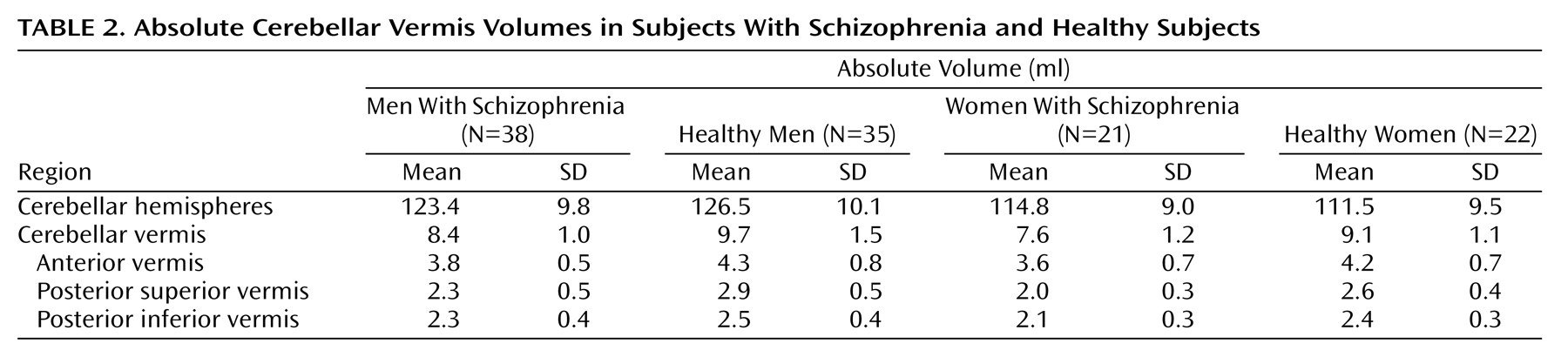
Absolute volume of cerebellar vermis was the volume of anterior vermis, posterior superior vermis, and posterior inferior vermis added together. Absolute volumes of cerebellar hemispheres, anterior vermis, posterior superior vermis, and posterior inferior vermis were independent factors. In the first analysis, we assessed diagnostic difference in absolute volumes of cerebellar hemispheres, anterior vermis, posterior superior vermis, and posterior inferior vermis by using the two-way multivariate analysis of variance (MANOVA), which included diagnosis, gender, and the diagnosis-by-gender interaction.
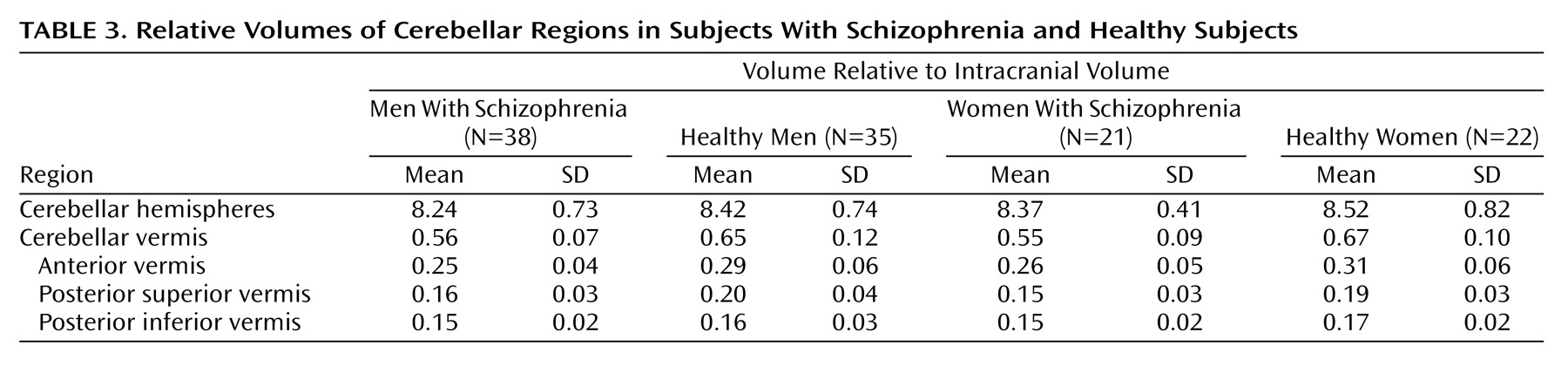
In the final analysis, the intracranial volume was used to correct for individual differences in head size. We assessed diagnostic differences for relative volumes (ratio of volume of interest to intracranial volume) of cerebellar subregions by using the two-way analysis of variance (ANOVA) model, which included diagnosis, gender, and the diagnosis-by-gender interaction. Differences were considered to be statistically significant if p<0.01 (i.e., 0.05/five regions of interest). Spearman’s correlation was used to test the correlation between volume measures and current dose of medication converted into haloperidol units or age or duration of illness in the patient group.
Discussion
In the present material, both men and women with schizophrenia had significantly smaller relative volumes of the total vermis and the three subregions (anterior vermis, posterior superior vermis, and posterior inferior vermis) compared with healthy subjects. When we studied the absolute volumes, schizophrenic subjects had significantly smaller cerebellar subregions compared with healthy subjects, and female subjects had significantly smaller cerebellar subregions compared with male subjects. There were no significant correlations between current neuroleptic dosage and volumes of cerebellar subregions.
We previously reported that the volume of the posterior superior vermis was selectively reduced within the cerebellum of male subjects with schizophrenia. In the current study, with a larger number of subjects of both genders, we demonstrated that the volumes of all the vermis subregions are reduced and that the volume reduction was most prominent for the posterior superior vermis among the vermian subregions.
Volume reduction of the total vermis was found in 20 male subjects with schizophrenia
(11). In another MRI study, Loeber et al.
(10) described volume reduction of inferior vermis and total vermis in schizophrenic patients (15 men and four women) relative to the same number of healthy subjects. In this study, we found relative volume reduction of all the vermian subregions and total vermis within the cerebellum in female as well as male subjects with chronic schizophrenia.
In other MRI studies, structural changes of the cerebellar hemispheres were reported for patients with schizophrenia
(7,
20,
21). Volume changes of the cerebellar hemispheres in schizophrenia were not found in another study, and this was also the case for the present results
(4,
22). DeLisi et al.
(23) found that the cerebellar hemispheric volumes become smaller over time in male and female subjects with schizophrenia relative to healthy subjects.
In conclusion, the result of the present study confirmed the hypothesis that within the cerebellum, the vermis volume is selectively reduced in male and female subjects with chronic schizophrenia. Since the volume measures were not correlated with neuroleptic dose, age of patients, or duration of disease, it seems possible that the vermian changes represent a significant feature of the pathophysiology in at least some patients with schizophrenia. Longitudinal studies are necessary to determine whether there is also a progressive change in the vermis.