There are more than half a million deaths by homicide each year; homicide is the sixth highest cause of mortality worldwide in those 20–44 years old
(1). Uncertainty exists regarding the association between major mental disorders and homicide; twofold differences in rates of psychotic disorders have been reported
(2–
4), and only one study
(5) examined prevalence rates apart from psychosis. To clarify prevalence rates, we investigated 2,005 homicide offenders over 14 years in Sweden; these subjects represent a study group that is more than twice the size of any previous study group.
Method
In Sweden, all residents are given a unique 12-digit identification number. High-quality national registers for crime, hospital discharge diagnoses, and forensic psychiatric evaluations can be linked on the basis of this identification number. The crime register identified 2,005 homicide offenders (convictions for murder, manslaughter, attempted murder, and attempted manslaughter) from January 1, 1988, to December 31, 2001. The proportion of homicides leading to conviction in Sweden is approximately 70%. The Swedish legal system has no plea bargaining, so individuals who are deemed legally insane or mentally disordered at the time of the offense and those who have their convictions commuted for other reasons are convicted of murder or manslaughter, although sentencing may vary from imprisonment to treatment in a secure hospital.
Psychiatric information was gathered from two comprehensive national registers that use standardized diagnostic criteria: the forensic psychiatric evaluation database and the hospital discharge register. Forensic psychiatric evaluations are ordered by all courts before sentencing to establish whether a defendant was legally insane at the time of the offense. If so, the defendant is not imprisoned but transferred to a hospital for treatment.
There are two types of forensic psychiatric evaluations: minor and major. The minor forensic psychiatric evaluation is an hour-long interview with a specialist psychiatrist who reviews medical and police records. The minor forensic psychiatric evaluation is typically used to screen for the need for a major forensic psychiatric evaluation. A major forensic psychiatric evaluation involves a multidisciplinary assessment by a forensic psychiatrist, clinical psychologist, social worker, and nursing staff in one of four specialized hospitals for up to 4 weeks. Because a major forensic psychiatric evaluation is usually required for the court to send an individual to a hospital, in some cases the court orders a major forensic psychiatric evaluation without a minor forensic psychiatric evaluation.
The hospital discharge register includes standardized discharge diagnoses for all psychiatric inpatients. Research has demonstrated the diagnostic validity of this register (6). In both the hospital discharge register and forensic psychiatric evaluation registers, ICD-9 was the diagnostic standard in 1988–1996. Starting in 1997, forensic psychiatric evaluations have used DSM-IV and the hospital discharge register shifted to ICD-10.
Principal diagnoses for homicide offenders reflected a hierarchy of diagnostic validity. We assumed that the major forensic psychiatric evaluations provided the highest quality psychiatric information, followed by minor forensic psychiatric evaluations, and, finally, the hospital discharge register. We calculated secondary diagnoses of personality and substance use disorders only in major forensic psychiatric evaluations. Thus, we first linked the personal identification number of each homicide offender to the major forensic psychiatric evaluation register. Of the 2,005 homicide offenders, 1,100 (55%) had a major forensic psychiatric evaluation. The identification numbers of the remaining 905 homicide offenders were linked to the minor forensic psychiatric evaluation database, providing information on a further 271 individuals (14%). Of the 271 offenders given minor forensic psychiatric evaluations, 230 (85%) received no diagnosis or one of substance use. The remaining 634 offenders were linked to the hospital discharge register, which provided information on a further 254 individuals (13%). Overall, information from standardized psychiatric assessments was gathered for 1,625 individuals (81%).
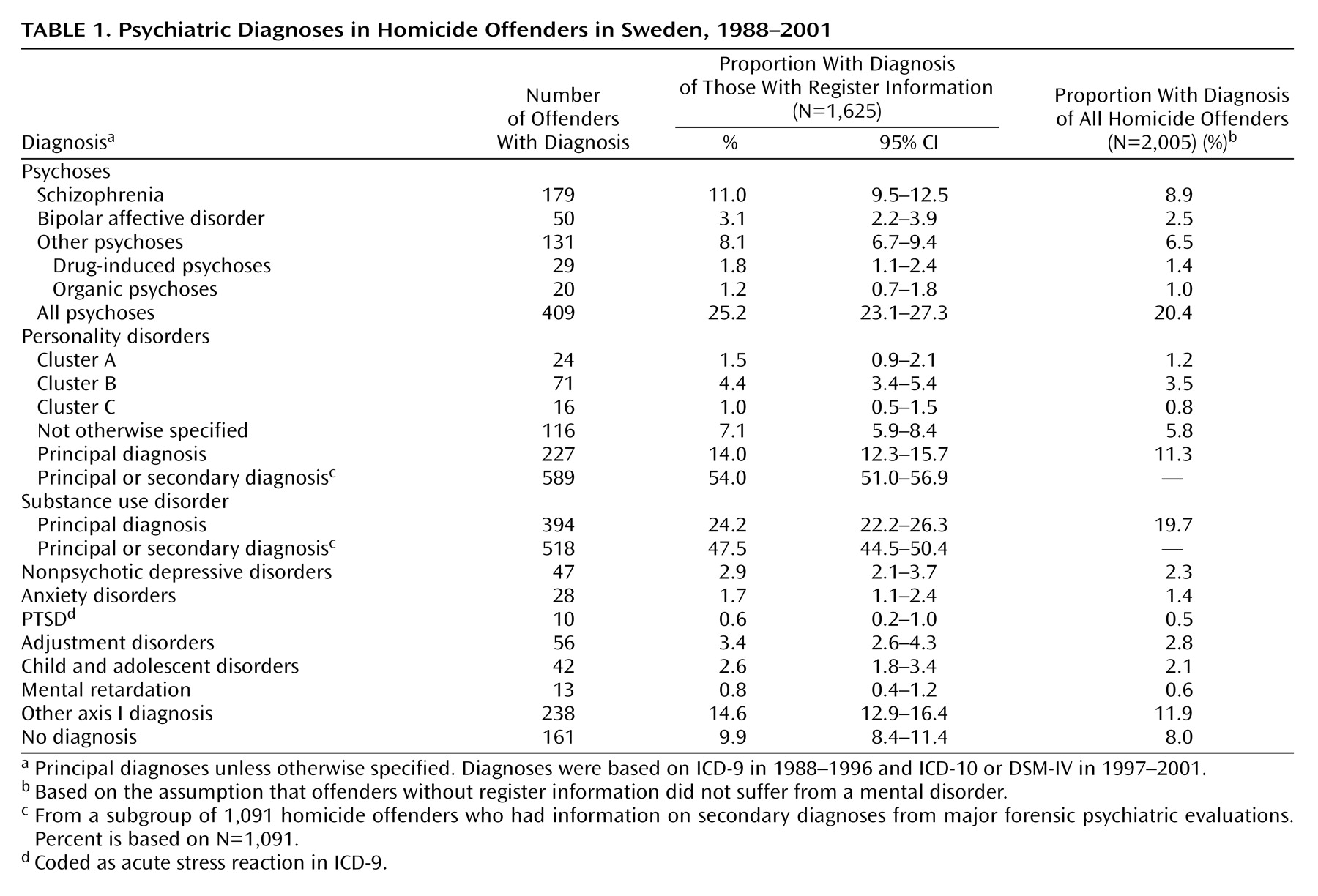
Prevalence rates are reported in
Table 1. Two proportions for the rate of mental disorders are provided. The first is based on the 1,625 individuals with standardized assessments. For these offenders, we calculated 95% confidence intervals, estimated as mean plus or minus (1.96*standard error), where the standard error=the square root of (p[1–p]/N). The second is based on all 2,005 homicide offenders. The criterion for statistical significance for comparisons between subgroups with and without diagnostic information was p<0.05 (two-tailed).
Results
The database identified 2,005 homicide offenders. Their ages ranged from 15 to 90 years (mean=30.0, SD=11.7, median=31.0); 166 (8.3%) were women, and 1,323 (66%) were Swedish citizens. There were differences in age, gender, and citizenship between offenders for whom diagnostic information was or was not available: those without diagnostic information were younger (mean age=30.5 versus 33.6) (t=–4.7, p<0.001), included a smaller proportion of women (5.3% [N=20] versus 9.0% [N=360]) (χ2=5.8, df=1, p=0.016), and included fewer Swedish citizens (16.7% [N=203] versus 22.3% [N=177]) (χ2=9.8, df=1, p=0.02).
Over 90% of homicide offenders had a mental disorder according to ICD-9, ICD-10, or DSM-IV (
Table 1). Assuming that individuals without diagnostic information in any register did not have a mental disorder, we found that the prevalence of psychotic disorders was 20%, including 9% with schizophrenia. Twenty-four percent of the offenders with register information had substance use as principal diagnosis, and 14% had a principal diagnosis of personality disorder. In the subgroup of offenders who received major forensic psychiatric evaluations where secondary diagnoses were investigated, the rate of any substance use disorder was 47% and any personality disorder was 54% (
Table 1) (any cluster A 6% [N=64], cluster B 17% [N=185], cluster C 1% [N=14], personality disorder not otherwise specified 24% [N=261]).
Discussion
To our knowledge, this is the largest study to date of mental disorders in homicide offenders. We found that over 90% had a psychiatric diagnosis. One in five suffered from a psychotic illness, and about half had a substance use or personality disorder. A weakness of the study is that it is based on retrospective data, which did not use standardized diagnostic instruments. However, homicide does not lend itself to a prospective design because the outcome is so rare.
The rates of psychotic illnesses found here are double those found in other studies. Shaw et al.
(2) examined psychiatric court reports in 500 homicide offenders in England and Wales, representing 70% of the homicide convictions in the study period. These investigators found that 6% of these offenders had schizophrenia and 44% had any lifetime mental disorder but did not report other specific diagnoses. Eronen et al.
(5) investigated 693 Finnish homicide offenders, representing 70% of all homicides, and estimated that 6% had schizophrenia, 2% suffered from other psychoses, none had manic disorders, and 33% had a personality disorder. In contrast, we estimated that 9% of homicide offenders had schizophrenia and 11% had other psychotic illnesses.
The baseline rate of psychosis in Sweden is not higher than in other countries
(7), so the differences between our findings and those of Shaw et al. and Eronen et al. might have two explanations. First, we obtained psychiatric diagnoses on 81% of homicide offenders, a higher proportion than previous studies, by collecting information from both forensic evaluations and hospital admissions. Second, the diagnostic quality of this study is higher than those based solely on court reports; research has shown that cases of mental disorder are missed at the court stage
(8). However, our study might have underestimated the true rates of mental illness, because 8%–16% of homicide offenders in Scandinavia commit suicide at the time of their offense
(9).
This study found that one in two homicide offenders had a substance use disorder or a personality disorder, primarily a cluster B disorder. Although these rates are not different from the rates in general prison populations, they suggest that comorbidity is a significant treatment challenge for this group of offenders.
Sweden’s homicide rate of around 19 homicide victims per million population is similar to the European Union average rate of 17 and three times lower than the rate in the United States
(10). In countries with more liberal gun laws, the proportion of mentally disordered homicide offenders may be different. Nevertheless, this study adds to the evidence that careful psychiatric evaluation is necessary for homicide offenders. Whether treatment has a preventive role remains an important research question.